HaNDL syndrome (transient headache and neurological deficits with cerebrospinal fluid lymphocytosis) is characterised by one or more episodes of headache and transient neurological deficits associated with cerebrospinal fluid lymphocytosis. To date, few cases of HaNDL manifesting with confusional symptoms have been described. Likewise, very few patients with HaNDL and confusional symptoms have been evaluated with transcranial Doppler ultrasound (TCD). TCD data from patients with focal involvement reveal changes consistent with vasomotor alterations.
DevelopmentWe present the case of a 42-year-old man who experienced headache and confusional symptoms and displayed pleocytosis, diffuse slow activity on EEG, increased blood flow velocity in both middle cerebral arteries on TCD, and single-photon emission computed tomography (SPECT) findings suggestive of diffuse involvement, especially in the left hemisphere.
ConclusionsTo our knowledge, this is the first description of a patient with HaNDL, confusional symptoms, diffuse slow activity on EEG, and increased blood flow velocity in TCD. Our findings suggest a relationship between cerebral vasomotor changes and the pathophysiology of HaNDL. TCD may be a useful tool for early diagnosis of HaNDL.
El síndrome de cefalea y déficits neurológicos transitorios con pleocitosis en líquido cefalorraquídeo (acrónimo en inglés, HaNDL) se caracteriza por la presencia de uno o más episodios de cefalea y déficits neurológicos transitorios asociados con linfocitosis en líquido cefalorraquídeo. Hasta la fecha actual se han reportado escasos episodios de HaNDL con clínica compatible con cuadro confusional, y no se encuentran descritas mediciones de Doppler transcraneal (DTC) en pacientes afectos de HaNDL y cuadro confusional. En los registros DTC realizados en pacientes con afectación focal se han objetivado datos indicativos de alteraciones vasomotoras.
DesarrolloPresentamos el caso clínico y los resultados de pruebas complementarias de un varón de 42años afecto de cefalea, síndrome confusional, pleocitosis, electroencefalograma (EEG) con enlentecimiento difuso, DTC con elevación de velocidades en ambas arterias cerebrales medias y tomografía computarizada por emisión de fotón único compatible con afectación difusa de predominio hemisférico izquierdo.
ConclusionesAportamos a la literatura el primer paciente descrito que aúna síndrome de HaNDL, cuadro confusional, EEG compatible con afectación difusa y DTC con aceleración de velocidades. Nuestros hallazgos sugieren una relación entre las alteraciones vasomotoras y la fisiopatología del HaNDL, y consideramos que el DTC es una herramienta útil para el diagnóstico precoz del HaNDL.
The syndrome of transient headache and neurological deficits with cerebrospinal fluid lymphocytosis (HaNDL syndrome), also known as pseudomigraine with pleocytosis, is characterised by episodes of moderate to severe headache lasting several hours, with concurrent or subsequent transient neurological symptoms.1 The episodes are closely linked to CSF pleocytosis and resolve within 3 months.1 Predominantly lymphocytic pleocytosis (>15 cells/μL) and normal complementary test results (neuroimaging studies, CSF cultures, etc.) are included among the diagnostic criteria, but are not essential for diagnosis.1 The initial manifestation resembles that of several other diseases2–10; complementary testing is therefore necessary to rule out these conditions. Focal sensory symptoms (affecting 78% of patients), aphasia (66%), and motor symptoms (56%) constitute the most frequent clinical manifestations of HaNDL syndrome. Visual alterations are infrequent (18%)11; basilar involvement is even rarer.12 Diffuse alterations or confusional symptoms have rarely been reported as the initial manifestation of the syndrome.11,13–23
Few articles have described the use of transcranial Doppler ultrasonography (TDU) to detect vasomotor changes in these patients.24,25 The cases described in the literature presented symptoms compatible with focal deficits.24,25
We present the case of a patient eventually diagnosed with HaNDL syndrome, whose complementary test results, especially those from TDU, underscore the importance of vasomotor changes in the pathophysiology of the syndrome. We also reviewed the literature on the topic and propose TDU as the diagnostic technique of choice for HaNDL syndrome.
Patients and methodsOur patient, a 42-year-old man, was a frequent cannabis user and occasional cocaine user; he had no history of migraine or other personal history of interest.
The patient initially came to our hospital due to sudden onset of a mild holocranial headache, language alterations in the form of paraphasia and blocking, and hypoaesthesia affecting the right side of the face and the right arm; the episode resolved within minutes. He reported consuming cannabis the day before the episode and cocaine 7 days previously.
The patient was admitted to our hospital's stroke unit and underwent a vascular study in accordance with the unit's “young stroke patient protocol.” A blood test (complete blood count; coagulation test; biochemical study; renal, liver, lipid, iron, hormonal, and immunological profile; serology study; tumour marker test) detected no alterations. A Doppler ultrasound of the supra-aortic trunks, a TDU, cranial CT scan, a transthoracic echocardiogram, and Holter electrocardiography found no alterations. After 24hours of observation, the patient was asymptomatic and was therefore discharged with a diagnosis of transient ischaemic attack (TIA) affecting the left carotid artery. Seven days after discharge, the patient used cannabis again.
Nine days after discharge, several hours after waking up, he presented intense holocranial headache and behavioural alterations, with no other neurological symptoms, requiring sedoanalgesia and intubation by emergency services staff. Upon arrival at hospital, a head CT and CT-angiography study were performed, with no relevant findings. The eye fundus examination did not reveal alterations compatible with papilloedema.
During the first few hours at the intensive care unit, the patient's temperature rose to 37.9°C; a CSF analysis revealed pleocytosis (40 leukocytes per field; 99% monocytes) and elevated protein levels (100mg/dL), with normal glucose levels. Suspecting herpes simplex encephalitis, we started treatment with aciclovir (10mg/kg/8h); treatment was discontinued 5 days later as 2 CSF polymerase chain reaction tests for herpesvirus returned negative results.
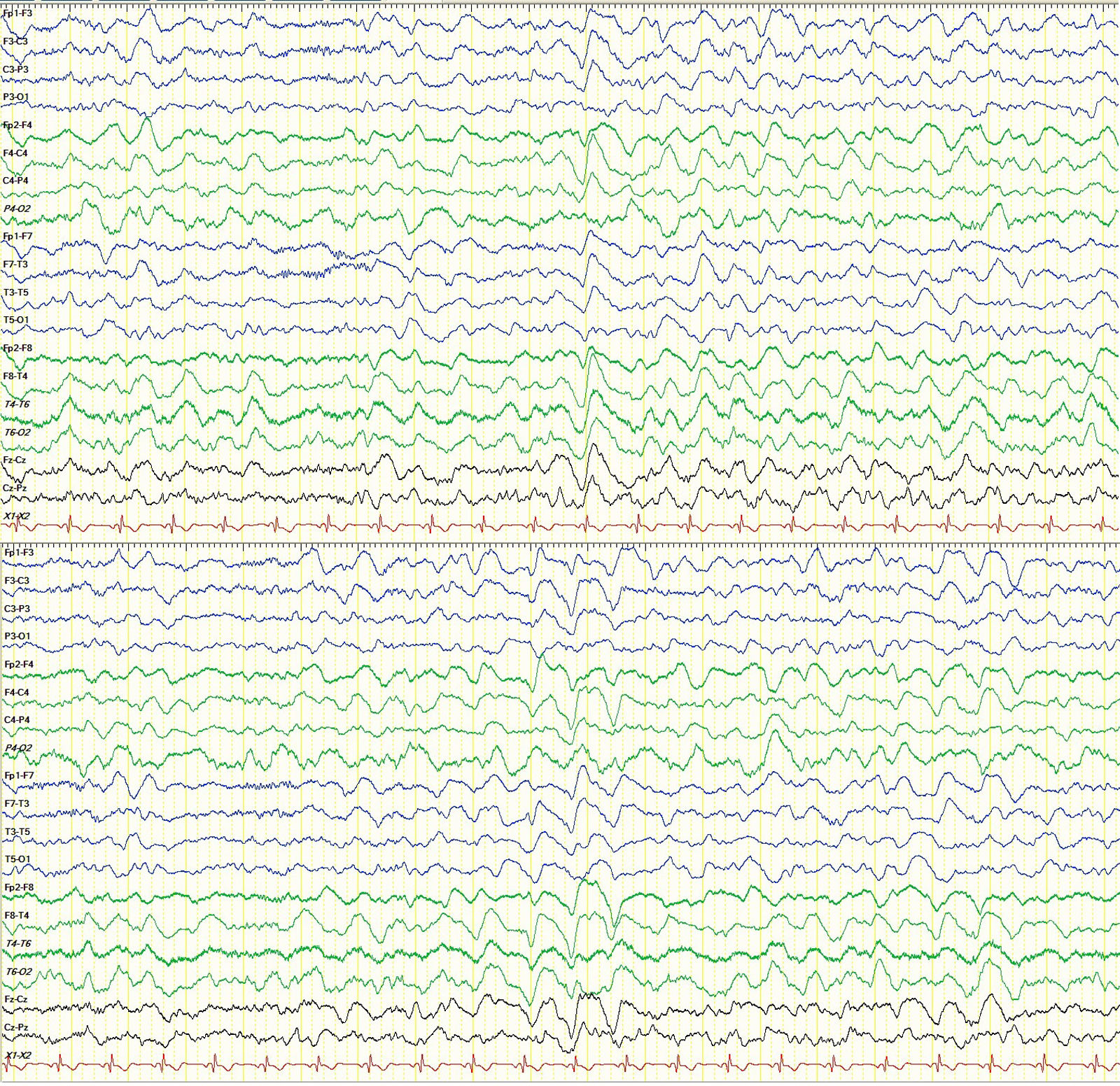
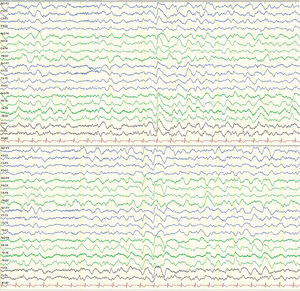
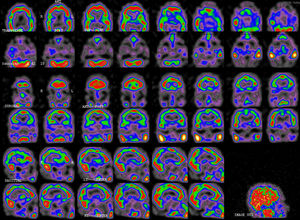
An electroencephalography study (EEG) performed the day after readmission revealed signs of diffuse encephalopathy (Fig. 1). A TDU study performed 48hours after onset of confusional symptoms revealed increased flow velocity (142cm/s) in the M1 segment of the middle cerebral artery (MCA) bilaterally, suggesting cerebral vasospasm. Nimodipine perfusion was started. A TDU study performed 4 days after treatment onset revealed normal flow velocity in both MCAs, with no other relevant findings. Nimodipine administration was discontinued.
After discontinuation of sedatives, the patient continued to display delirium with a paranoid component and occasional complex visual hallucinations.
CSF analyses performed on days 3 and 8 revealed a progressive decrease in the leucocyte count (22 and 20 leukocytes per field, respectively); protein levels remained elevated, however (66 and 138mg/dL). Serology studies for neurotropic microorganisms yielded negative results. The immunology study revealed blood-brain barrier (BBB) dysfunction with elevated IgM, IgA, and albumin levels and intrathecal IgA synthesis, with negative oligoclonal bands. The patient tested negative for onconeural antibodies and for sodium, calcium, potassium, and chloride channel receptor antibodies.
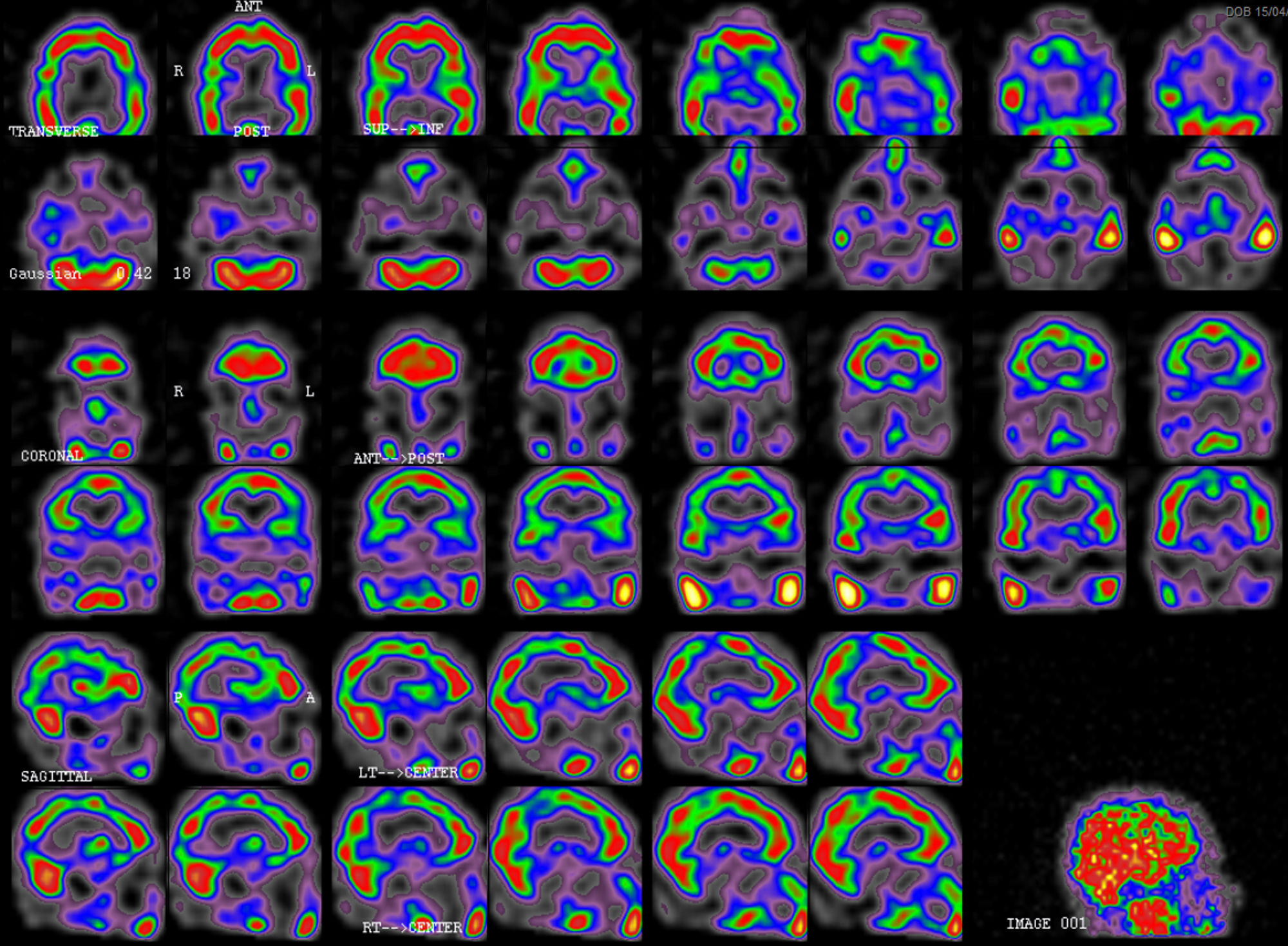
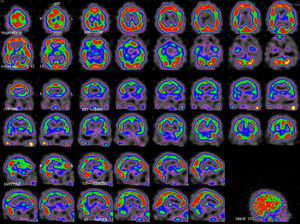
A brain MRI-angiography study performed 4 days after readmission, including diffusion sequences, showed no remarkable findings. We ruled out structural alterations compatible with posterior reversible encephalopathy syndrome. The likelihood of reversible cerebral vasoconstriction syndrome2 or vasculitis was extremely low in view of the patient's symptoms and complementary test results; angiography was therefore not performed. Given suspicion of HaNDL syndrome, a single-photon emission CT (SPECT) scan was performed 16 days after symptom onset (Fig. 2), revealing moderate temporoparietal hypoperfusion, predominantly on the left side, with mild involvement of the occipital and dorsolateral frontal cortex.
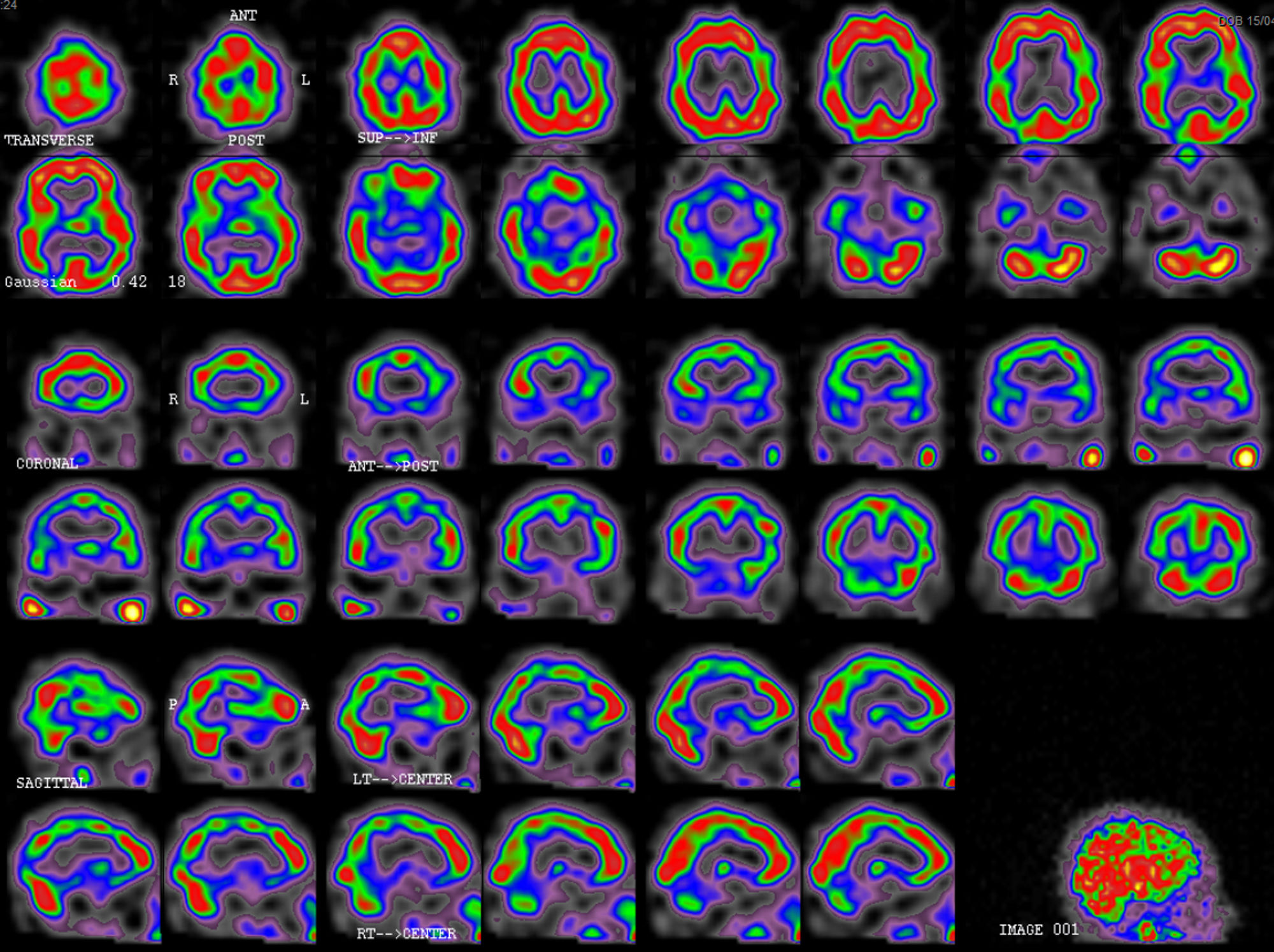
Symptoms resolved completely 13 days after admission. The patient was discharged 16 days after admission in view of symptom resolution and the suspected diagnosis of HaNDL syndrome. A follow-up SPECT scan at 2 months (Fig. 3) showed improvements in cortical perfusion; mild-to-moderate bilateral temporoparietal hypoperfusion persisted. The patient has experienced no further symptoms.
DiscussionSeveral hypotheses have attempted to explain the pathophysiology of HaNDL syndrome. The condition was initially thought to be a migraine-like phenomenon induced by CNS inflammation.26 A later hypothesis suggested that immune system activation by proinflammatory cytokine generation27,28 or production of antibodies against neuronal or vascular antigens causes leptomeningeal vasculitis associated with cortical spreading depression.29,30 Based on results from TDU24,25 and SPECT31,32 studies and cases of HaNDL syndrome following consumption of vasoconstrictive substances,4 some researchers have proposed neuronal metabolism alterations and cerebral hypoperfusion as epiphenomena of the syndrome. Hypercapnic and hypocapnic reactivity tests have detected sustained arteriolar vasolidation in some patients.25
Our case points to the involvement of 2 pathophysiological mechanisms in HaNDL syndrome. An initial episode of vasospasm may be followed by hypoperfusion, disrupting BBB function.20 These BBB alterations would then trigger an inflammatory response.20 Our patient consumed vasoconstrictive substances (cocaine,4 cannabis33) and displayed signs of vasospasm in the TDU. Furthermore, in addition to vasomotor alterations, we cannot rule out the presence of BBB alterations that may explain the inflammatory response seen in the patient's CSF. The follow-up SPECT scan showed the resolution of perfusion alterations, underscoring the major role played by vasomotor alterations in the pathophysiology of the disease.
All patients reported to date who underwent TDU studies have shown focal neurological signs. These patients display asymmetrical decreases and increases in flow velocity and pulsatility in the MCAs, supporting the presence of focal vasomotor alterations.24 Velocity changes have always been found to be associated with each patient's focal neurological signs, as also occurs with SPECT findings.31,32 Unlike in our case, the patients with diffuse involvement described in the literature did not undergo a TDU study; we are therefore unable to compare the presence of unilateral or bilateral vasomotor alterations between these patients and our own. TDU should be performed in cases of suspected HaNDL syndrome in order to: (1) confirm findings of previous TDU studies, (2) study the association between vasomotor alterations and the pathophysiology of HaNDL syndrome, and (3) study the parameters that may enable TDU to be established as a new, non-invasive diagnostic tool for suspected HaNDL syndrome. In conclusion, we have described the case of a patient with HaNDL syndrome and symptoms compatible with confusional state. Unlike in previous cases, our patient displayed EEG findings compatible with diffuse involvement and predominantly left-sided global involvement in SPECT imagery. Furthermore, ours is the first patient to undergo a TDU study during the acute phase; this study revealed elevated flow velocity in both MCAs, indicating vasospasm. Based on the literature and on our own findings, we may conclude that vasomotor alterations are involved in the pathophysiology of the syndrome. The alterations observed in our patient and in other patients described in the literature suggest that TDU is a useful tool for early diagnosis of HaNDL syndrome.
FundingThis study has received no funding of any kind.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Hidalgo de la Cruz M, Domínguez Rubio R, Luque Buzo E, Díaz Otero F, Vázquez Alén P, Orcajo Rincón J, et al. Síndrome de cefalea transitoria con déficits neurológicos asociados y pleocitosis en líquido cefalorraquídeo (HaNDL) con cuadro confusional, EEG compatible con afectación difusa y datos de vasoespasmo bilateral en estudio Doppler transcraneal: presentación de un caso y revisión de la literatura. Neurología. 2019;34:536–542.
This study was presented at the 67th Annual Meeting of the Spanish Society of Neurology in November 2015.