Melkersson-Rosenthal syndrome is a rare neuro-mucocutaneous disease with a chronic intermittent course, characterized by a classic triad of orofacial swelling, fissured tongue (lingua plicata) and facial paralysis. The authors describe the case of an oligosymptomatic variant (lip and tongue involvement) with childhood onset, whose diagnosis was only established at the age of 19 years. The syndrome's pathophysiology is unclear and the treatment is challenging; corticosteroid therapy is the mainstay of treatment and is associated with clinical and histological improvement.
Melkersson-Rosenthal syndrome (MRS) is a rare neuro-mucocutaneous disorder with a recurrent and progressive course, characterized by the triad of lip swelling (cheilitis granulomatosa or Miescher cheilitis), fissured tongue (lingua plicata or scrotal tongue) and facial paralysis. However, oligosymptomatic and monosymptomatic forms are the most common clinical presentation.1 MRS can occur in people of any age and it affects both genders – the mean age-of-onset was 39 years (8-79 years) in a series of 75 patients1 and 14 years in another series of 44 patients,2 both with a clear female predominance.1 The diagnostic delay may exceed several decades.1,3
The underlying process is a chronic granulomatous inflammation affecting (intermittently or persistently) mucocutaneous tissues and orofacial innervation and its a etiology has not been clearly established. The observation of familial aggregation and the suggestion of a relationship with the de novo autosomal t(9;21)(p11;p11) translocation, support the hypothesis of a genetic predisposition.4,5 An association with infections6,7 and autoimmune disorders has also been described.8–10 Early histopathological changes include perivascular lymphocytic infiltration with a variable phenotype11,12 and subepidermal edema. Persistent infiltration is associated with the formation of noncaseating granulomas in the dermis, hypodermis and lamina propria.13
Recurrent unilateral or bilateral lip swelling is the most common monosymptomatic presentation.1 Noncaseating cheilitis granulomatosa (CG) belongs to the orofacial granulomatosis group and it has been suggested that they may be a subtype of Crohn's disease and precede its diagnosis by years, especially in children.14–16Lingua plicata is characterized by the development of deep grooves or fissures on the dorsal and lateral surfaces of the tongue; it is a benign condition frequently found in healthy people but it is more common in people with MRS, chronic granulomatous disease, psoriasis and Sjögren's syndrome.17,18 Recurrent facial nerve paralysis is less frequent, clinically indistinguishable from Bell's palsy and it may precede CG by years.19 MRS may also be associated with other cranial nerve palsies and dysautonomia.19,20
In a patient with persistent or recurrent orofacial oedema, the presence of at least one of the findings of idiopathic facial paralysis or lingua plicata is sufficient to make a definitive MRS diagnosis.
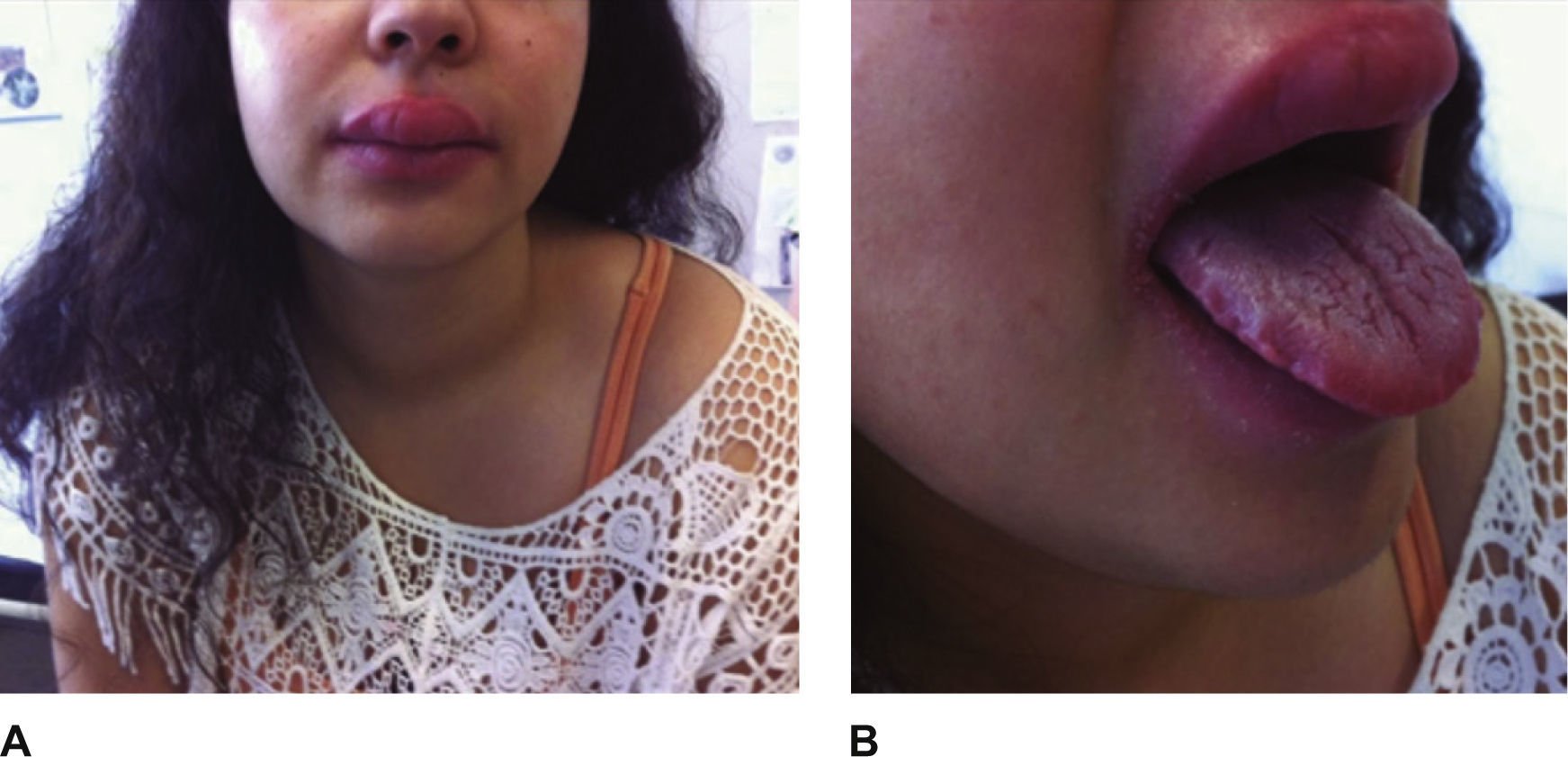
Case reportThe authors report the case of a Caucasian 19-year-old female referred to the Allergy/Immunology Department for evaluation of recurrent self-limited episodes of tense upper lip edema, with painless and non-pruriginous swelling to 2-3 times normal lip size. The symptoms started at the age of 6, with variable time intervals and no identified triggers. Since adolescence, they suffered an increase in frequency and duration. For the last two years, the patient has been experiencing 1-2 episodes per month and more recently the oedema became persistent. It was refractory to antihistamines but had a favourable res-ponse to oral steroids.
The patient also reported a change in tongue morphology, with the development of painful grooves on its surface, for the last six years. She had no symptoms of cranial neuropathy or dysautonomia. The patient had a personal history of chronic rhinitis and no relevant family history.
On physical examination, the abnormal findings were a symmetrical upper lip oedema with a firm homogeneous consistency on palpation (Fig. 1A), macroglossia, and the presence of deep fissures on the dorsal and lateral surfaces of the tongue (Fig. 1B). Skin prick tests with common regional aeroallergens, latex, and foods were performed, and they were positive for mites and grass pollen. The patch test (European standard battery) reading at 48h was negative and there were no abnormal serological findings.
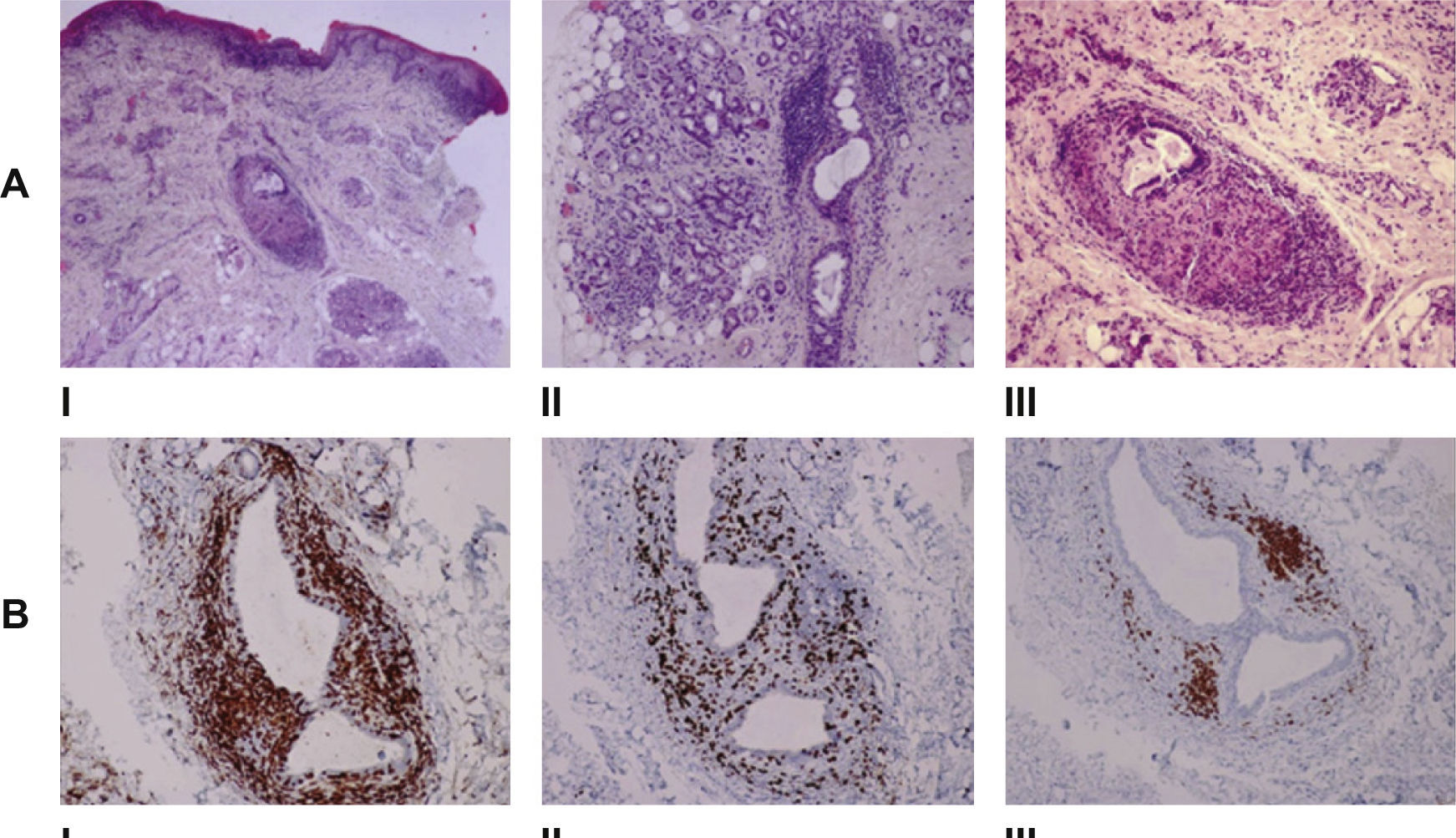
After thorough evaluation, the patient was diagnosed with an oligosymptomatic variant of MRS, presenting with recurrent orofacial edema and lingua plicata. She was referred to a specialist in Oral Medicine that performed an incisional biopsy of the upper lip. Histopathological examination revealed a labial mucosa with perivascular mononuclear inflammatory infiltration, fibrosis and an increase in neurovascular branching. There were noncaseating epithelioid cell granulomas (Fig. 2-I II) and multinucleated Langhans giant cells. The histochemical study with PAS, PAS-D and Ziehl Neelsen was negative. Immunohistochemical studies showed a predominance of T-cells in the multiple granulomas’ surrounding area, the majority were CD4+ (75%), the remaining were CD8+ (15%) and a few B-cells (10%) were also located in the multiple granulomas’ centre (Fig. 2B).
Histopathological findings in the labial mucosa. A – I. The biopsy of the swollen lip shows granulomatous chelitis characterized by perivascular lymphocytic infiltration with granuloma formation in the submucosa (haematoxylin-eosin [H&E], original magnification x 40). II. Deeper areas of the biopsy show the presence of chronic inflammatory infiltration of the lips’ salivary glands (H&E, original magnification x 100). III. High power view of the granuloma (H&E, original magnification x 100). B – Immunochemistry study. I. CD4+ cells representing 75% of T-Lymphocytes. II. CD8+ cells representing 15% of T-Lymphocytes. III. Scanty CD20+ cells (x100 immunoperoxidase with haematoxylin counterstain).
Treatment was initiated with 0.5mg/kg per day of oral deflazacort and with a favourable clinical response of the lip swelling so far, although the patient is still in the initial phase of treatment.
DiscussionMRS is a clinical syndrome with no need for histological evidence in the establishment of a diagnosis and the absence of typical findings do not exclude it.2,3 However, histopathology may help to exclude other conditions and, in our case, allowed additional characterization of the underlying inflammatory process, which may help us better understand the mechanisms of the disease. A histological exam also revealed chronic sialadenitis of a minor salivary gland, although the patient has had no symptoms suggestive of exocrine gland dysfunction and no serological changes suggestive of an autoimmune disease.
CG is the most frequent clinical manifestation in patients with MRS and poses difficulties regarding treatment. Oral or intralesional steroids remain a mainstay of CG treatment regimens and its potent anti-inflammatory activity is associated with clinical and histological improvement.21,22 Although oral doses are not well established, intralesional triamcinolone dosing varies from 10 to 20mg doses with intervals of weeks to months between injections.21,23,24 Clinical success of this approach is often temporary,21,25 but its use may be an alternative to the chronic use of oral steroids with the consequent iatrogenic effects.
Anti-inflammatory and immunomodulatory activities of some antibiotic agents may explain why they have been successfully used for treating CG. The antibiotics that have gained more recent prominence include minocycline (100mg daily) and roxithromycin (150-300mg daily); promising results have been obtained with metronidazole using doses of 750-1000mg daily.21
Infliximab, effective in the treatment of Crohn's disease, has also been reported as a promising agent for use in difficult-to-treat CG, in infusion doses ranging from 3 to 5 mg/kg;13,26 methotrexate reduces the proliferation of immune cell lines and was used effectively in doses of 5-10mg given orally at weekly intervals.21,27
Surgical management is an option reserved for severe or deforming CG,28 but recurrence is frequent29 and the risk of losing normal sensation in the affected lip must be weighted.28
A good oral hygiene, avoidance of irritating foods and intermittent use of anti-inflammatory and alkaline solutions may be of benefit in cases with fissured tongue.18
We would like to thank Dr. Jorge Serafim Freitas (Serviço de Estomatologia, Centro Hospitalar São João, E.P.E.) for his collaboration in the diagnostic workup of our patient.



![Histopathological findings in the labial mucosa. A – I. The biopsy of the swollen lip shows granulomatous chelitis characterized by perivascular lymphocytic infiltration with granuloma formation in the submucosa (haematoxylin-eosin [H&E], original magnification x 40). II. Deeper areas of the biopsy show the presence of chronic inflammatory infiltration of the lips’ salivary glands (H&E, original magnification x 100). III. High power view of the granuloma (H&E, original magnification x 100). B – Immunochemistry study. I. CD4+ cells representing 75% of T-Lymphocytes. II. CD8+ cells representing 15% of T-Lymphocytes. III. Scanty CD20+ cells (x100 immunoperoxidase with haematoxylin counterstain). Histopathological findings in the labial mucosa. A – I. The biopsy of the swollen lip shows granulomatous chelitis characterized by perivascular lymphocytic infiltration with granuloma formation in the submucosa (haematoxylin-eosin [H&E], original magnification x 40). II. Deeper areas of the biopsy show the presence of chronic inflammatory infiltration of the lips’ salivary glands (H&E, original magnification x 100). III. High power view of the granuloma (H&E, original magnification x 100). B – Immunochemistry study. I. CD4+ cells representing 75% of T-Lymphocytes. II. CD8+ cells representing 15% of T-Lymphocytes. III. Scanty CD20+ cells (x100 immunoperoxidase with haematoxylin counterstain).](https://static.elsevier.es/multimedia/24448664/0000000100000001/v3_201606070024/S244486641600012X/v3_201606070024/en/main.assets/thumbnail/gr2.jpeg?xkr=ue/ImdikoIMrsJoerZ+w96p5LBcBpyJTqfwgorxm+Ow=)
