This work proposes a novel approach to assess spinal curvature, by using Microsoft's Kinect™ to obtain 3D reconstructed models of subject's dorsal skin surface in different postures. This method is non-invasive, radiation-free and low-cost.
The trial tests here presented intended to evaluate the reliability of this approach, by assessing the tendency of 98 volunteers to present scoliosis. The shoulder height difference was calculated for each subject's scan, by quantifying the angular slope of a line crossing both scapulae.
The volunteers’ average age was 24.7 years. Results showed that 68.37% of the volunteers revealed differences higher than 1° between the shoulders, having that their record in what concerns to loads and lesions proved to increase the angular slope. This initial approach shall establish the grounds for assessing spinal posture in pre-clinical or industrial ergonomics scans. Further studies shall include comparison versus traditional imaging methods and experienced clinical evaluation.
Low back pain, where suboptimal sagittal alignment is frequently compromised, was found to be among the top ten causes of disability in a worldwide study of global burden of disease.1,2 Clinically, spinal posture positioning and training is an important aspect of musculoskeletal assessment and treatment of low back pain.3 Spinal posture is defined as a positional relationship between the different spinal segments with respect to one another and with respect to gravity.4
Despite its importance, there is little consensus on what are the “ideal”, “correct” and “incorrect” postures. The current descriptions on this matter are predominantly qualitative rather than quantitative.4,5 The lack of quantitative data on this matter arises difficulty for researchers and health practitioners to be precise when speaking about the curvature of the spine.3,6
One of the conditions that is mostly well-known to compromise spinal curvature is scoliosis, which is a deformity where one or more lateral deviations of the midline of the spine occur in the coronal plane. The lateral curvature of the spine is also associated with rotation of the vertebrae, producing a three-dimensional deformity of the spine.7–9 Basic clinical investigation of scoliosis includes complete physical and neurological examinations.10,11 This work is focused on the physical examination branch. The patient should be evaluated from behind and the examiner should be on the lookout for eventual asymmetries in shoulders, scapulae, waistline, ribs, arm distance from the trunk and head alignment relative to the pelvis.9 Examination should proceed by performing the Adam's forward bending test: the standing examined person is asked to bend forward looking down until the spine is horizontal while keeping the feet together, knees extended and arms dependent. If positive, a rib prominence in the thoracic region or a paraspinal fullness in the lumbar region displays, reflecting the effects of vertebral rotation associated with scoliosis.7,12 This test is the key procedure for the purpose of screening scoliosis through the biomechanical point of view, so it is highly pertinent for the evaluation of the spinal curvature and posture.9
Given that the clinical evaluation of posture and spinal curvature is based on surface observation, quantitative studies on these matters should focus on skin surface measurements.4,13 Previous quantitative studies at the skin surface level have often relied on the use of a technique called “Skin Surface tracking”,3,4,6 involving the acquisition of surface measurements along the spinal curvature. In order to achieve such measurements, markers and/or sensors are placed on the skin of the patient, overlying spinal processes. It must be highlighted that such procedures are unable to provide data for a 3D reconstruction of the skin surface.14 Therefore, measurements are limited to the points where markers/sensors are positioned, rendering impossible a global or topological assessment of spinal curvature.
The method here presented intends to overcome such difficulties, by using Microsoft's Kinect™ to acquire the topology of the subjects’ spine. Kinect™ is able to acquire positional data without the need for sensors, allowing for 3D reconstruction of the dorsal skin surface using appropriate software.15–17 The resulting models can be used to acquire measurements by referring to relevant anatomical references. Past studies assessing Kinect's reliability in a kinematic evaluation of postural control (i.e. assessing posture during movement) suggested that this device is valid for the assessment of postural control.15,16 In addition, the images generated by the Kinect's sensors are valuable input for full 3D image reconstruction, following similar protocols to the ones designed by18,19 and subsequent specific simulation of the subject's spine through the Finite Element Method (FEM), accordingly to the work of.20
The key goal for the present work is to evaluate the reliability of Microsoft Kinect™ as a tool to perform an initial assessment of spinal posture. To this end, a quantitative comparison of simplified skin surface scans obtained from the 98 volunteers is held, considering two postures classically evaluated during a clinical assessment, namely the habitual standing posture and Adam's forward bending test.
Materials and methodsA convenience sample of 103 adult students or researchers was recruited from the Life and Health Sciences Research Institute of the University of Minho (51 females and 52 males). 3 females and 2 males were excluded, due to inadequate acquisition of the scans. Such exclusions were caused solely by acquisition problems and not by any particular condition of the participants. The main reasons for scan exclusion were related to excessive time spent acquiring the same region leading to excessive face capture in the 3D mesh, which resulted in irregular surfaces and thus the isolation of contours for postural analysis was inefficient or impossible. Inadequate lighting was also a drawback for this procedure, particularly in subjects with a light skin, where excessive light reflection can impair surfaces acquisition.
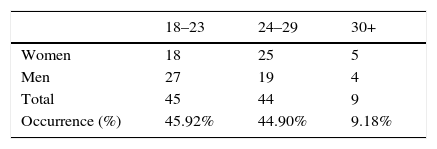
The average age of the remaining 98 volunteers was 24.7, being the range comprised between 19 and 40 years. More information on the age distribution of the volunteers is shown in Table 1. This population tends to spend a considerable part of the day sited at a desk and using a computer. Such routine is potentially a source of posture-related spinal conditions.4,21
Each participant has first signed a written informed consent form. Then, a short questionnaire about antecedents which can influence posture/curvature was held, containing 4 questions: (a) past or present history of back pain, or known spinal pathology/lesion (clinically diagnosed); (b) previous spinal treatment/surgery (clinically prescribed); (c) history of recurrent sports practice; (d) recurrent exposition to heavy loads in the past or present.22–24 The collected data was used for variable control.
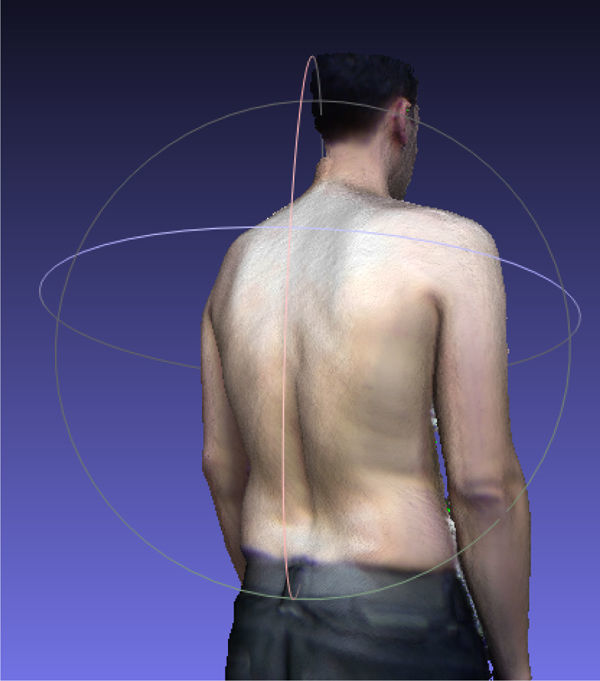
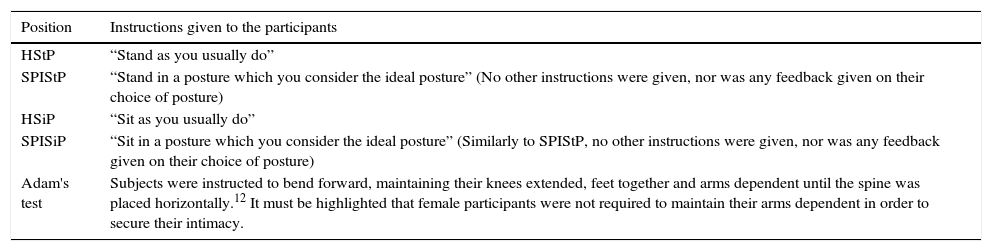
The scanning procedure focused on capturing the area of interest for studying the spinal curvature, i.e. the skin surface of the spine, scapular region and superior aspect of the sacroiliac region.25,26 The choice of the postures was based on a review of several studies examining ideal posture and subjective perception of ideal posture.6,23,27Table 2 contains the instructions given to the participants to execute the 5 predetermined postures, i.e. “Habitual standing posture” (HStP), “Subjectively perceived ideal standing posture” (SPIStP), “Habitual sitting posture” (HSiP), “Subjectively perceived ideal sitting posture” (SPISiP) and Adam's forward bending test.12Fig. 1 shows an example of a volunteer's scan while executing the HStP. For sitting postures participants sat on a stool, with their feet fully placed on the ground and knees flexed at a right angle. Along the study, female participants placed their arms against the chest, in order to secure their intimacy. Male participants were asked to place their arms along the trunk (or as parallel as possible to the legs in Adam's position).
The 5 predetermined postures and the correspondent instructions given to the participants.
| Position | Instructions given to the participants |
|---|---|
| HStP | “Stand as you usually do” |
| SPIStP | “Stand in a posture which you consider the ideal posture” (No other instructions were given, nor was any feedback given on their choice of posture) |
| HSiP | “Sit as you usually do” |
| SPISiP | “Sit in a posture which you consider the ideal posture” (Similarly to SPIStP, no other instructions were given, nor was any feedback given on their choice of posture) |
| Adam's test | Subjects were instructed to bend forward, maintaining their knees extended, feet together and arms dependent until the spine was placed horizontally.12 It must be highlighted that female participants were not required to maintain their arms dependent in order to secure their intimacy. |
Microsoft Kinect™ was used to obtain the scans for each position. This device is equipped with an infrared laser transmitter and an infrared detecting camera, allowing for the calculation of distances of objects in the environment. Together with the regular video feed obtained from a traditional camera, this allows the acquisition of data for surface reconstruction and position tracking.15–17
The software used for acquiring the scans and creating the computational model was ReconstructMe® (PROFACTOR, Austria). For visualization and captioning purposes, the software was Meshlab® (ISTI-CNR, Italy). From the different acquired positions, only two were analyzed, namely the HStP and Adam's test, due to their clinical relevance.9,12,28
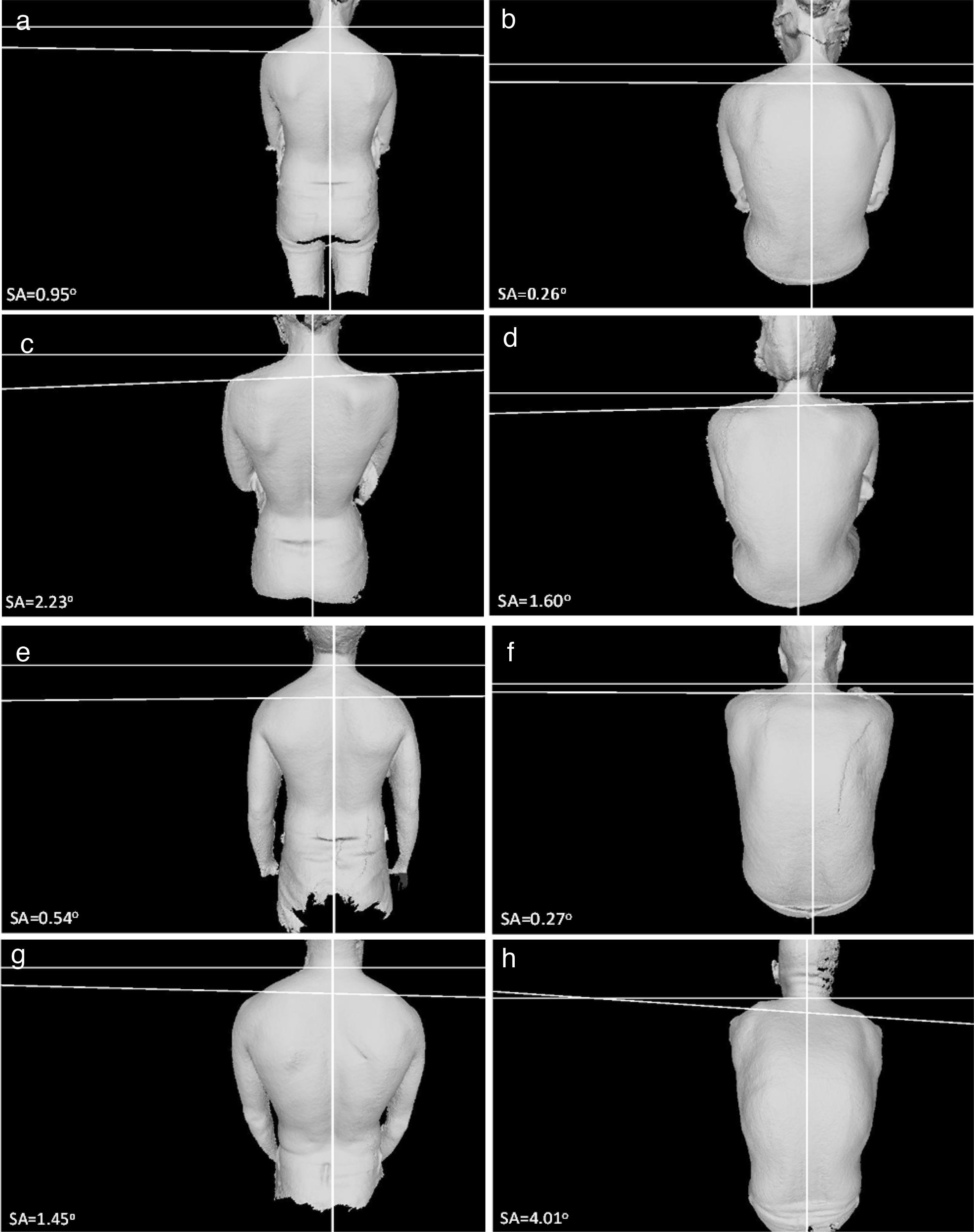
In order to evaluate the tendency of the subject to present scoliosis (or other spinal deformity), the shoulder angulation (SA) was calculated. The position of the C7 spinal process was estimated using a method of pixel-shade difference, and a vertical line intersecting it was drawn. The angle of the slope of the inter-acromial line relative to a perpendicular to the vertical line along the C7 point was measured, and this was considered the SA (Fig. 2). The calculation of the SA was obtained using a custom Matlab® (Mathworks, USA) script, having the captions as input. The position of the acromia was manually adjusted, with the aim of allowing for direct comparison between the subjects.
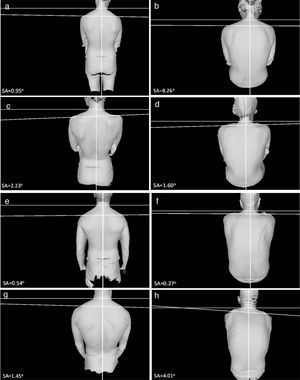
Examples of the volunteers’ captions. On the left, (a), (c), (e) and (g) show the HStP, while on the right, (b), (d), (f) and (h) show Adam's test. Participants with not relevant SA are shown in (a), (b) (female), (e) and (f) (male). Participants with SA higher than 1° are shown in (c), (d) (female), (g) and (h) (male). SA value is shown in each image.
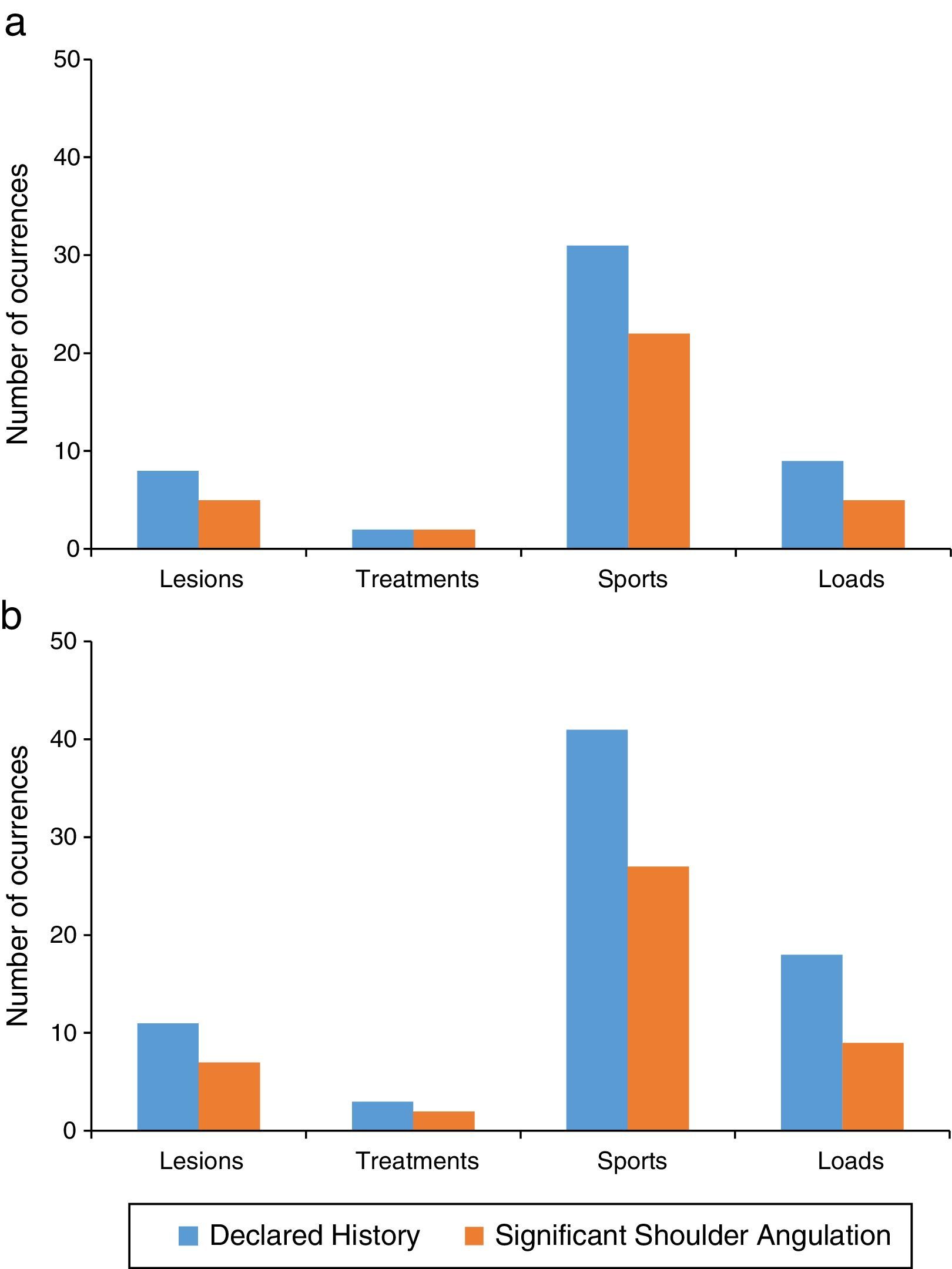
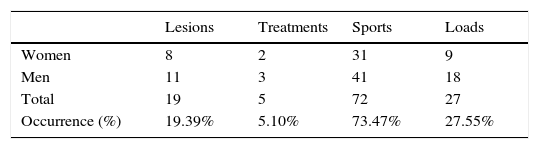
Table 3 shows the record of the history of the 98 participants with valid scans, divided by the four points of the questionnaire. 19.39% of the participants declared to have record a spinal lesion in the past, but only 5.10% have record of spinal treatment. 73.47% have practiced sports regularly and 27.55% were recurrently exposed to heavy loads.
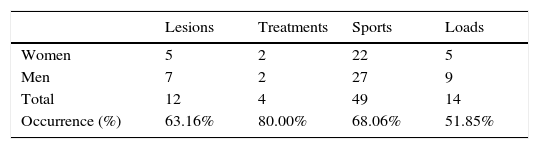
Using the procedure described in the previous section, the valid scans were characterized in terms of SA, for the two chosen positions (HStP and Adam's test). SA was only considered to be relevant for clinical evaluation if it was higher than 1°. In accordance with this premise, 37 women (77.08%) and 30 men (60.00%) have shown shoulder deviation, which corresponds to 68.37% of the participants. Fig. 2 shows examples of the 2D captions, marked with the SA calculation, while Table 4 shows the number of occurrences divided by each point of the preliminary questionnaire.
63.16% of the participants that have declared spinal lesion in the past presented relevant SA. Previous spinal treatment was flagged in 80.00% of the cases, while 68.06% was the percentage of occurrences for the athletes. Finally, 51.85% of the participants exposed to heavy load proved to have relevant SA. Apart from these results, 11 women and 2 men presented relevant SA while declaring no record of spinal lesion, sports practice or loads carrying history. This corresponds to 19.70% of the participants with relevant SA. It is also interesting to notice that only one volunteer had track of spinal treatment and actually shown irrelevant SA.
Fig. 3 presents the comparison between the participants’ history and their actual SA, divided in female and male cases, respectively. No substantial differences were found between genders.
The total SA calculations revealed that male participants presented an average SA of 1.46°, while female participants have shown a higher value of 2.22°, which results on a global average of 1.84°. The standard deviation was 1.08 for the male's group and 1.54 for the female's group. It must be highlighted that this average evaluation considered all the valid scans, i.e. including both relevant and irrelevant SA calculations.
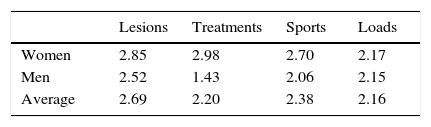
In what concerns solely to the relevant SA scores, Table 5 shows that record divided by the participants’ history and also by gender. No substantial differences are noticed between genders, except for the participants with previous spinal treatments. Male participants with this antecedent presented average SA of about half of the correspondent female participants. The group of participants with history of spinal lesions presented the highest average SA value (2.69), while the lowest average value corresponded to the group of participants with recurrent exposition to exaggerated loads.
DiscussionFor the current study, each image was positioned along a referential placed on Kinect's depth sensors. Comparison of scans required manual adjustment of the referential, which was necessary to guarantee comparable SA calculations, but which can also lead to observation errors. Future scans should adopt a standard referential, through the improvement of the Matlab® script. The common location for the origin of the referential shall be on the midpoint between superior posterior iliac spines.9 These body landmarks are easily traced and identified by a physician meaning that such a referential could be adopted for future studies.
Previous studies of postural assessment based on skin surface measurements have focused mainly on angles between lines intersecting the spine along the sagittal plane, namely spinal processes including C7, T1, T5, T10, L3 and S2.4,6,23 The current study is limited by the fact that S2's spinal process exposition was not ensured. While this limits the comparison with previous studies, it is important to note that several studies have questioned the reliability and validity of spinal process identification.28–30 These points are chosen taking in account apexes and inflection points along the spinal curvature. Cobb's angle, the gold standard for curvature assessment, is based on a similar principle.7,31,32 Therefore, the method presented in this work allowed the identification of anatomical markers and can still be improved to approach other markers.
The calculations of the SA for the 98 participants have shown that women present higher shoulder deviation than men, even if the differences may not be noteworthy. In addition, the reliability of this finding may be limited by the non-ideal conditions of Adam's test for female participants, given that they positioned the arms in front of the trunk instead of extending their arms parallel to their legs (as asked to men participants). This could induce some extra bending on the shoulders, even if it should not influence the overall SA scores. For the HStP test, the position of the arms was not considerably important, as the shoulders were on a steadier position.
The calculated SA values can be directly correlated with the participants’ history. For all the 4 points asked in the preliminary questionnaire, the percentage of relevant SA scores versus declared history was higher than 50%. It was interesting to notice that one participant had a record of spinal treatment and has shown irrelevant SA, probably meaning that the treatment was successful. 19.70% of the participants with relevant SA scores did not declare any related history, which may be interpreted as undisclosed causes for postural problems or questionnaire limitations (which may need to be improved).
73.47% of the 98 participants have declared to regularly practice sports, and amongst those, 68.06% presented relevant SA, with an average value of 2.38°. Sports practice can be beneficial to reduce spinal problems, but these numbers seem to show that that correlation is not straightforward. The relation between previous injuries and relevant SA was also disclosed, being this the point with the highest average SA (2.69°), based on the 63.16% of participants which declared to have an injury record and have actually shown relevant SA. These participants are most likely strong candidates to present a spinal posture-related condition, namely associated with scoliosis.
ConclusionsScans were successfully obtained for 98 subjects out of an initial sample of 103. This low number of exclusions means that the scanning procedure here proposed is effective, which is important for both clinical and industrial applications.
The results here presented have shown that Microsoft Kinect™ might be a valuable tool to quantitatively evaluate spinal posture, as it allows for radiation-free assessment of spinal contours. This work led to the collection of a wide sample of scans which will continue to be analyzed for this purpose. Future studies should examine the degree of correlation between SA values and Adam's test result. SA should thus be complemented by other measurements.9,33,34
The relation between the participants’ history and their tendency to develop a spinal-posture condition could be disclosed with this method, which means that the developed approach has the potential to serve as an initial evaluation of scoliosis and other positioning-related spinal problems. In the future, this procedure will be applied for 3D postural studies based on measurements along a sagittal spinal 3D contour, evaluating the extent to which subjectively perceived ideal posture differs from an ideal/neutral posture. Such knowledge would allow innovation in posture correction technology or the development of a follow-up method in the industrial environment. This procedure has demonstrated potential to be applied as a low cost radiation-free alternative to radiologic methods (X-ray or CT) for spinal curvature evaluation, along with 3D reconstruction and numerical simulation through FEM.18–20 Further research will include validation against traditional medical imaging methods.
Conflicts of interestThe authors declare no conflicts of interest.