Different surgical procedures have been described for the treatment of the recurrent anterior dislocation of the shoulder. Despite the documented success of the open procedures, some studies suggest that the arthroscopic technique leads to more favorable results. However, there still seems to be some disagreement concerning the incidence of complications, when comparing open and arthroscopic techniques.
Objective and methodsAs an attempt to clarify these doubts about the incidence of complications associated with the different techniques, this study contains a free literature review along with a retrospective case series of the patients who underwent these procedures in an University hospital in the past 10 years.
Discussion and conclusionThere are various techniques for the treatment of the recurrent dislocation of the shoulder, all of them with known success when it comes to prevention of recurrence. However, all of them are invariably associated with high complication rates.
Despite being associated with a slightly higher re-operation rate, in the literature, the arthroscopic technique was found to have an overall lower rate of complications when compared to the open procedures. Centro Hospitalar São João (CHSJ) presented a higher rate of screw related complications and revision surgery than the literature. However, concerning other complications and when assessing the procedures individually, no tendency was verified. One can therefore conclude that, despite being scarce, the Centro Hospitalar São João CHSJ data roughly overlap the literature.
Different surgical procedures have been described for treatment of the recurrent anterior dislocation of the shoulder.1 Currently, efforts are being made to determine parameters that can be widely used to decide what procedure to perform. Balg and Boileau2 have created an instability score (ISIS) to determine pre-operative risk factors in patients with recurrent instability. This score intends to help the surgeon decide whether to perform a soft tissue procedure or a bone graft procedure. So, in patients with high recurrence risk, coracoid transfer procedures that place the coracoid process on the anteroinferior border of the glenoid cavity are an alternative to the soft tissue procedures (Bankart). The first coracoid transfer procedure was described by Latarjet3 in 1954 and by Helfet (who named the procedure after Bristow) in 1958, having suffered some modifications since then.
The difference between both (Latarjet and Bristow) lies in the coracoid graft position. The Bristow procedure places the longer axis of the graft perpendicularly,4 whereas the Latarjet procedure places it parallel to the glenoid cavity.5 In both, the final effect is a bone block that reinforces the anteroinferior border of the glenoid cavity and a stabilizing sling effect achieved by the transfer of the coracoid and conjoint tendon through the subscapular muscle.6
Despite the documented success of the open procedures, some studies suggested that the arthroscopic technique is associated with a cosmetically more favorable result, as well as with a lower post-operative morbidity and a faster recovery. And, as far as the procedure is concerned, studies claim that this minimally invasive technique allows a more accurate positioning of the graft, theoretically lowering the complications associated with its dislocation.7 However, there still seems to be some disagreement concerning the incidence of complications, when comparing open and arthroscopic techniques.8
This study focuses exclusively on coracoid transfer procedures, which, despite being effective on patients with a high risk of recurrence, are also associated with certain complications that must be taken into consideration before, during and after the surgery.
Thus, as an attempt to clarify these doubts about the incidence of complications associated with the different techniques, this study contains a free literature review alongside a retrospective case series of the patients who underwent these procedures in an university hospital in the past 10 years.
MethodsA literature review was performed, using the PubMed database. The keywords were Complications; Bristow; Latarjet; Open; Coracoid Transfer; Bone-block; Arthroscopic; Shoulder; Glenohumeral; Instability; Dislocation.
Complication was defined as an adverse event or morbidity caused by the surgery and the complications included in this study were recurrent instability (dislocation, subluxation and positive apprehension test), pseudarthrosis, graft dislocation, graft fracture, osteolysis/graft reabsorption, arthrosis, screw related complications (loose, migration, fracture), pain, hematoma, infection (deep or superficial), neuromuscular/vascular complications, revision surgery and functional restrictions.
The inclusion criteria were: English or Portuguese language studies published after 2005; Case series with human participants; studies reporting the complications of the original or modifications of the Bristow/Latarjet procedures for the treatment of the recurrent dislocation of the shoulder.
The exclusion criteria were: studies on any language other than Portuguese or English; studies published before 2005; studies in animals; level of evidence V, opinion articles, anatomic studies, biomechanical studies, or studies referring only to the surgical or image techniques. Case reports, abstract only publications and revision articles with no original data were also excluded, as well as studies reporting only the outcomes of revision surgeries and isolated soft tissue stabilization procedures (Bankart). The studies reporting the results of more than one technique were only included if a clear distinction of the outcomes of each procedure was possible.
The title, abstract or both of each article were reviewed. The full texts were reviewed when inclusion was anticipated, when there was no abstract available or when a decision regarding inclusion or exclusion could not be made from the title and/or abstract alone. The references of the included studies were also reviewed for potential inclusion, for any additional articles not identified through the database search. A total of 19 articles were included,1,5,8–24 the data were organized and descriptive statistics were calculated and analyzed.
A retrospective review of the patients submitted to coracoid transfer procedures in the Orthopedics and Traumatology department of the Centro Hospitalar São João (CHSJ), an University hospital in Porto was also performed. The data were extracted from computer records. The inclusion criteria were: surgeries performed between January 2006 and December 2015. The exclusion criteria were: soft tissue stabilization procedures and revision surgeries.
From the 69 patients submitted to stabilization procedures for the recurrent dislocation of the shoulder, only 34 were submitted to coracoid transfer procedures. The others underwent soft tissue procedures. Thus, 34 patients were included and such as in the literature review, the data were organized and descriptive statistics were calculated and analyzed.
In the statistical analysis, the chi-square test was used to evaluate the differences in the incidence of complications among the different procedures. When the sample was too small, the Fisher's Exact test was used. A similar way was used to assess the qualitative differences of the functional scores results and the t student test was used to analyze continuous variables. p<0.05 was deemed statistically significant.
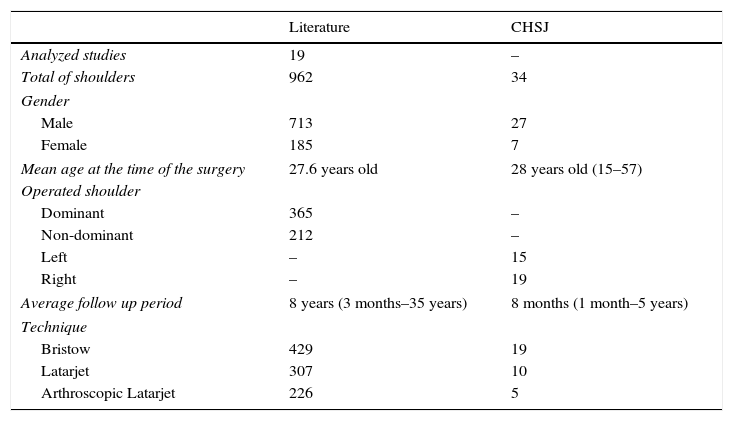
ResultsLiterature reviewIn the literature review, a total of 898 patients (962 operated shoulders) were included, of which 713 (79%) were male and 185 (21%) were female.
The mean age at the time of the procedure was 27.6 years old. The dominant side was involved in 365 (63%) cases whereas the non-dominant side was involved in 212 (37%). The average follow-up period was 8 years (ranging from 3 months to 35 years) (Table 1). From all the operated shoulders, 429 underwent the Bristow procedure, 307 the Latarjet procedure and 226 the arthroscopic Latarjet procedure (Table 1). The data from each included study is discriminated in Table 2.
General data from the literature and CHSJ, the University hospital. Since many articles do not refer to some of the variables, the total number may not coincide in all of them. The data from each included study is discriminated in Table 2.
| Literature | CHSJ | |
|---|---|---|
| Analyzed studies | 19 | – |
| Total of shoulders | 962 | 34 |
| Gender | ||
| Male | 713 | 27 |
| Female | 185 | 7 |
| Mean age at the time of the surgery | 27.6 years old | 28 years old (15–57) |
| Operated shoulder | ||
| Dominant | 365 | – |
| Non-dominant | 212 | – |
| Left | – | 15 |
| Right | – | 19 |
| Average follow up period | 8 years (3 months–35 years) | 8 months (1 month–5 years) |
| Technique | ||
| Bristow | 429 | 19 |
| Latarjet | 307 | 10 |
| Arthroscopic Latarjet | 226 | 5 |
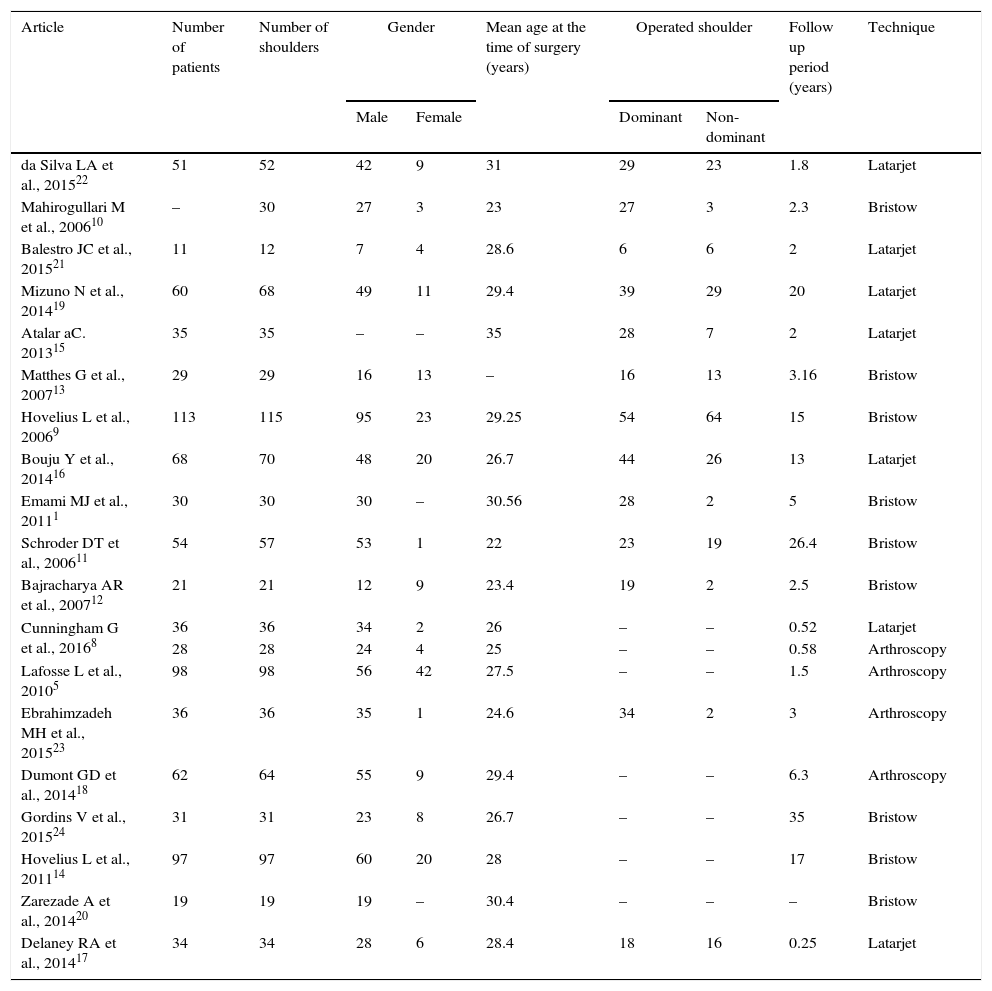
Collected general data for each included study.
| Article | Number of patients | Number of shoulders | Gender | Mean age at the time of surgery (years) | Operated shoulder | Follow up period (years) | Technique | ||
|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Dominant | Non-dominant | ||||||
| da Silva LA et al., 201522 | 51 | 52 | 42 | 9 | 31 | 29 | 23 | 1.8 | Latarjet |
| Mahirogullari M et al., 200610 | – | 30 | 27 | 3 | 23 | 27 | 3 | 2.3 | Bristow |
| Balestro JC et al., 201521 | 11 | 12 | 7 | 4 | 28.6 | 6 | 6 | 2 | Latarjet |
| Mizuno N et al., 201419 | 60 | 68 | 49 | 11 | 29.4 | 39 | 29 | 20 | Latarjet |
| Atalar aC. 201315 | 35 | 35 | – | – | 35 | 28 | 7 | 2 | Latarjet |
| Matthes G et al., 200713 | 29 | 29 | 16 | 13 | – | 16 | 13 | 3.16 | Bristow |
| Hovelius L et al., 20069 | 113 | 115 | 95 | 23 | 29.25 | 54 | 64 | 15 | Bristow |
| Bouju Y et al., 201416 | 68 | 70 | 48 | 20 | 26.7 | 44 | 26 | 13 | Latarjet |
| Emami MJ et al., 20111 | 30 | 30 | 30 | – | 30.56 | 28 | 2 | 5 | Bristow |
| Schroder DT et al., 200611 | 54 | 57 | 53 | 1 | 22 | 23 | 19 | 26.4 | Bristow |
| Bajracharya AR et al., 200712 | 21 | 21 | 12 | 9 | 23.4 | 19 | 2 | 2.5 | Bristow |
| Cunningham G et al., 20168 | 36 | 36 | 34 | 2 | 26 | – | – | 0.52 | Latarjet |
| 28 | 28 | 24 | 4 | 25 | – | – | 0.58 | Arthroscopy | |
| Lafosse L et al., 20105 | 98 | 98 | 56 | 42 | 27.5 | – | – | 1.5 | Arthroscopy |
| Ebrahimzadeh MH et al., 201523 | 36 | 36 | 35 | 1 | 24.6 | 34 | 2 | 3 | Arthroscopy |
| Dumont GD et al., 201418 | 62 | 64 | 55 | 9 | 29.4 | – | – | 6.3 | Arthroscopy |
| Gordins V et al., 201524 | 31 | 31 | 23 | 8 | 26.7 | – | – | 35 | Bristow |
| Hovelius L et al., 201114 | 97 | 97 | 60 | 20 | 28 | – | – | 17 | Bristow |
| Zarezade A et al., 201420 | 19 | 19 | 19 | – | 30.4 | – | – | – | Bristow |
| Delaney RA et al., 201417 | 34 | 34 | 28 | 6 | 28.4 | 18 | 16 | 0.25 | Latarjet |
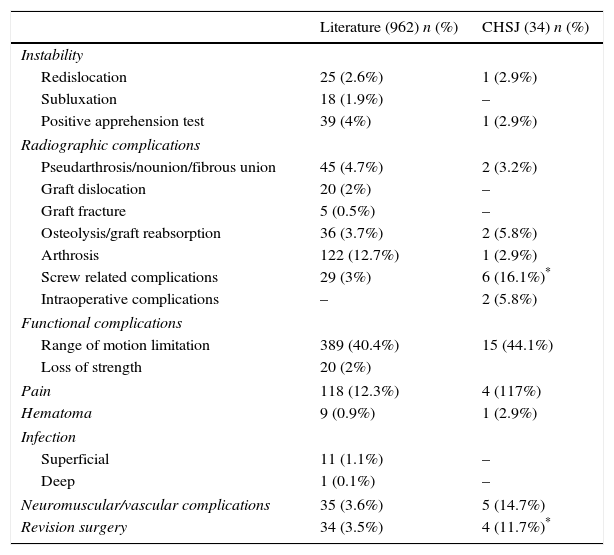
Range of motion limitation refers to movements in every direction, but the most significant one was the restriction in external rotation, found in 82% of the shoulders with range of motion limitation. Screw related complications include screw fracture, migrations and the presence of loose or prominent screws. Neuromuscular complications include intraoperative alerts (26), axillary nerve damage (5), musculocutaneous nerve damage (1) and deltoid muscle atrophy (3). Besides intraoperative nerve alerts, no other intraoperative complications were reported in the literature.
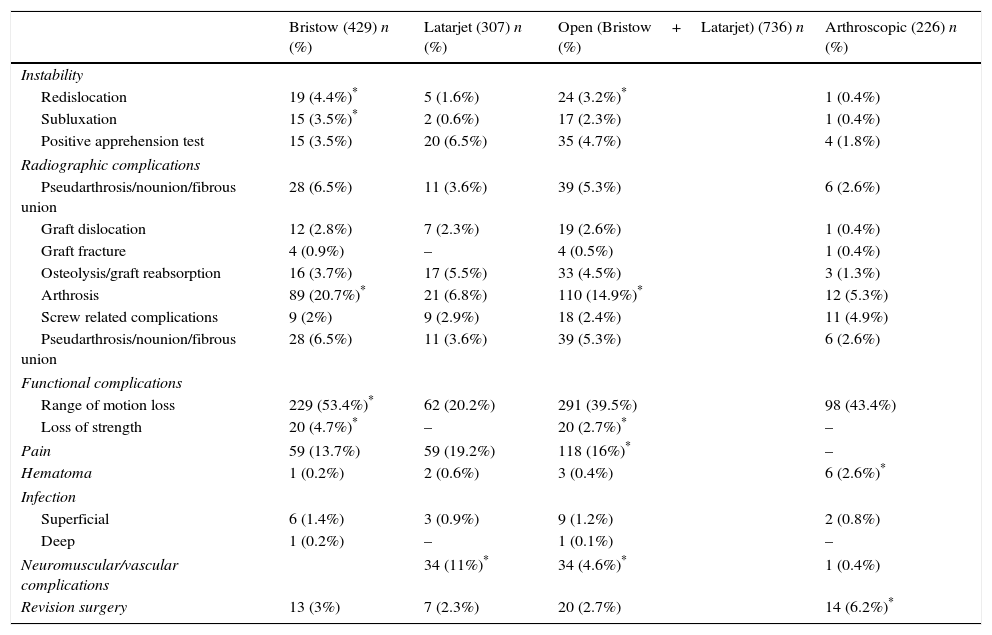
As presented in Table 4, and although the open techniques were generally associated to a higher rate of complications, the arthroscopic technique is associated with a significantly higher number of hematoma and revision surgery.
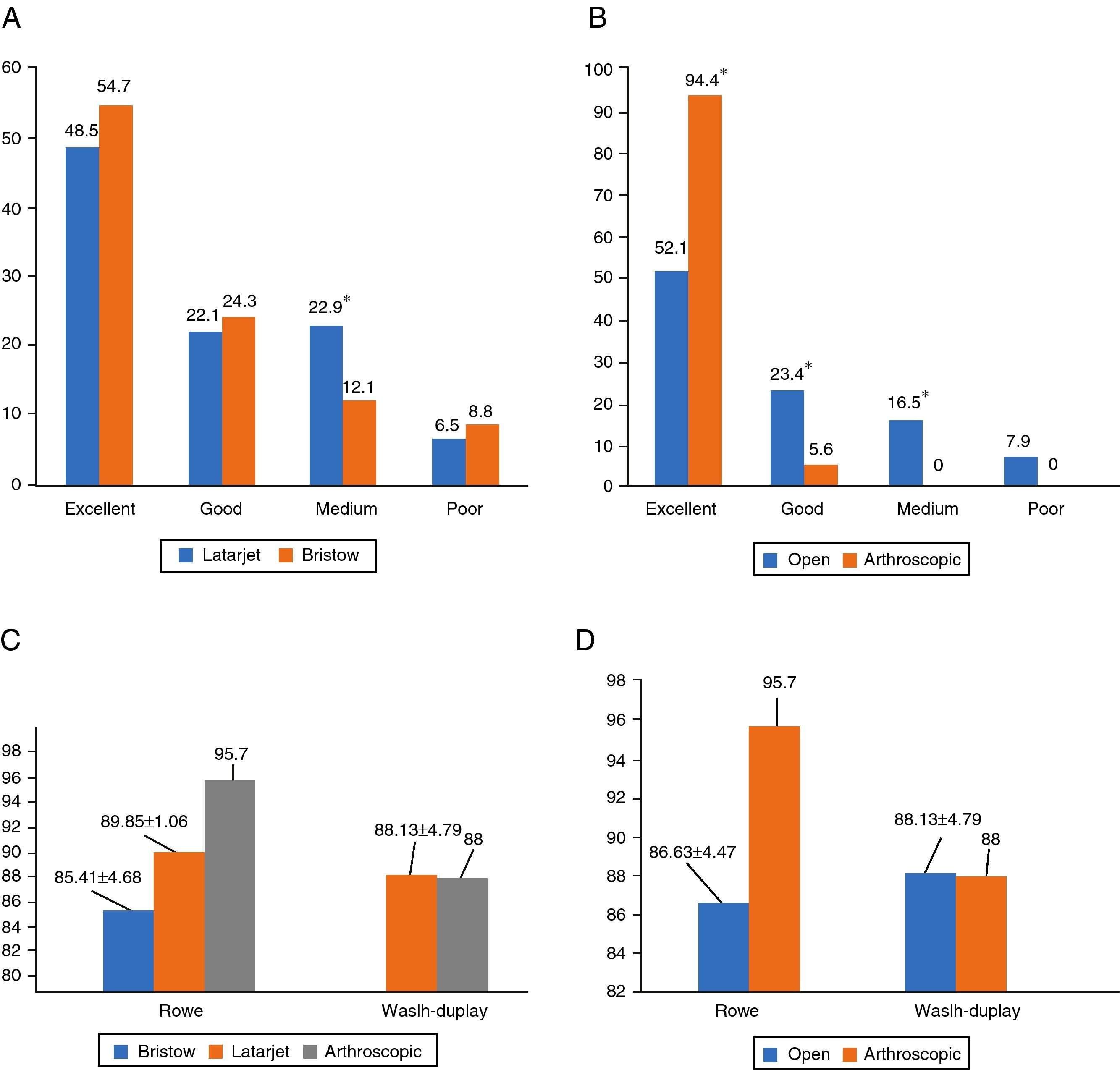
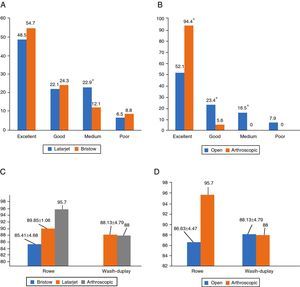
Relative to the functional scores, graphics A and B compare the qualitative functional results (“Excellent”, “Good”, “Fair” and “Poor”) reported in the literature, associated with the Bristow and Latarjet techniques (Graphic A) and with open and arthroscopic techniques (Graphic B). There is a significantly higher percentage of “Excellent” results with the arthroscopic techniques when compared to the open procedures, while these were associated with higher “Good” and “Fair” results (Fig. 1).
Graphics describing and comparing the percentages of qualitative evaluation and quantitative means of the functional scores. (A) Percentage of each functional result associated with Bristow and Latarjet procedures. (B) Percentage of each functional result associated with open and arthroscopic procedures. (C) Quantitative mean of the functional scores associated with the Bristow, Latarjet and arthroscopic techniques. (D) Quantitative mean of the functional scores associated with the open and arthroscopic techniques.
Graphics C and D represent the comparison between the quantitative means of the Rowe and Walsh Duplay scores associated with Bristow, Latarjet and Arthroscopic (Graphic C) and with the open and arthroscopic procedures (Graphic D). The differences between the procedures were not statistically significant despite the overall better evaluation of the arthroscopic technique with the Rowe score. To be noted that only 2 studies relating to the arthroscopic procedure reported functional scores results: one of them used the Rowe Score and the other used the Walsh-Duplay score, thus, the mean and standard deviation was not calculated for this technique in graphics C and D.
CHSJRelative to the CHSJ data, a total of 34 patients were included, of which 27 (79%) were male and 7 (21%) were female. The mean age at the time of the procedure was 28 years old. Although the dominance of the operated shoulder was not registered, 15 of them were right shoulders and 19 were left. The average follow-up period was 8 months (ranging from 1 month to 5 years) (Table 1).
Out of all the operated shoulders, 19 underwent the Bristow procedure, 10 the Latarjet procedure and 5 the arthroscopic Latarjet procedure (Table 1) and 47% of all the surgeries were performed by the same surgeon.
The total number and percentage of complications (from all the techniques) is discriminated in Table 3. The intraoperative complications include graft fracture and loss of fixation. Revision surgery was performed due to screw related complications (3) and graft reabsorption (1). As found in the literature results, the most significant movement affected by the range of motion limitation was external rotation, found in 67% of the shoulders with range of motion limitation and neuromuscular complications included axillary nerve damage (1), atrophy of the deltoid muscle (2), atrophy of the triceps muscle (1) and chronic neurogenic atrophy (1).
Total of complications found in the literature and in CHSJ, the University hospital. The data are presented as number and percentage of individuals that suffered that complication.
| Literature (962) n (%) | CHSJ (34) n (%) | |
|---|---|---|
| Instability | ||
| Redislocation | 25 (2.6%) | 1 (2.9%) |
| Subluxation | 18 (1.9%) | – |
| Positive apprehension test | 39 (4%) | 1 (2.9%) |
| Radiographic complications | ||
| Pseudarthrosis/nounion/fibrous union | 45 (4.7%) | 2 (3.2%) |
| Graft dislocation | 20 (2%) | – |
| Graft fracture | 5 (0.5%) | – |
| Osteolysis/graft reabsorption | 36 (3.7%) | 2 (5.8%) |
| Arthrosis | 122 (12.7%) | 1 (2.9%) |
| Screw related complications | 29 (3%) | 6 (16.1%)* |
| Intraoperative complications | – | 2 (5.8%) |
| Functional complications | ||
| Range of motion limitation | 389 (40.4%) | 15 (44.1%) |
| Loss of strength | 20 (2%) | |
| Pain | 118 (12.3%) | 4 (117%) |
| Hematoma | 9 (0.9%) | 1 (2.9%) |
| Infection | ||
| Superficial | 11 (1.1%) | – |
| Deep | 1 (0.1%) | – |
| Neuromuscular/vascular complications | 35 (3.6%) | 5 (14.7%) |
| Revision surgery | 34 (3.5%) | 4 (11.7%)* |
Complications associated with open (Bristow and Latarjet) and arthroscopic techniques found in the literature review. The data are presented as number and percentage of individuals that suffered that complication.
| Bristow (429) n (%) | Latarjet (307) n (%) | Open (Bristow+Latarjet) (736) n (%) | Arthroscopic (226) n (%) | |
|---|---|---|---|---|
| Instability | ||||
| Redislocation | 19 (4.4%)* | 5 (1.6%) | 24 (3.2%)* | 1 (0.4%) |
| Subluxation | 15 (3.5%)* | 2 (0.6%) | 17 (2.3%) | 1 (0.4%) |
| Positive apprehension test | 15 (3.5%) | 20 (6.5%) | 35 (4.7%) | 4 (1.8%) |
| Radiographic complications | ||||
| Pseudarthrosis/nounion/fibrous union | 28 (6.5%) | 11 (3.6%) | 39 (5.3%) | 6 (2.6%) |
| Graft dislocation | 12 (2.8%) | 7 (2.3%) | 19 (2.6%) | 1 (0.4%) |
| Graft fracture | 4 (0.9%) | – | 4 (0.5%) | 1 (0.4%) |
| Osteolysis/graft reabsorption | 16 (3.7%) | 17 (5.5%) | 33 (4.5%) | 3 (1.3%) |
| Arthrosis | 89 (20.7%)* | 21 (6.8%) | 110 (14.9%)* | 12 (5.3%) |
| Screw related complications | 9 (2%) | 9 (2.9%) | 18 (2.4%) | 11 (4.9%) |
| Pseudarthrosis/nounion/fibrous union | 28 (6.5%) | 11 (3.6%) | 39 (5.3%) | 6 (2.6%) |
| Functional complications | ||||
| Range of motion loss | 229 (53.4%)* | 62 (20.2%) | 291 (39.5%) | 98 (43.4%) |
| Loss of strength | 20 (4.7%)* | – | 20 (2.7%)* | – |
| Pain | 59 (13.7%) | 59 (19.2%) | 118 (16%)* | – |
| Hematoma | 1 (0.2%) | 2 (0.6%) | 3 (0.4%) | 6 (2.6%)* |
| Infection | ||||
| Superficial | 6 (1.4%) | 3 (0.9%) | 9 (1.2%) | 2 (0.8%) |
| Deep | 1 (0.2%) | – | 1 (0.1%) | – |
| Neuromuscular/vascular complications | 34 (11%)* | 34 (4.6%)* | 1 (0.4%) | |
| Revision surgery | 13 (3%) | 7 (2.3%) | 20 (2.7%) | 14 (6.2%)* |
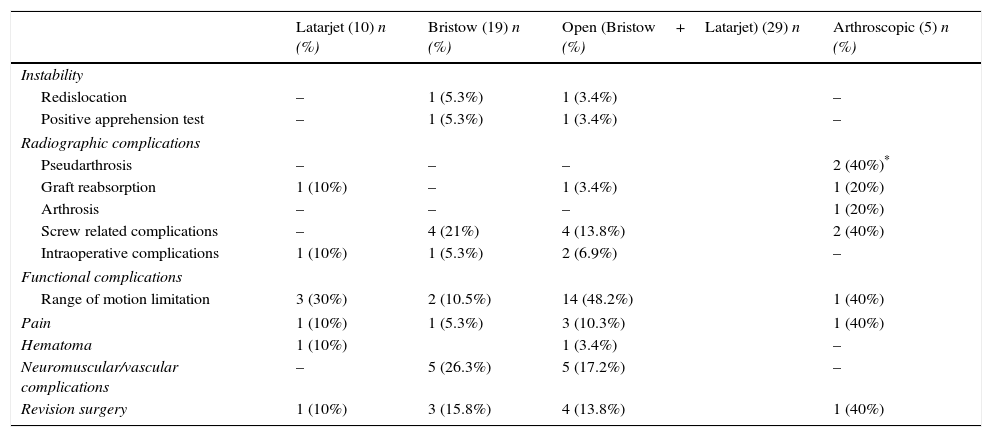
Table 5 describes and allows the comparison between the complications found associated with Bristow and Latarjet, as well as the comparison between open (Bristow and Latarjet) and all arthroscopic techniques. The statistically significant results are marked in Table: *=p<0.05. There was a significantly higher number of pseudarthrosis associated with the arthroscopic technique when compared with the open procedures. There were no other statistically significant differences relating to the other complications.
Complications associated with open (Bristow and Latarjet) and arthroscopic techniques found in the CHSJ the University hospital. The data are presented as number and percentage of individuals that suffered that complication.
| Latarjet (10) n (%) | Bristow (19) n (%) | Open (Bristow+Latarjet) (29) n (%) | Arthroscopic (5) n (%) | |
|---|---|---|---|---|
| Instability | ||||
| Redislocation | – | 1 (5.3%) | 1 (3.4%) | – |
| Positive apprehension test | – | 1 (5.3%) | 1 (3.4%) | – |
| Radiographic complications | ||||
| Pseudarthrosis | – | – | – | 2 (40%)* |
| Graft reabsorption | 1 (10%) | – | 1 (3.4%) | 1 (20%) |
| Arthrosis | – | – | – | 1 (20%) |
| Screw related complications | – | 4 (21%) | 4 (13.8%) | 2 (40%) |
| Intraoperative complications | 1 (10%) | 1 (5.3%) | 2 (6.9%) | – |
| Functional complications | ||||
| Range of motion limitation | 3 (30%) | 2 (10.5%) | 14 (48.2%) | 1 (40%) |
| Pain | 1 (10%) | 1 (5.3%) | 3 (10.3%) | 1 (40%) |
| Hematoma | 1 (10%) | 1 (3.4%) | – | |
| Neuromuscular/vascular complications | – | 5 (26.3%) | 5 (17.2%) | – |
| Revision surgery | 1 (10%) | 3 (15.8%) | 4 (13.8%) | 1 (40%) |
No functional scores were registered in this hospital.
Literature vs CHSJRelative to the total of complications, the CHSJ had a higher percentage of screw related complications and revision surgery when compared to the data reported in the literature (Table 2) and considering only the Bristow procedure, there is a significantly higher proportion of arthrosis and range of motion limitation in the literature when compared to the CHSJ. Among all the open procedures, there is a significantly higher proportion of arthrosis in the literature when compared to the CHSJ. On the other hand, there is a significantly higher proportion of screw related complications and revision surgery in the CHSJ data when compared to the literature and relative to the arthroscopic procedure, there was a significantly higher proportion of pseudarthrosis and screw related complications in the CHSJ data.
DiscussionThis study aimed to compare the incidence of complications associated to the different coracoid transfer procedures, open and arthroscopic, and simultaneously assess whether the data from the CHSJ differ significantly, or not, from the literature. Despite being effective and widely used techniques for the treatment of recurrent dislocation of the shoulder, the Bristow–Latarjet procedures are generally associated with a substantial complication and reintervention rates, both in the literature and the CHSJ.
In the literature, the arthroscopic technique had a lower proportion of complications, being, however, associated with a higher reintervention rate when compared to the open techniques. Note that due to the relatively low number of arthroscopic surgeries performed in the CHSJ so far and, possibly, due to the shorter follow-up period, the low number of complications registered in this hospital precludes a good comparative analysis between the different techniques. The fact that the arthroscopic procedure is relatively recent and the surgeons are still in an early stage of the learning curve allows a greater room for progression so that better results can be achieved. Another factor to consider is the duration of the surgery. Theoretically, this is longer for arthroscopic procedures, what could translate in a higher postoperative functional limitation rate. This tendency was verified in the literature but not in the CHSJ.
Although Infection was a complication rarely found in the literature, it is still important to state that no case of infection was observed in the CHSJ data. Functional complications such as range of motion limitation were found in a high percentage of patients both in the literature (40.4%) and the CHSJ (44.1%) and there were no significant differences between techniques. The restriction in external rotation (the most common functional complication), for instance, may have important implications for athletes and should be one of the topics taken into consideration when making the therapeutic decision. Another complication widely mentioned in the literature was arthrosis (12.7%); however, it was only present in 2.9% of the CHSJ patients. This discrepancy can be explained by the large difference between the follow up periods.
The percentages associated with each complication may not relate to their real incidence since not all the studies focus on the same outcomes. For example, only 2 studies referred to neuromuscular/vascular complications, one of them focusing solely on these. Therefore, the short number of studies referring to neuromuscular/vascular complications limits the comparative analysis between techniques as far as this item is concerned. However, in theory, nerve and vascular damage during arthroscopic coracoid transfer would be of major concern because of the proximity of the brachial plexus and the axillary vessels.
There are several differences between the studies included in the literature review and the one performed with the CHSJ, namely, the sample size and the follow up period, which limit the comparison between literature and CHSJ. The mean age and the gender distribution were similar. Another limitation of this study lies in the scarcity of the hospital records and in the lack of standardized radiological assessment protocols in the CHSJ. The complications found in the CHSJ were obtained exclusively from retrospective data, which could possibly underestimate their incidence, since the records may not include minor complications.
To sum up, there are various techniques for the treatment of the recurrent dislocation of the shoulder, all of them with known success when it comes to prevention of recurrence. However, all of them are invariably associated with high complication rates, which reinforces the need to discuss them with each patient pre-operatively. Despite being associated with a slightly higher re-operation rate, in the literature, the arthroscopic technique was found to have an overall lower rate of complications when compared to the open procedures.
CHSJ presented a higher rate of screw related complications and revision surgery than the literature. However, concerning other complications and when assessing the procedures individually, no particular tendency was verified. One can therefore conclude that, despite being scarce, the CHSJ data roughly overlap the literature.
An active search for complications as well as a functional evaluation through standardized scores, in a long term prospective study, would be a way to overcome this study's limitations and clarify which of the techniques would guarantee better long term outcomes, concerning stability, motion, functional scores and prevention of arthrosis.
Conflicts of interestsThe authors declare no conflicts of interest.