Primary central nervous system (CNS) lymphomas constitute a rare form of extranodal non-Hodgkin lymphomas involving the central nervous system exclusively. Primary CNS lymphomas may appear both in immunosuppressed and in immunocompetent individuals, and account for less than 2% of all intracranial tumours1,2; they are infratentorial in only 10%-20% of cases.3
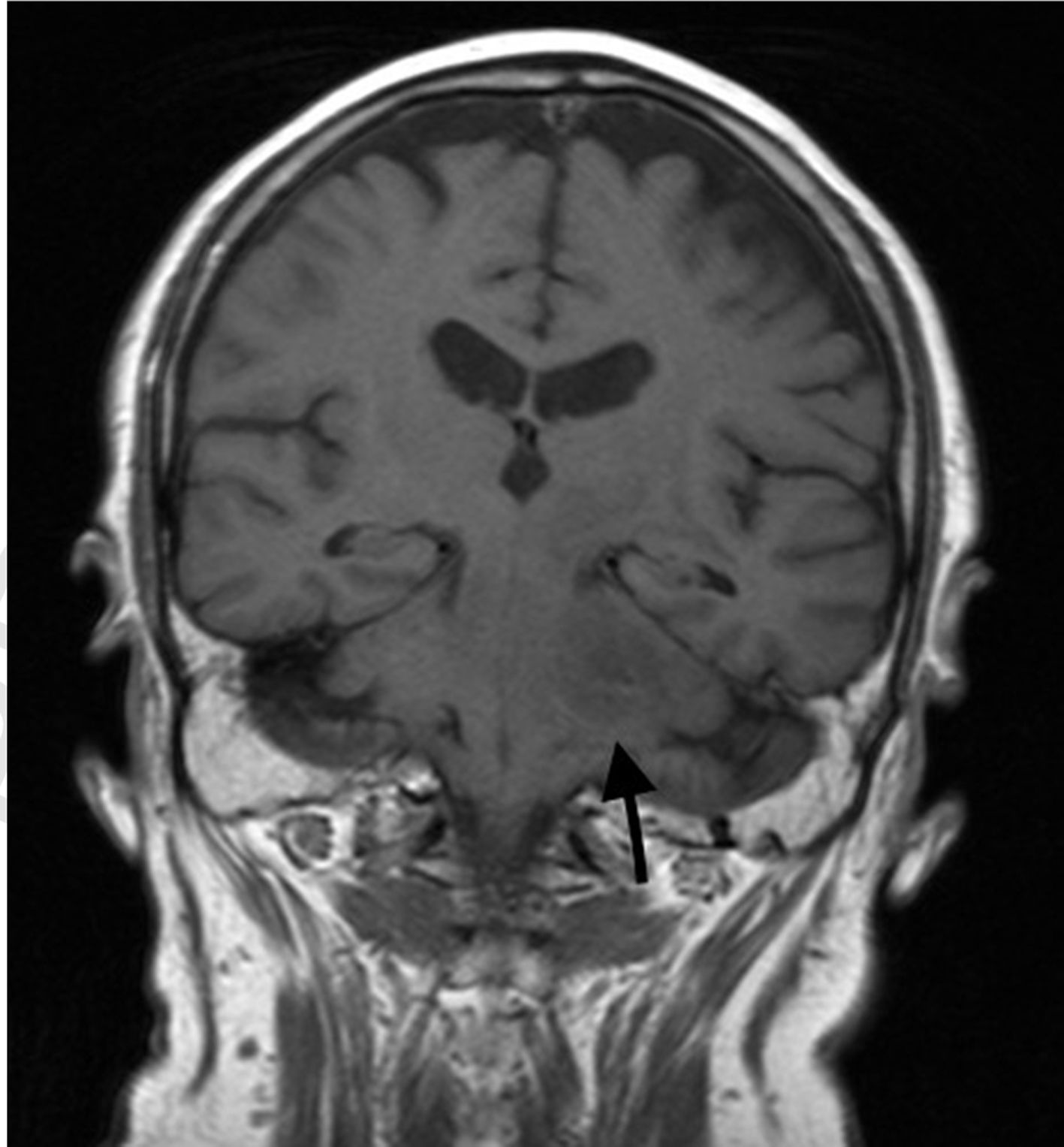
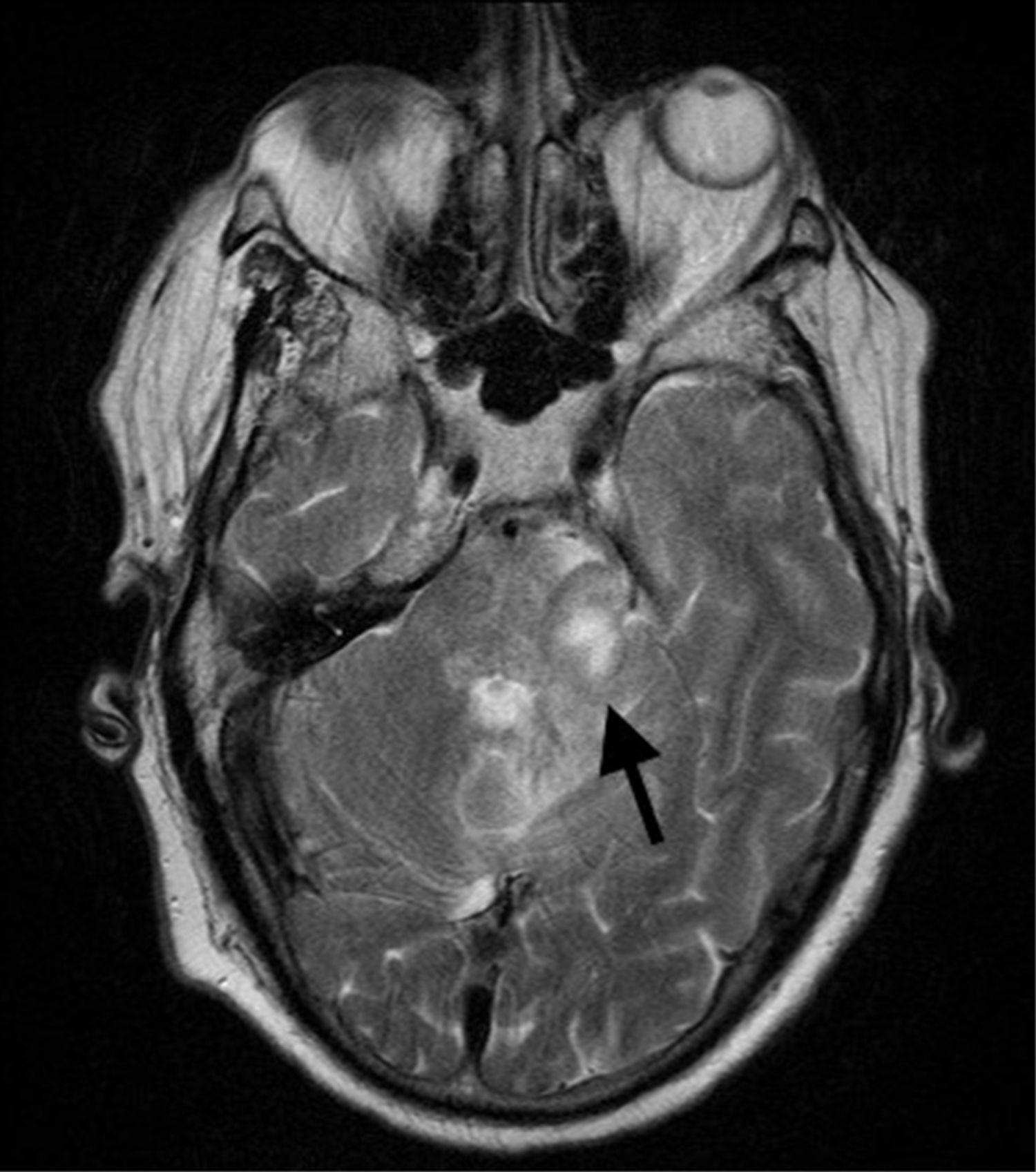
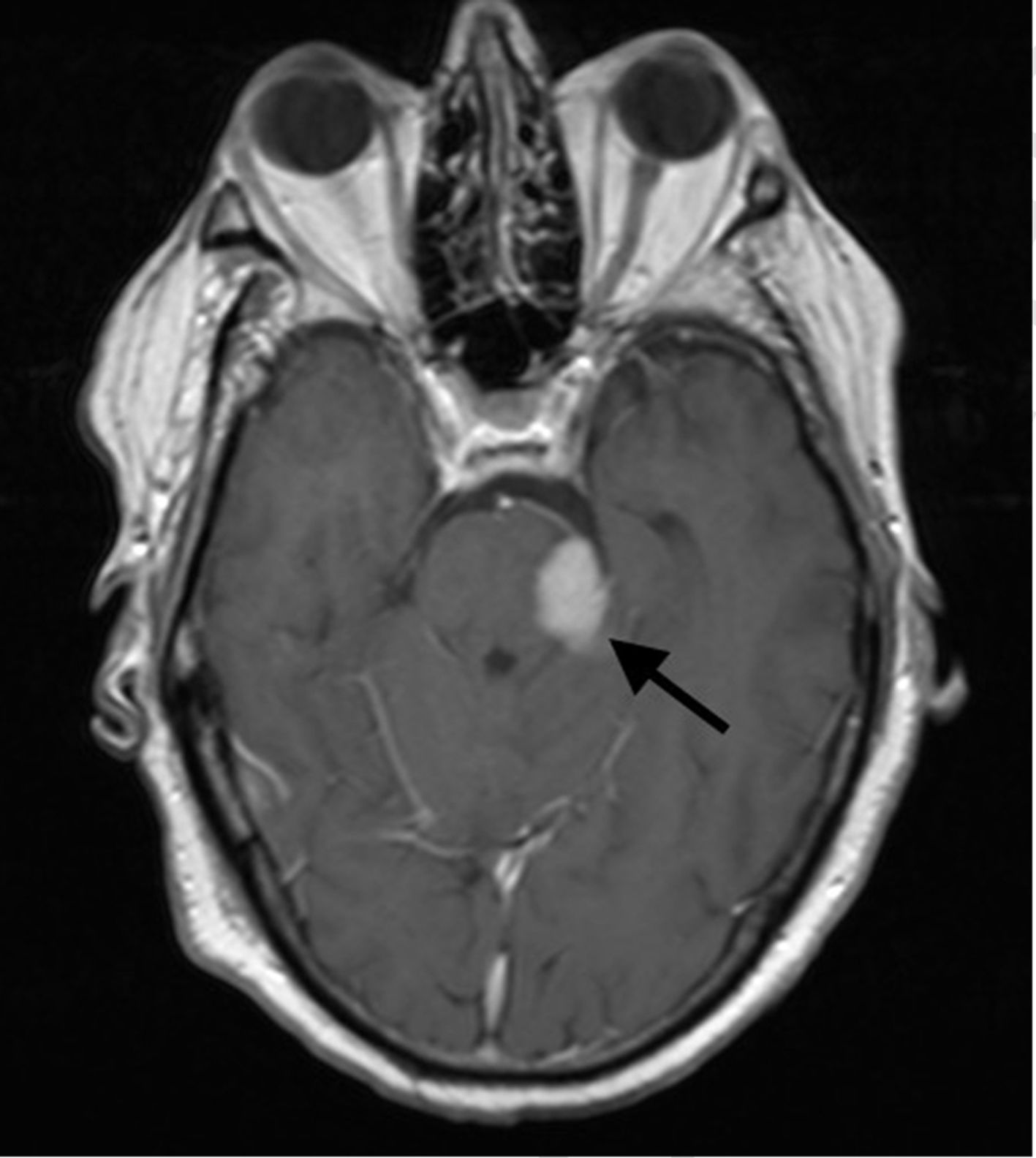
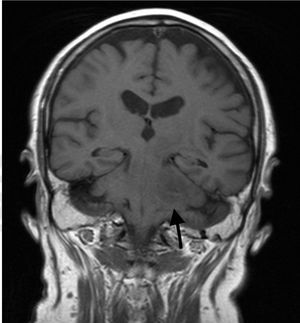
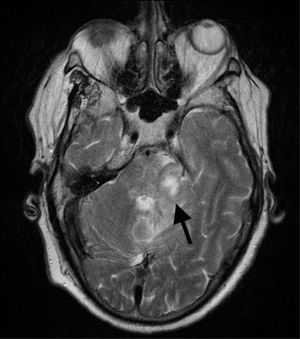
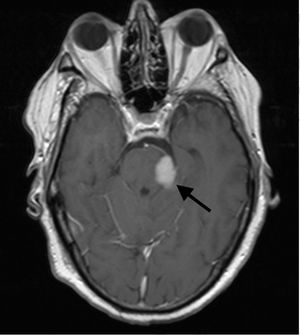
Clinical caseOur patient was a 60-year-old man, with no relevant medical history except for left-sided hearing loss, developing over the course of several months. The patient came to our hospital due to a 4-week history of subacute left-sided facial paraesthesia and hypoaesthesia, mild ataxic gait with a tendency to sway to the right, and worsening of hearing loss. The patient had not lost weight, and a complete blood count did not indicate anaemia or any other relevant alteration. A brain MRI scan (Figs. 1–3) revealed an expansive lesion in the left cerebellopontine angle (CPA), measuring 20×20×15mm (CC×AP×T); the lesion was nodular, extra-axial, hypointense on T1-weighted sequences, and moderately hyperintense on T2-weighted and FLAIR sequences. We observed perilesional oedema extending across the cerebellar peduncle to the left cerebellar hemisphere, left side of the pons and midbrain, and left cerebral peduncle. The whole area displayed intense, homogeneous gadolinium uptake. We considered several diagnostic possibilities, including vestibular schwannoma, meningioma, and metastasis, and the less likely diagnoses of vascular malformation, abscess, or chronic granulomatous disease. Further testing, including tumour markers and a chest and abdomen CT scan, showed no signs of malignancy or alterations in the lymph nodes; treatment was started with moderate doses of oral corticosteroids (0.5mg/kg/day). Despite initial improvement, symptoms reappeared and worsened after corticosteroid dosage was reduced. The patient was readmitted for evaluation of his eligibility for surgery. In addition to the symptoms mentioned above, our patient displayed left-sided peripheral facial paralysis (House–Brackmann grade III), persistent horizontal nystagmus, left-limb dysmetria, moderate dysarthria, global hyperreflexia, and marked ataxic gait. A complete blood count revealed mild macrocytic anaemia. Serology tests for HBV, HCV, and HIV yielded negative results. An MRI scan performed 3 months after the first scan showed that the lesion had increased in size (27×18×26mm), displayed similar characteristics, and exerted a more pronounced mass effect on the medulla oblongata and pons. The patient underwent surgery, given his clinical and radiological progression. The lesion was found to have originated in the pons. Anatomical pathology revealed proliferation of large, irregular lymphoid cells following a diffuse pattern, predominantly surrounding blood vessels but without infiltration; areas of necrosis; and a proliferation index >90%. The immunohistochemical study yielded positive results for CD10 and BCL6 and negative results for ALK; these findings are compatible with primary diffuse large B-cell lymphoma of the CNS. To date, 6 months after symptom onset, the patient has received 3 cycles of chemotherapy (carmustine, methotrexate, cytarabine, and rituximab), experiencing several adverse reactions; gait instability persists.
Differential diagnosis of masses in the CPA should include vestibular schwannoma (70%-80%), meningioma (5%-10%), and epidermoid cyst (5%-7%). Primary CNS lymphomas presenting as a mass in the CPA are extremely rare. MRI is the technique of choice for studying these masses. It reveals intense, homogeneous contrast uptake, as in the case presented here. Marked response to corticosteroids is also characteristic of these tumours. To our knowledge, the literature includes only 16 cases of primary CNS lymphomas appearing as masses in the CPA.4–10
FundingThe study has not received any public or private funding.
Please cite this article as: Berrocal-Izquierdo N, Muñoz F, Bosch J, Molet J. Linfoma primario del sistema nervioso central aparentado lesión del ángulo pontocerebeloso. Neurología. 2018;33:614–616.