Wernicke encephalopathy (WE) is a serious, sometimes lethal disorder caused by thiamine (vitamin B1) deficiency, which is normally quickly reversible using vitamin supplementation. Most typically associated with alcoholism, it may also occur in patients with hyperemesis, hyperthyroidism, or tumours and those undergoing haemodialysis or bariatric surgery, and on occasions it is iatrogenic in patients who depend on parenteral nutrition.1–5
The classic triad of symptoms includes ataxia, ophthalmoplegia, and confusion; however, it is only present in 10% of the patients.5 In practice, symptoms are varied and non-specific, including neurological (amnesia, tremor, auditory and visual disturbances, hypothermia, etc.), digestive (nausea, vomiting, abdominal pain, etc.), and cardiovascular symptoms (changes in blood pressure and heart rate, dyspnoea, etc.),5,6 with the most serious one being lactic acidosis. Although usually mild, lactic acidosis may also be severe and even fatal.7
We present here the clinical case of a patient with symptoms of WE and severe lactic acidosis secondary to a thiamine deficiency due to the administration of parenteral nutrition without adequate vitamin supplementation.
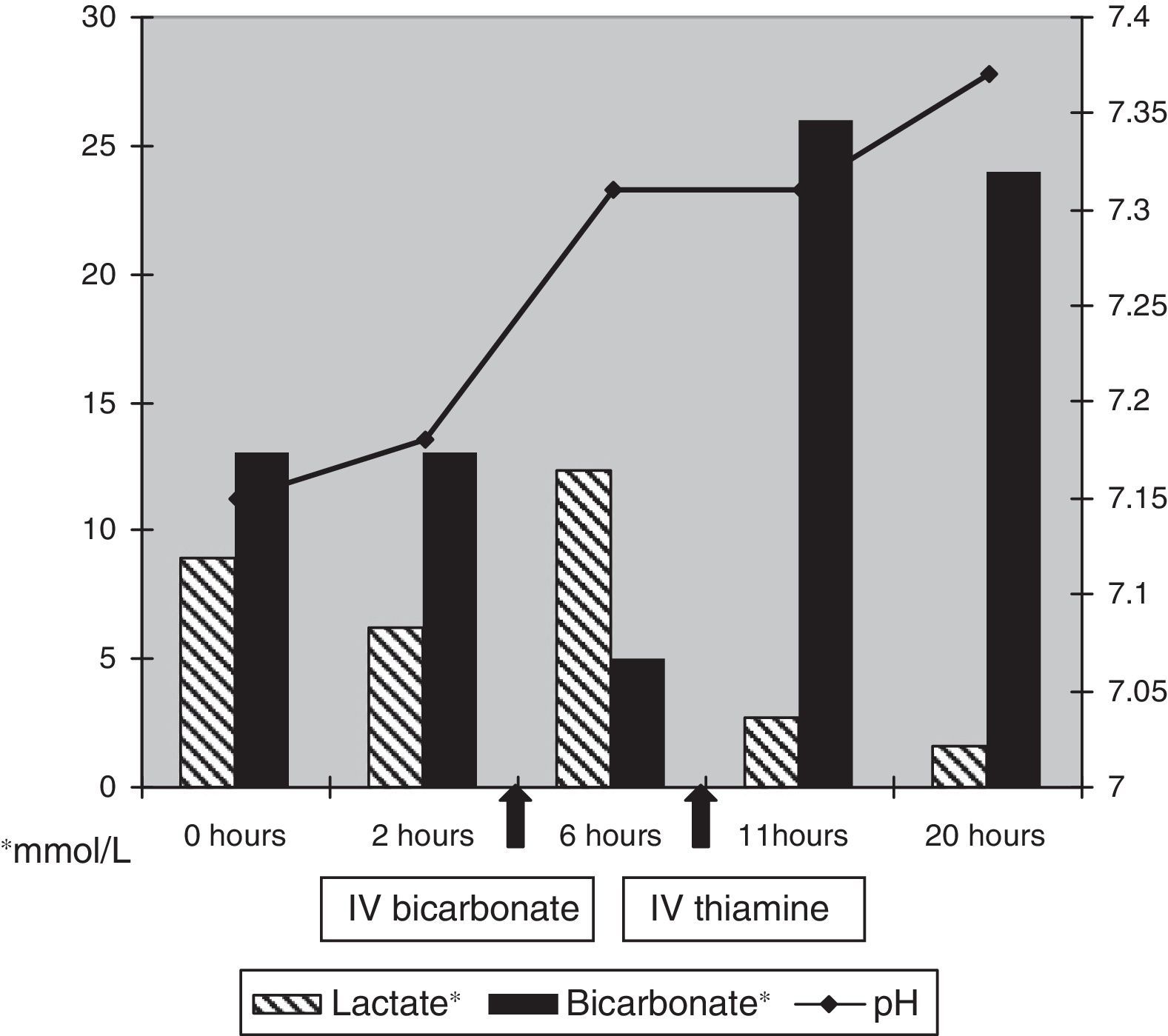
Our patient was a 2-year-old boy with VACTERL association (vertebral defects, anal atresia, cardiac defects, tracheoesophageal fistula and/or esophageal atresia, renal anomalies and limb defects). He presented episodic confusion, tachycardia, sweating, fluctuations in blood pressure and temperature, and a resting tremor 32 days after being admitted for an oesophagocoloplasty. Symptoms presented with increasing frequency and 2 days later were accompanied by paralysis of the left abducens nerve. Because of the patient's clinical situation and muscle atrophy, gait was not tested. Blood gas testing showed metabolic acidosis with hyperlactacidaemia (pH 7.18 and lactate 8.9mmol/L). Despite treatment with sodium bicarbonate, the acidosis worsened, reaching a pH of 7.15 and lactate levels of 12.3mmol/L with a base excess of −15. On reviewing his medical history, the lack of a multivitamin supplement to go with the patient's parenteral nutrition stood out and thiamine deficiency was suspected, so he received an intravenous infusion of thiamine (100mg in a single dose) along with cobalamin and carnitine. The patient improved rapidly after this treatment; acidosis resolved (Fig. 1), and the remaining symptoms disappeared within a few hours. Very low levels of thiamine were subsequently confirmed from a sample taken previous to treatment. The patient was followed up for 2 years and showed no sequelae from this set of symptoms.
Our patient presented with symptoms of WE and severe lactic acidosis secondary to thiamine deficiency due to parenteral nutrition without vitamin supplementation.8 As described in this case, lactic acidosis is refractory to treatment with sodium bicarbonate but shows fast clinical and biochemical responses to intravenous thiamine. It must be noted that without treatment, symptoms worsen quickly and result in death.8,9 The presence of low thiamine levels allows retrospective corroboration of the diagnosis in cases like ours. However, the diagnosis of WE is clinical, since imaging findings are not pathognomonic for this disease, and normal thiamine levels do not rule it out. Cases of WE have been reported where the patient showed normal or elevated levels of thiamine due to a genetic anomaly resulting in impaired thiamine transport at the mitochondrial level.10 When neuroimaging techniques are used on these patients, the images are consistent with a diagnosis of WE.9,11,12 In the case of our patient, we did not perform an MRI scan for ethical reasons (sedation) and due to the rapidity with which he recovered after treatment, but such images would probably have displayed alterations, particularly of the posterior hypothalamus and oculomotor nerve nuclei. The white matter, the dentate nucleus of the cerebellum, the red nucleus, and the putamen are frequently altered in children with WE.12
Lactic acidosis may be congenital or secondary, and is classified as either type A (increased lactate production) or type B (decreased lactate metabolism) depending on the pathogenic mechanism.7 Secondary lactic acidosis may be due to tissue hypoxia, liver or kidney involvement, tumours, intense exercise, seizures, drugs, and toxins. Treatments described in the literature for these entities include biguanides, antiretrovirals, isoniazid, linezolid, propylene glycol, propofol, adrenergic stimulants, and very occasionally, nalidixic acid and statins.7 This group also includes the cases associated with thiamine deficiency due to parenteral nutrition and those with d-lactic acidosis as a result of the overproduction of d-lactic acid by intestinal bacteria following oral antibiotic therapy in patients with short bowel syndrome.7,13
Thiamine, which is essential to glucose metabolism,14 is a cofactor for pyruvate dehydrogenase (PDH), α-ketoglutarate-dehydrogenase, and transketolase. PDH catalyses the conversion of pyruvic acid to acetyl coenzyme A, which means that a thiamine deficiency causes the accumulation of pyruvic acid which then transforms into lactic acid, resulting in hyperlactacidaemia.1 Thiamine forms a part of multivitamin complexes for children included in parenteral nutrition, with a recommended dose of 0.35–0.5mg/kg/day for preterm infants and 1.2mg/day for nursing infants and children.15 The association between total parenteral nutrition unsupplemented with thiamine and severe lactic acidosis and WE has been described in patients of all ages, and symptoms may develop in as few as 7 days.8,9 We should therefore maintain a high level of suspicion for this complication in children receiving parenteral nutrition who present with hyperlactacidaemia and clinical deterioration. Empirical thiamine treatment should be administered as soon as a lack of adequate supplementation to parenteral nutrition is confirmed.1,2 Prompt action can prevent comorbidities and even potential mortality caused by this severe iatrogenic complication.
FundingThis study has received no funding of any kind.
Please cite this article as: Hurtado Mingo A, Madruga Garrido M, Neth O, Obando I. Inusual complicación en la edad pediátrica: encefalopatía de Wernicke asociada a nutrición parenteral deficiente en tiamina. Neurología. 2016;31:280–281.
This study has not been presented at any of the SEN Annual Meetings. It was introduced as a poster display and clinical case at the National Congress of the Spanish Association of Pediatrics in 2012.