Brachial plexopathy (BP) is a heterogeneous neurological entity that can generate different degrees of disability.1 Non-traumatic etiologies are rare, with infectious causes representing less than 2% of cases.2 In this case, we present a patient with BP due to varicella-zoster virus (VZV) as the initial manifestation of a human immunodeficiency virus (HIV) infection.
A 54-year-old male patient from Cali, Colombia, who consulted for the appearance of vesicular lesions and pruritic scabs; 10 days later, he present a sudden paresis of the LUL, with burning pain in the anterior and lateral face of the arm, without episodes of pain in LUL before the motor deficit, no fever, gastrointestinal or respiratory symptoms. His only personal history was long-standing hearing loss without studies on the matter.
Underweight, a preserved cognitive response and functional cranial nerves, with negative meningeal signs, were found, also LUL paresis that limited abduction, flexion, and rotations of the shoulder with a manual muscle test (MMT) of 0/5, in flexion and extension of the elbow 2/5, flexion and extension of wrist and hand 1/5, decreased muscle tone, and hyporeflexia. The other limbs with a 5/5 MMT. The sensory evaluation found allodynia in different areas of the LUL, without having a ro"ot or peripheral nerve distribution with a severe pain intensity of 7/10 on the numerical classification scale (NCS).
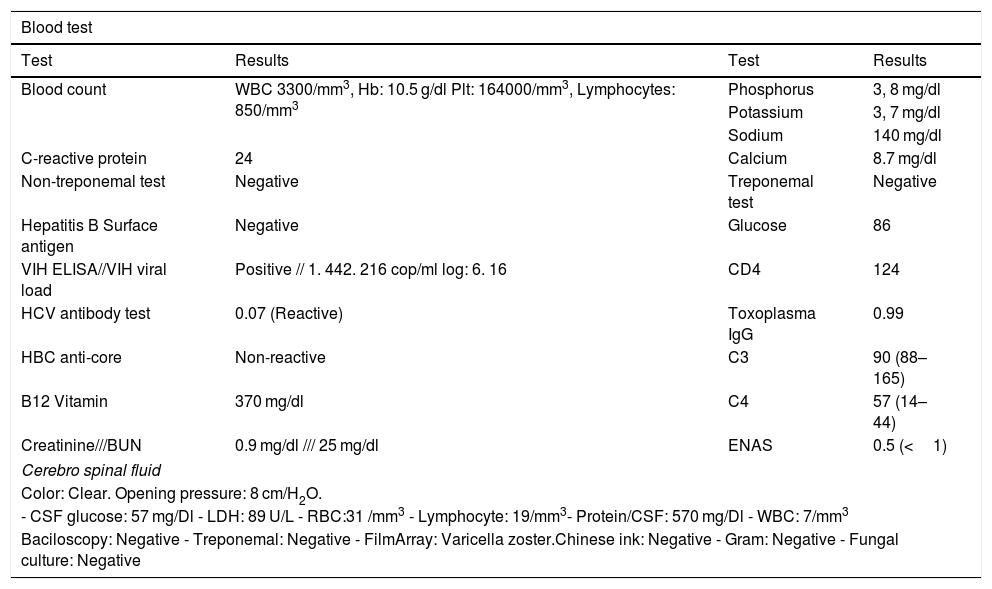
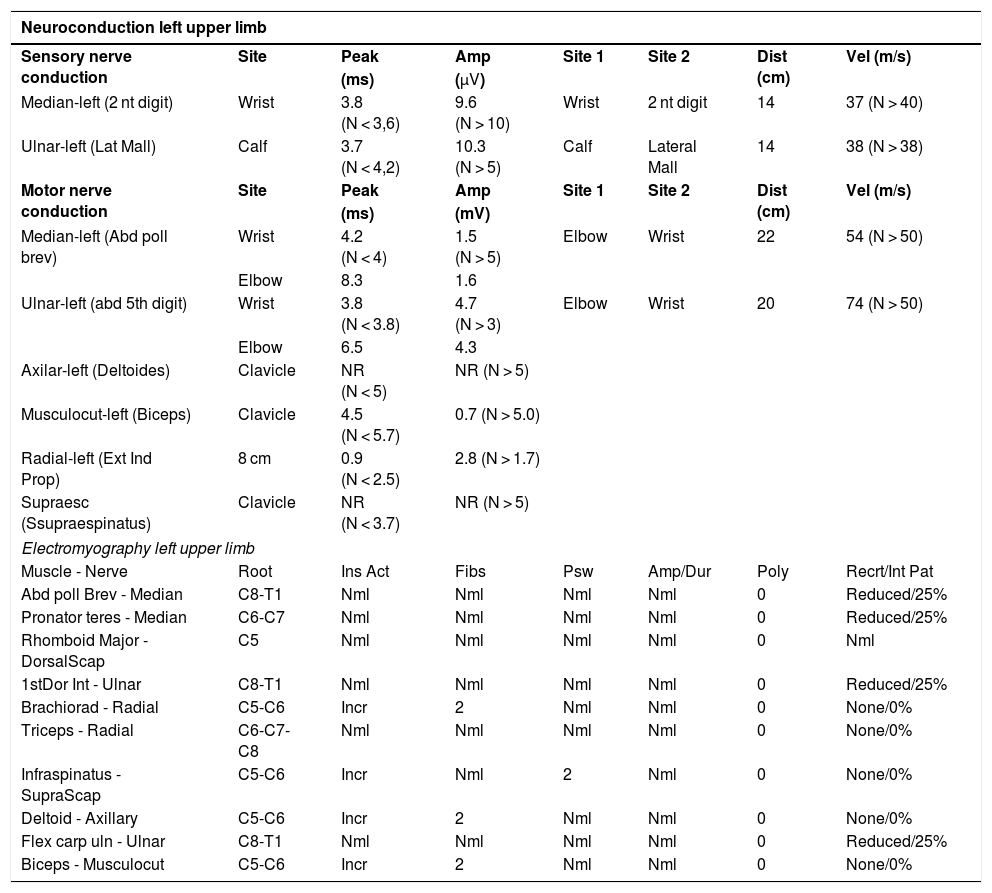
Multiple diagnostic studies were performed, finding a positive rapid test for HIV and a viral load of 1.442.216 copies/ml and total CD4 of 124, considering a patient in the AIDS phase. A lumbar puncture was performed with a cytochemical of cerebrospinal fluid with hyper protein spinal cord and mixed pleocytosis, a normal opening pressure, and a positive filmArray for VVZ (Table 1). In the imaging studies, a normal magnetic resonance imaging (MRI) of the brain and cervical spine and an MRI with angiography without alterations, ruling out vascular or brain parenchymal involvement. Electromyography studies plus LUL neuron conduction reported a severe incomplete axonal lesion of the left brachial plexus, at the level of the upper, middle, and lower trunks without signs of re-innervation, the patient was diagnosed with a VVZ brachial plexopathy (Table 2).
Patient studies.
| Blood test | |||
|---|---|---|---|
| Test | Results | Test | Results |
| Blood count | WBC 3300/mm3, Hb: 10.5 g/dl Plt: 164000/mm3, Lymphocytes: 850/mm3 | Phosphorus | 3, 8 mg/dl |
| Potassium | 3, 7 mg/dl | ||
| Sodium | 140 mg/dl | ||
| C-reactive protein | 24 | Calcium | 8.7 mg/dl |
| Non-treponemal test | Negative | Treponemal test | Negative |
| Hepatitis B Surface antigen | Negative | Glucose | 86 |
| VIH ELISA//VIH viral load | Positive // 1. 442. 216 cop/ml log: 6. 16 | CD4 | 124 |
| HCV antibody test | 0.07 (Reactive) | Toxoplasma IgG | 0.99 |
| HBC anti-core | Non-reactive | C3 | 90 (88–165) |
| B12 Vitamin | 370 mg/dl | C4 | 57 (14–44) |
| Creatinine///BUN | 0.9 mg/dl /// 25 mg/dl | ENAS | 0.5 (<1) |
| Cerebro spinal fluid | |||
| Color: Clear. Opening pressure: 8 cm/H2O. | |||
| - CSF glucose: 57 mg/Dl - LDH: 89 U/L - RBC:31 /mm3 - Lymphocyte: 19/mm3- Protein/CSF: 570 mg/Dl - WBC: 7/mm3 | |||
| Baciloscopy: Negative - Treponemal: Negative - FilmArray: Varicella zoster.Chinese ink: Negative - Gram: Negative - Fungal culture: Negative | |||
WBC: White blood cells, RBC: Red blood cells, Hb: Hemoglobim, Plt: Platelet, VIH: Human immunodeficiency virus, HB: Hepatitis, BUN: Blood urea nitrogen, CSF: cerebrospinal fluid.
Electromyography and nerve conduction studies.
| Neuroconduction left upper limb | |||||||
|---|---|---|---|---|---|---|---|
| Sensory nerve conduction | Site | Peak | Amp | Site 1 | Site 2 | Dist (cm) | Vel (m/s) |
| (ms) | (μV) | ||||||
| Median-left (2 nt digit) | Wrist | 3.8 (N < 3,6) | 9.6 (N > 10) | Wrist | 2 nt digit | 14 | 37 (N > 40) |
| Ulnar-left (Lat Mall) | Calf | 3.7 (N < 4,2) | 10.3 (N > 5) | Calf | Lateral Mall | 14 | 38 (N > 38) |
| Motor nerve conduction | Site | Peak | Amp | Site 1 | Site 2 | Dist (cm) | Vel (m/s) |
| (ms) | (mV) | ||||||
| Median-left (Abd poll brev) | Wrist | 4.2 (N < 4) | 1.5 (N > 5) | Elbow | Wrist | 22 | 54 (N > 50) |
| Elbow | 8.3 | 1.6 | |||||
| Ulnar-left (abd 5th digit) | Wrist | 3.8 (N < 3.8) | 4.7 (N > 3) | Elbow | Wrist | 20 | 74 (N > 50) |
| Elbow | 6.5 | 4.3 | |||||
| Axilar-left (Deltoides) | Clavicle | NR (N < 5) | NR (N > 5) | ||||
| Musculocut-left (Biceps) | Clavicle | 4.5 (N < 5.7) | 0.7 (N > 5.0) | ||||
| Radial-left (Ext Ind Prop) | 8 cm | 0.9 (N < 2.5) | 2.8 (N > 1.7) | ||||
| Supraesc (Ssupraespinatus) | Clavicle | NR (N < 3.7) | NR (N > 5) | ||||
| Electromyography left upper limb | |||||||
| Muscle - Nerve | Root | Ins Act | Fibs | Psw | Amp/Dur | Poly | Recrt/Int Pat |
| Abd poll Brev - Median | C8-T1 | Nml | Nml | Nml | Nml | 0 | Reduced/25% |
| Pronator teres - Median | C6-C7 | Nml | Nml | Nml | Nml | 0 | Reduced/25% |
| Rhomboid Major - DorsalScap | C5 | Nml | Nml | Nml | Nml | 0 | Nml |
| 1stDor Int - Ulnar | C8-T1 | Nml | Nml | Nml | Nml | 0 | Reduced/25% |
| Brachiorad - Radial | C5-C6 | Incr | 2 | Nml | Nml | 0 | None/0% |
| Triceps - Radial | C6-C7-C8 | Nml | Nml | Nml | Nml | 0 | None/0% |
| Infraspinatus - SupraScap | C5-C6 | Incr | Nml | 2 | Nml | 0 | None/0% |
| Deltoid - Axillary | C5-C6 | Incr | 2 | Nml | Nml | 0 | None/0% |
| Flex carp uln - Ulnar | C8-T1 | Nml | Nml | Nml | Nml | 0 | Reduced/25% |
| Biceps - Musculocut | C5-C6 | Incr | 2 | Nml | Nml | 0 | None/0% |
Amp: Amplitude, Dist: Distance, Vel: Velocity, Ins act: Insertion activity, Fibs: fibrillation, Psw: Positive sharp waves, Dur: Duration, Poly: polyphasic, Recrt: Recruitment, Int Pat: Interference pattern, NML: Normal. NR: no response.
The patient required treatment with intravenous acyclovir for 14 days, in addition to pregabalin titrated up to 225 mg/day for neuropathic pain with adequate control, ENC 2/10. A rehabilitation plan was also established with functional objectives with physical and occupational therapy, in addition to orthotic management that achieved an adequate positioning and prevention of LUL contractures.
This case illustrates the neurological complications of varicella-zoster infection, in addition to generating the need to rule out the most frequent causes of immunosuppression in patients with this symptomatology.1 In the diagnostic approach, the patient's history and his semiological evaluation generate a diagnostic approach that must be confirmed with images and electrophysiological studies to rule out related etiologies. The findings of the involvement of the brachial plexus with emphasis on the middle and upper trunk confirmed the diagnosis and focused the multidisciplinary team on the comprehensive management of the patient, a Parsonage-Turner syndrome was ruled out by not complying with the typical presentation of onset and chronological evolution of pain and weakness.3
Herpes zoster is characterized by the reactivation of the varicella-zoster virus that has remained latent in the dorsal root ganglion, being associated with different neurological complications, most of them sensitive, with the motor involvement described in only 2–3% of patients, the cases.4 The motor deficit and pain could be related to an extension of the viral infection from the dorsal root ganglion to the anterior motor root before viral reactivation,4 however, it may be due to an intense inflammatory process and damage to the motor root due to an immune-mediated post-infectious phenomenon such as the one presented in this case,5 generally appears between the first and fourth week with a time range between 1 and 120 days.4
The treatment of this entity and its neurological and functional complications is based on antiretroviral management, in addition to transversal interventions in the disease process, with rehabilitation and pain management.2 The rehabilitation plan should include the maintenance of joint mobility arches, muscle strengthening, and sensory and motor re-education with an emphasis on activities of daily living. Pain interventions are various, starting from topical medication, gabapentinoids, atypical opioids to interventionism such as neurostimulation or surgical interventions; in this case, achieving symptom control with a gabapentinoid selected based on the safety of the patient's history and comorbidities.2
It is considered in these patients that an early diagnosis adjusted to a multidisciplinary intervention will generate a positive outcome in their quality of life, pain control, and return to daily activities, in addition to strict surveillance and management of their comorbidities.
Ethical considerationThe patient gave his consent for the use of clinical and paraclinical information, it was authorized by the ethics committee of the Hospital Universitario del Valle, Cali, Colombia.
FundingThe authors did not receive funding to carry out this report.
Declaratipon of Competing InterestWe declare that we have no conflict of interest.
To the Hospital Universitario del Valle Evaristo García E.S.E and its department of electro-diagnosis.