Anal squamous cell cancer is an HPV associated disease, highly prevalent in HIV-infected men who have sex with men (MSM). We evaluate the prevalence of HPV infection in an HIV-positive MSM population attending our hospital. Cytological results are correlated with an HR-HPV genotype.
MethodsFrom February 2013 to July 2014, 95 anal Thin Prep cytologies and 17 histological specimens were evaluated in 89 HIV-infected MSM. HPV detection (cobas® HPV Test) was done in 78 patients. Patients with a positive cytological result were biopsied according to the recommendations of the European Society for Medical Oncology Clinical Practical Guidelines. The STATVIEW statistical computer program was used.
ResultsThe mean age was 37 years. Cytological results: 40% - NILM, 17.9% - ASCUS, 24.2% - LSIL, 4.2% - HSIL and 1.1% - AGC. The overall prevalence of HR-HPV was of 80.8%. In 76.9% of the cases, infection occurred with multiple HR-HPV genotypes. The “other” HR-HPV pattern was the most prevalent HR-HPV genotype. Considering age, HPV-16 prevalence was 50.0% and 28.6% in patients under and over 30 years, respectively. A histological specimen was obtained from 17 patients and 82.4% of them had AIN.
Conclusion1 - HIV-infected MSM is a highly HR-HPV genotype infected population; 2 - The multiple infection pattern was the most prevalent; 3 - “Other”, an HPV subtype was the most prevalent pattern; 4 - The prevalence of HPV infection and multiplicity of infection was directly related to the severity of the cytological abnormalities and age; 5 - HPV-16 prevalence was more prevalent in patients under 30 years.
Anal squamous cell cancer (ASCC) is a serious health problem, mainly in immunosuppressed patients such as human immunodeficiency virus (HIV) carriers and transplant recipients, as well as in men who have sex with men (MSM).
ASCC is a human papillovirus (HPV) associated disease, believed to arise at the squamocolumnar transition zone in precancerous dysplastic lesions and can be detected by cytology and/or anal anoscopy. Both of these methods have been extensively studied and validated for cervical cancer, and only recently addressed for ASCC. High-grade squamous intraepithelial neoplasia (HSIL), a dysplastic lesion for ASCC, is present in 30% of HIV-positive MSM, however neither the progression rate to ASCC nor the regression rate are known.1 There are over 100 HPV genotypes of which only 35 seem to be associated with the capacity of causing dysplastic changes, hence the importance of knowing the prevalence of these lesions as well as their association with the HPV genotypes. The aim of the present study was to define the prevalence of anal HR-HPV genotypes in HIV-positive MSM and their distribution according to cytological results, in a population of patients from the São João Hospital Center between February 2013 and July 2014.
Material and methodsThe present study includes 95 samples of anal liquid-based cytology (Thin Prep) and 17 histological specimens from 89 HIV-positive MSM, collected between February 2013 and July 2014. All patients were attending a medical appointment for HIV-infected MSM. These patients were all routinely submitted to anal cytology. Cytology assessment and an HPV test (cobas® HPV Test) were performed in all samples. Patients with positive cytological results (atypical squamous cells of undetermined significance [ASCUS] or higher grade lesions) were submitted to anoscopy with acetic acid and lugol, and suspicious lesions were mapped and biopsied (according to the recommendations of the European Society for Medical Oncology Clinical Practical Guidelines). Statistical analysis of frequency distribution and correlation X square tests were performed using the STATVIEW statistical computer program.
Specimen collection and diagnosisAnal samples were collected by clinicians using an endocervical brush device (Cytobrush Hologic), according to the manufacturer's instructions and then the brush was rinsed in Thin Prep PreservCyt solution.
Liquid-based cytology samples were prepared using the Thin Prep processor and stained with the Papanicolaou method. Hypocellular samples were considered inadequate for the cytological analysis and HPV test. Cytological results were reported following the Bethesda 2001 classification, also accepted for anal cytology.
Detection and genotyping of HPVIn the remainder of the liquid-based anal cytology specimen, HPV detection was performed using the second-generation Roche HPV test (cobas® HPV Test), according to the manufacturer's instructions. The cobas® HPV Test is a qualitative multiplex assay that provides specific genotyping information for HPV types 16 and 18, while concurrently detecting the other 12 HR-HPV types (31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66 and 68) in a pooled result, at clinically relevant infection levels.
ß-globin from cellular input was used as an internal control to assess specimen quality and identify specimens containing factors that inhibit the amplification process.
ResultsA total of 95 Thin Prep cytological specimens from 89 patients were reviewed and classified. The mean age of the patients was 37 years (range of 19-62 years; median 35.9 years). Cytologies were classified as no cytological epithelial anomalies (NILM) (40%), ASCUS (17.9%), low-grade squamous intraepithelial lesion [LSIL] (24.2%), HSIL (4.2%) and atypical glandular cells [AGC] (1.1%). Hipocellularity was found in 12.6% of the samples, which was considered unsatisfactory for diagnosis.
HR-HPV was successfully performed in 78 patients and a positive result was found in 63 patients (80.8%).
In 60 patients (95.2%), infection occurred with multiple HR-HPV types (90.9% in LSIL and 100% in HSIL). Simple infection occurred in only three patients (3.8%), all with HPV-16, two with NILM, and one with LSIL. The HPV multiple infection pattern distribution was: HPV-16 and “other” in 19 patients (24.4%), HPV-16, 18 and “other” in five patients (6.4%), HPV-18 and “other” in six patients (7.7%), and “other” in 30 patients (38.5%). HPV-16 was present as a co-infection or as a single agent in 27 patients (42.9%), and infection with “other” subtypes was present in 60 patients (95.2%). HPV-18 was never present as a single agent and was detected in 11 patients (17.5%).
The most prevalent HR-HPV type pattern was obtained with “other” HR-HPV types (38.5%), followed by infection with HPV-16 together with “other” HR-HPV types (24.4%).
When correlating cytological results with HR-HPV types, all HPV positive patients had satisfactory cytological samples: NILM in 25 patients (39.7%), ASCUS in 13 patients (20.6%), LSIL in 21 patients (33.3%) and HSIL in four patients (6.3%).
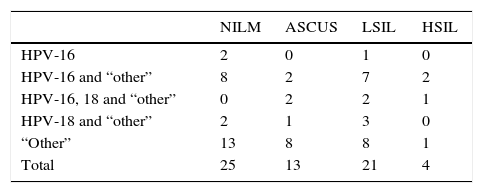
The distribution of the HPV pattern of infection and its correlation with cytological results is described in Table 1.
Cytological results according to HPV infection patterns.
| NILM | ASCUS | LSIL | HSIL | |
|---|---|---|---|---|
| HPV-16 | 2 | 0 | 1 | 0 |
| HPV-16 and “other” | 8 | 2 | 7 | 2 |
| HPV-16, 18 and “other” | 0 | 2 | 2 | 1 |
| HPV-18 and “other” | 2 | 1 | 3 | 0 |
| “Other” | 13 | 8 | 8 | 1 |
| Total | 25 | 13 | 21 | 4 |
ASCUS, atypical squamous cells of undetermined significance; HSIL, high-grade squamous intraepithelial neoplasia; LSIL, low-grade squamous intraepithelial lesion; NILM, negative for intraepithelial lesion or malignancy.
When considering age, 22 patients (28.2%) were younger than 30 years and 56 (71.8%) patients were older than 30 years. Positive cytological results (lesions classified as ASCUS or with a higher degree) were diagnosed in 28.2% of patients aged less than 30 years and 70.5% in patients over 30 years. All cytological diagnosis of HSIL occurred in patients over 30 years. Concerning the distribution of HPV subtype prevalence in the considered age groups, a significant difference was found in relation to HPV-16 infection prevalence, HPV-16 was prevalent in 11 patients (50%) and in 16 patients (28.6%) of patients under and over 30 years, respectively. “The other” subtype HR-HPV infection was present in 17 patients (77.3%) and in 43 patients (76.8%) under and over 30 years, respectively, and HPV-18 was detected in three (13.6%) and eight (14.3%) cases, respectively.
Histological specimens were observed in 17 patients. A positive histological result (anal intraepithelial neoplasia [AIN]) was achieved in 14 patients (82.4%) (n=11 [64.7%] with AIN I and n=3 [17.6%] with AIN II/III).
Biopsy was performed in two patients with the cytological result of NILM, in both a diagnosis of AIN I was obtained. One had HPV-16 and the other was positive for “other” HPV subtypes.
DiscussionWe recognize the limited number and the biased selection of patients. Our patients belong to a selected hospital population of HIV-positive MSM that attended a medical oriented appointment during a period of 17 months. Variables such as sociodemographic data, number of sexual partners, HIV viral load, antiretroviral treatment status or immunological condition (CD4 T cell counts) were not considered. Age was considered and patients were classified in 5-year age intervals. However, when grouping patients in 5-year interval categories, a reduced number of patients was included in each category providing no reliability for further considerations. Thus, a dichotomic division of patients under and over 30 years was preferred. As routine, all patients were submitted to anal cytology and further anoscopy with biopsy according to the recommendations of the European Society for Medical Oncology Clinical Practical Guidelines. A cobas® HPV Test was performed in all cytological samples.
Nevertheless, our results were consistent with those of previous publications, regarding the prevalence of HR-HPV infection in HIV-positive MSM.1–4 In his paper, Del Amo et al. refer to 83.4% of HPV infected individuals among HIV-positive MSM.4 Torres et al. refer a prevalence of 83.0% of HR-HPV infection in HIV-positive MSM.2 In our series, 80.8% of HIV-positive MSM were HR-HPV positive as well. This prevalence seems to rise with cytological abnormality.2 In fact, we found a prevalence of 73.5% of HR-HPV infection in patients with NILM, while in patients with a positive cytological result, the percentage of HR-HPV infection increased with the degree of severity of the cytological result (ASCUS - 76.5%; LSIL - 95.5% and HSIL - 100%).
In our series, only 5.1% of the patients had HSIL, a much lower rate considering those reported by other series at 30%.5
Multiple HR-HPV infections also seem to be more frequent than isolated infections.1,4 An association between multiplicity HR-HPV infection, age, number of recent sexual partners and cytological abnormalities has been referred.4,6–8 According to Van der Loeff et al., it seems that the multiple infection status was more common with the advancing degree of histological abnormality, 45.5% for AIN-I cases and 76.3% of AIN-III cases.1 Multiplicity of HR-HPV types were found in our series in 76.9% of infected patients, being 67.6% in patients with NILM, 76.5% in ASCUS, 90.9% in LSIL and 100% in HSIL. Other studies have also found that multiple HR-HPV infection was correlated with age, reaching its peak at 35 years and also with the number of sexual partners in the previous year.4 Unfortunately, due to the reduced number of patients included in our sample, we did not find any significant influence of age in the multiplicity of the HR-HPV type.
As expected, HPV-16 was highly prevalent (42.9%), but in the present study the most prevalent status of infection was obtained with “other” HR-HPV subtypes (65.79%). This result could be dependent on the small size of our sample. HPV-16 was present in 14 patients (48.3%) with ASCUS and/or LSIL and in two (50%) patients with HSIL. HPV-18 was only present in eight (27.6%) patients of the ASCUS and/or LSIL patients and in 25% of the HSIL patients. HPV-16 and 18 was found in five patients, four of them with a cytological diagnosis of ASCUS and/or LSIL and the other with HSIL.
In previous studies, the peak prevalence for HPV is observed in patients in their late thirties.2,4 Most of our patients (69.2%) were between 26 and 45 years of age. When considering only two groups, under and over 30 years, we did not find any differences with respect to the prevalence of positive cytologies or in the prevalence of HPV types, except for the prevalence of HPV-16 that was much higher in those under 30 years (50.0% vs 28.6%). All of our HSIL were diagnosed in patients older than 30 years.
ConclusionsDespite the great limitations of our study, we showed, as previously reported by other authors, that HIV-positive MSM, are 1 - a highly infected HR-HPV population, 2 - the prevalence of HPV infection raises with cytological abnormality 3 - the most common pattern of infection occurs with multiple HR-HPV types and this multiplicity seems to also be correlated with age, 4 - “other” HPV subtypes seem to be the most prevalent HR-HPV type, except for those patients under 30 years, where HPV-16 is significantly more prevalent, 5 - HPV-18 seems to be the least prevalent HR-HPV subtype. Further studies performed in larger and more diverse populations with an investigation of past and current sexual behaviour as well as studies including more discriminated HR-HPV types can be helpful in order to evaluate the impact of the different HR-HPV types in anal squamous cell cancer.
FundingNo external funding was received and all costs were supported by the São João Hospital Center as part of routine work.