A disease of unknown aetiology, Alzheimer's disease (AD) is the most common type of dementia. As the elderly population grows worldwide, the number of patients with AD also increases rapidly. The aim of this meta-analysis is to evaluate the prevalence and incidence of AD in Europe.
MethodologyWe conducted a literature search on Medline, Scopus, and CINAHL Complete using the keywords “Alzheimer”, “Alzheimer's disease”, and “AD” combined with “prevalence”, “incidence”, and “epidemiology”. A Bayesian random effects model with 95% credible intervals was used. The I2 statistic was applied to assess heterogeneity.
ResultsThe prevalence of Alzheimer's disease in Europe was estimated at 5.05% (95% CI, 4.73-5.39). The prevalence in men was 3.31% (95% CI, 2.85-3.80) and in women, 7.13% (95% CI, 6.56-7.72), and increased with age.
The incidence of Alzheimer's disease in Europe was 11.08 per 1000 person-years (95% CI, 10.30-11.89). Broken down by sex, it was 7.02 per 1000 person-years (95% CI, 6.06-8.05) in men and 13.25 per 1000 person-years (95% CI, 12.05-14.51) in women; again these rates increased with age.
ConclusionsThe results of our meta-analysis allow a better grasp of the impact of this disease in Europe.
La enfermedad de Alzheimer es el principal tipo de demencia y una enfermedad de etiología desconocida. Con el aumento de la población anciana mundial, el número de pacientes con enfermedad de Alzheimer muestra una tendencia de crecimiento rápido. El objetivo de este metaanálisis es evaluar la prevalencia e incidencia de la enfermedad de Alzheimer en Europa.
MetodologíaLa búsqueda de artículos se realizó en las bases de datos Medline, Scopus y CINAHL Complete utilizando las palabras claves «Alzheimer», «Alzheimer's disease» y «AD», combinadas con «prevalence», «incidence» y «epidemiology». Se utilizó el modelo bayesiano de efectos aleatorios, mostrando intervalos de credibilidad del 95%. Para estimar la heterogeneidad se usó el estadístico I2.
ResultadosLa prevalencia de enfermedad de Alzheimer en Europa fue 5,05% (IC del 95%, 4,73-5,39). La prevalencia por sexo en los hombres y las mujeres fue 3,31% (IC del 95%, 2,85-3,80) y 7,13% (IC del 95%, 6,56-7,72), respectivamente, y se encontró una tendencia creciente por grupos de edad.
La incidencia de enfermedad de Alzheimer en Europa fue 11,08 por 1.000 personas-año (IC del 95%, 10,30-11,89), siendo en los hombres y las mujeres de 7,02 por 1.000 personas-año (IC del 95%, 6,06-8,05) y 13,25 por 1.000 personas-año (IC del 95%, 12,05-14,51), respectivamente, con igual tendencia creciente con el aumento de la edad.
ConclusionesLos resultados del metaanálisis permiten una mejor comprensión de la enfermedad y su impacto en Europa.
The World Health Organization defines Alzheimer disease (AD) as a neurodegenerative disease of unknown aetiology, characterised by progressive memory and cognitive impairment1 which accounts for 50% to 75% of all cases of dementia.2 According to global statistical data from the Global Burden of Disease Study, AD was one of the fastest-rising diseases among the leading 50 causes of global years of life lost between 1990 and 2013.3
Multiple risk factors have been identified, including female sex,4 age,5 low education level,5,6 the APOE*E4 allele,7,8 smoking,9 obesity,10,11 and diabetes mellitus.12
A collaborative study including the results of several European population-based cohorts conducted in the 1990s found a prevalence of 4.4% in people older than 65.13 Rapid population ageing has resulted in an increasing number of patients with AD. In 2006, a total of 26.6 million patients had AD worldwide, with forecasts suggesting that this number will reach 106.8 million by 2050, with 16.51 million patients in Europe.14 More recent studies have confirmed this upward trend in the incidence of dementia, predicting a 87% increase in Europe for the 2010-2050 period.15
A deeper understanding of the epidemiology of AD is therefore important for early prevention, as it helps healthcare authorities and reduces the impact of the disease on the elderly. This meta-analysis aims to analyse the available literature and estimate the prevalence and incidence of AD in Europe.
Material and methodsSearch strategy and selection criteriaWe searched the MEDLINE, SCOPUS, and CINAHL Complete databases for articles published between 1 January 1995 and 31 March 2015 and written in English, Spanish, French, Italian, or Portuguese.
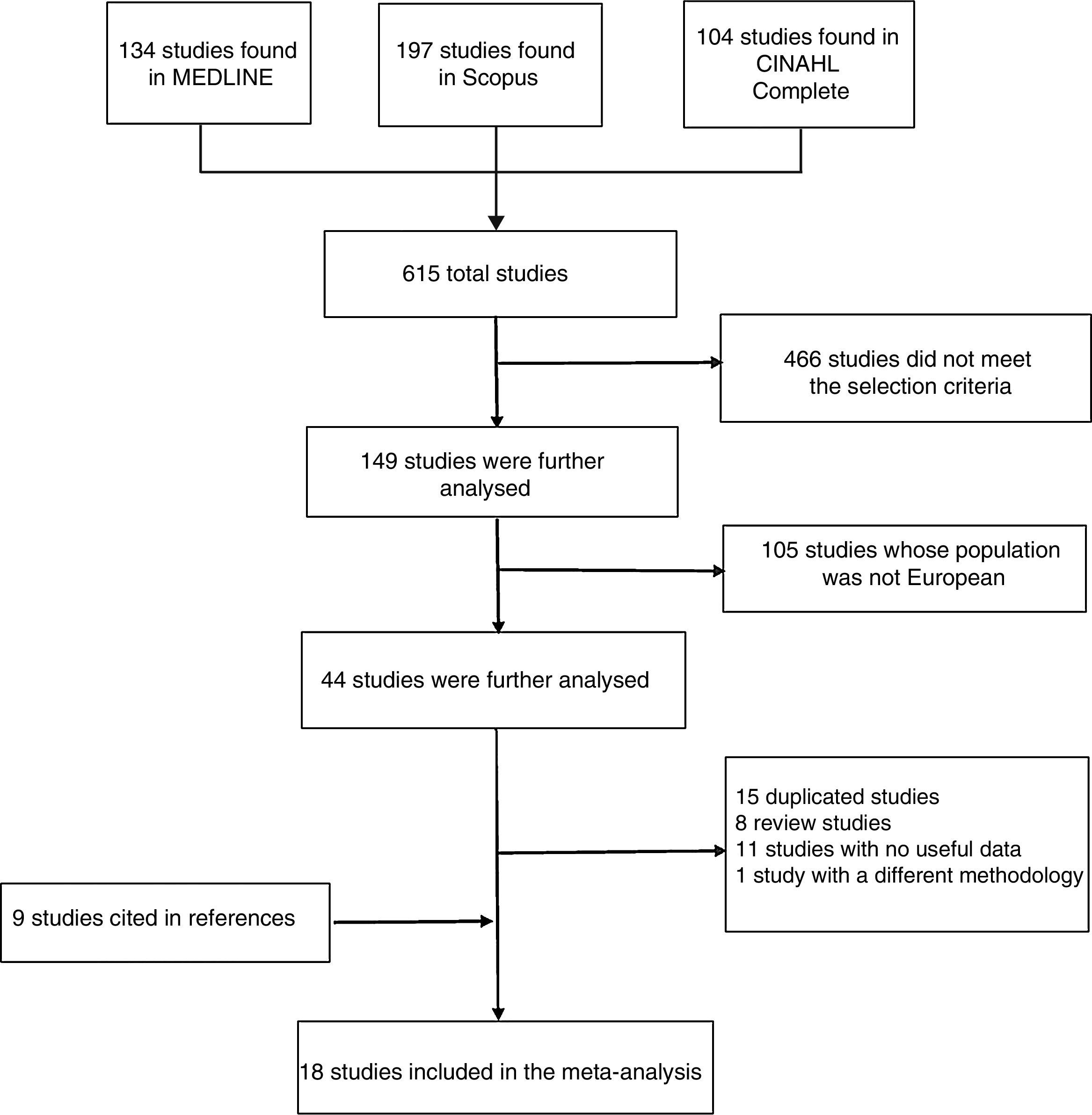
We searched by title using the following keywords: “Alzheimer”, “Alzheimer's disease”, and “AD”, combined with “prevalence”, “incidence”, and “epidemiology”. A total of 615 articles were gathered. Additionally, we reviewed the references cited by the selected articles to identify additional studies meeting our inclusion criteria. Two researchers (H.N. and I.A.A.) searched for and assessed the articles; any discrepancies were solved by consensus.
Our meta-analysis included all observational studies fulfilling the following criteria: 1) original articles; 2) including European populations; 3) participants were men and women older than 50; 4) providing original data on prevalence and/or incidence; 5) describing diagnosis of AD, and 6) available in full text. Review articles, meta-analyses, and studies not addressing the epidemiology of AD were excluded.
Data extractionData were extracted by 2 researchers (H.N. and I.A.A.) and discrepancies were resolved through consultation with a third researcher (F.G.G.). The meta-analysis included the following data from each article: 1) surname of the first author, year of publication, country of the study population; 2) demographic characteristics (number of participants, age range); 3) mean follow-up time; 4) number of patients with AD used to calculate the prevalence; 5) patients with AD and person-years at risk used to calculate the incidence.
Quantitative analysis (meta-analysis)Separate meta-analyses were conducted for prevalence and incidence. We used Fast*Pro software and a Bayesian random-effects model with a 95% credible interval (95% CI). Bayesian credible intervals are different from frequentist confidence intervals: a 95% credible interval indicates that the probability that the true value lies within the interval is 95% according to the data observed and prior belief, whereas a 95% confidence interval indicates that 95% of the intervals would include the true value if numerous samples were taken. We conducted sensitivity analyses, replicating the results after excluding one study to examine the robustness of the analysis and the influence of the excluded study.
Heterogeneity was assessed with I2, a statistic that estimates the percentage of total variation due to heterogeneity across studies.16
Brayne et al.19 and Andersen et al.27 used patient and person-years data from patients with minimal and greater severity AD, and very mild to severe AD, respectively. The study by Copeland et al.28 calculated patient and person-years at risk based on data from women and men of all ages. We included the study by Tsolaki et al.26 in the meta-analyses of the prevalence and incidence of AD.
ResultsThe MEDLINE search yielded 314 articles; 239 articles were excluded for not meeting the selection criteria and the remaining 75 articles required further analysis. Of these, 48 were excluded because they did not include European populations. Of the remaining 27 studies, we excluded 7 review articles, 11 articles whose data were not useful, and one study with a different research methodology. Our meta-analysis included 8 articles from MEDLINE.
We found 197 articles in Scopus; 143 of these were excluded for not fulfilling the selection criteria, and an additional 39 articles were excluded because their populations were not European. Of the remaining 15 studies, we excluded one review article, 4 articles whose data were not useful, and one study with a different research methodology. The remaining 9 articles met all the criteria. However, 8 of these were duplicated and were therefore excluded. As a result, only one article from Scopus was included in our meta-analysis.
The CINAHL Complete literature search yielded 104 articles; 84 of these did not meet the criteria and 18 did not include European populations. Two articles required further analysis: one of them was a review article and the other followed an incompatible methodology. No studies from CINAHL Complete were therefore included in our meta-analysis.
After reading the included articles, we identified and added 9 new articles cited in their reference lists; our meta-analysis finally included a total of 18 original articles (Fig. 1). As an exception, we included the study by Letenneur et al.17 for its importance as part of the EURODEM study.35
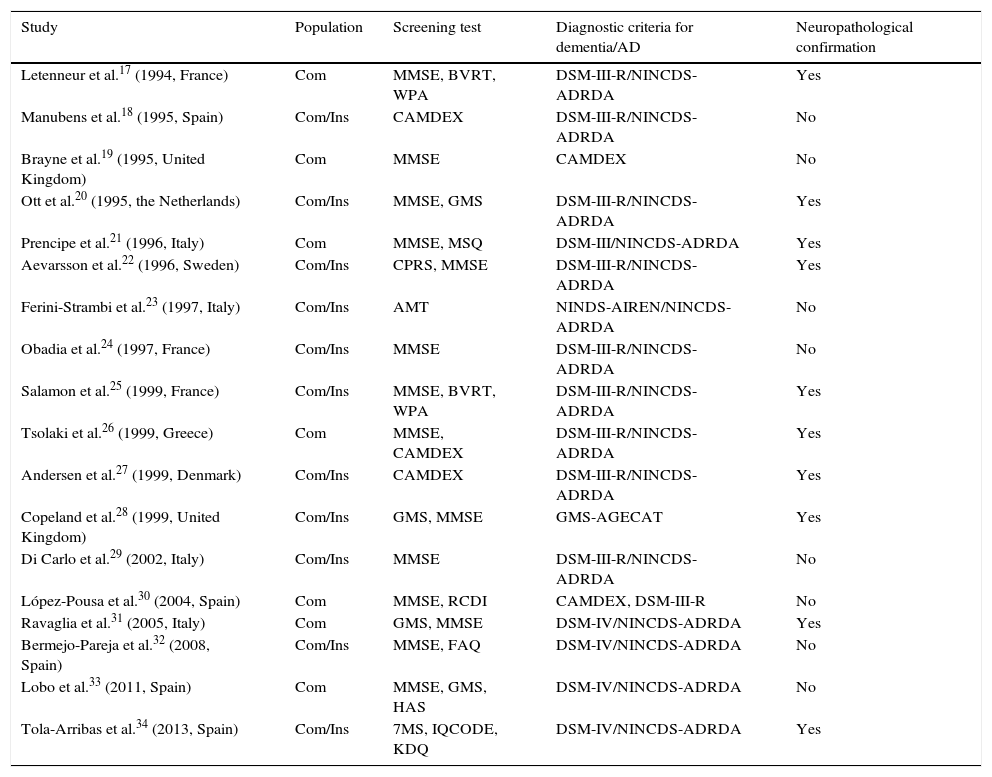
Study characteristics are listed in Table 1. Our selection of articles included 8 observational cross-sectional studies, which were included in the meta-analysis of prevalence (Table 2), and 11 longitudinal or cohort studies, which were used for the meta-analysis of incidence (Table 3). The study by Tsolaki et al.26 was used in both meta-analyses, given that it was cross-sectional and longitudinal.
Characteristics of the included studies.
| Study | Population | Screening test | Diagnostic criteria for dementia/AD | Neuropathological confirmation |
|---|---|---|---|---|
| Letenneur et al.17 (1994, France) | Com | MMSE, BVRT, WPA | DSM-III-R/NINCDS-ADRDA | Yes |
| Manubens et al.18 (1995, Spain) | Com/Ins | CAMDEX | DSM-III-R/NINCDS-ADRDA | No |
| Brayne et al.19 (1995, United Kingdom) | Com | MMSE | CAMDEX | No |
| Ott et al.20 (1995, the Netherlands) | Com/Ins | MMSE, GMS | DSM-III-R/NINCDS-ADRDA | Yes |
| Prencipe et al.21 (1996, Italy) | Com | MMSE, MSQ | DSM-III/NINCDS-ADRDA | Yes |
| Aevarsson et al.22 (1996, Sweden) | Com/Ins | CPRS, MMSE | DSM-III-R/NINCDS-ADRDA | Yes |
| Ferini-Strambi et al.23 (1997, Italy) | Com/Ins | AMT | NINDS-AIREN/NINCDS-ADRDA | No |
| Obadia et al.24 (1997, France) | Com/Ins | MMSE | DSM-III-R/NINCDS-ADRDA | No |
| Salamon et al.25 (1999, France) | Com/Ins | MMSE, BVRT, WPA | DSM-III-R/NINCDS-ADRDA | Yes |
| Tsolaki et al.26 (1999, Greece) | Com | MMSE, CAMDEX | DSM-III-R/NINCDS-ADRDA | Yes |
| Andersen et al.27 (1999, Denmark) | Com/Ins | CAMDEX | DSM-III-R/NINCDS-ADRDA | Yes |
| Copeland et al.28 (1999, United Kingdom) | Com/Ins | GMS, MMSE | GMS-AGECAT | Yes |
| Di Carlo et al.29 (2002, Italy) | Com/Ins | MMSE | DSM-III-R/NINCDS-ADRDA | No |
| López-Pousa et al.30 (2004, Spain) | Com | MMSE, RCDI | CAMDEX, DSM-III-R | No |
| Ravaglia et al.31 (2005, Italy) | Com | GMS, MMSE | DSM-IV/NINCDS-ADRDA | Yes |
| Bermejo-Pareja et al.32 (2008, Spain) | Com/Ins | MMSE, FAQ | DSM-IV/NINCDS-ADRDA | No |
| Lobo et al.33 (2011, Spain) | Com | MMSE, GMS, HAS | DSM-IV/NINCDS-ADRDA | No |
| Tola-Arribas et al.34 (2013, Spain) | Com/Ins | 7MS, IQCODE, KDQ | DSM-IV/NINCDS-ADRDA | Yes |
AGECAT: Automated Geriatric Examination for Computer Assisted Taxonomy; AMT: Abbreviated Mental Test; BVRT: Benton Visual Retention Test; CAMDEX: Cambridge Mental Disorders of the Elderly Examination; Com: community-living patients; CPRS: Comprehensive Psychopathological Rating Scale; DSM: Diagnostic and Statistical Manual of Mental Disorders; FAQ: Functional Activities Questionnaire; GDS: Geriatric Depression Scale; GMS: Geriatric Mental State; HAS: History and Aetiology Schedule; Ins: institutionalised patients; IQCODE: Informant Questionnaire on Cognitive Decline in the Elderly; KDQ: Kawas Dementia Questionnaire; MMSE: Mini–Mental State Examination; MSQ: Mental Status Questionnaire; NINCDS-ADRDA: National Institute of Neurological and Communicative Disorders and Stroke-Alzheimer's Disease and Related Disorders Association; NINDS-AIREN: National Institute of Neurological Disorders and Stroke-Association Internationale pour la Recherche et l’Enseignement en Neurosciences; RCDI: Retrospective Collateral Dementia Interview; WPA: Wechsler's Paired-Associates; 7MS: 7-Minute Screen Neurocognitive Battery.
Sources: Folstein et al.,36 Benton,37 Wechsler,38 Roth et al.,39 Copeland et al.,40 Copeland et al.,41 Kahn et al.,42 Asberg et al.,43 Rocca et al.,44 Davis et al.,45 Yesavage et al.,46 Pfeffer et al.,47 Dewey et al.,48 Solomon et al.,49 Jorm and Korten,50 Kawas et al.,51 American Psychiatric Association,52 American Psychiatric Association,53 McKhann et al.,54 and Roman et al.55
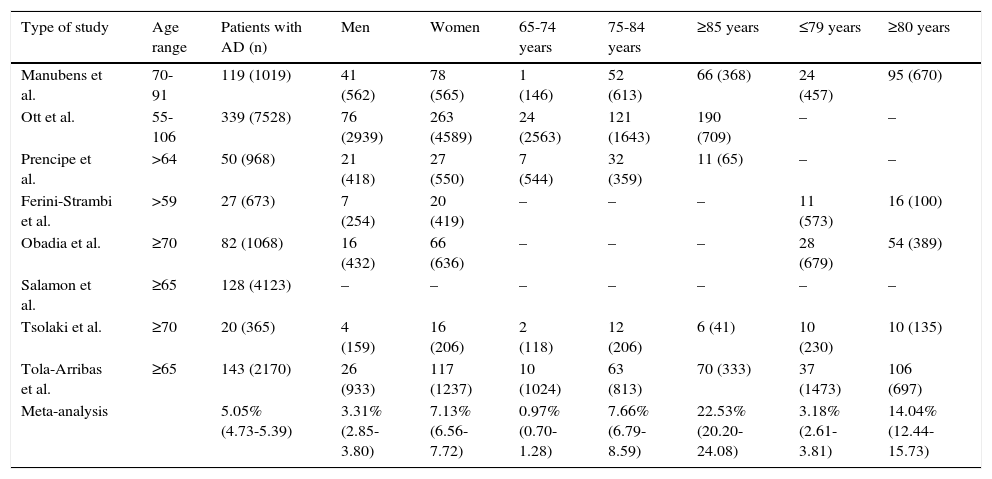
Meta-analysis of prevalence of Alzheimer disease in Europe, broken down by sex and age group.
| Type of study | Age range | Patients with AD (n) | Men | Women | 65-74 years | 75-84 years | ≥85 years | ≤79 years | ≥80 years |
|---|---|---|---|---|---|---|---|---|---|
| Manubens et al. | 70-91 | 119 (1019) | 41 (562) | 78 (565) | 1 (146) | 52 (613) | 66 (368) | 24 (457) | 95 (670) |
| Ott et al. | 55-106 | 339 (7528) | 76 (2939) | 263 (4589) | 24 (2563) | 121 (1643) | 190 (709) | – | – |
| Prencipe et al. | >64 | 50 (968) | 21 (418) | 27 (550) | 7 (544) | 32 (359) | 11 (65) | – | – |
| Ferini-Strambi et al. | >59 | 27 (673) | 7 (254) | 20 (419) | – | – | – | 11 (573) | 16 (100) |
| Obadia et al. | ≥70 | 82 (1068) | 16 (432) | 66 (636) | – | – | – | 28 (679) | 54 (389) |
| Salamon et al. | ≥65 | 128 (4123) | – | – | – | – | – | – | – |
| Tsolaki et al. | ≥70 | 20 (365) | 4 (159) | 16 (206) | 2 (118) | 12 (206) | 6 (41) | 10 (230) | 10 (135) |
| Tola-Arribas et al. | ≥65 | 143 (2170) | 26 (933) | 117 (1237) | 10 (1024) | 63 (813) | 70 (333) | 37 (1473) | 106 (697) |
| Meta-analysis | 5.05% (4.73-5.39) | 3.31% (2.85-3.80) | 7.13% (6.56-7.72) | 0.97% (0.70-1.28) | 7.66% (6.79-8.59) | 22.53% (20.20-24.08) | 3.18% (2.61-3.81) | 14.04% (12.44-15.73) |
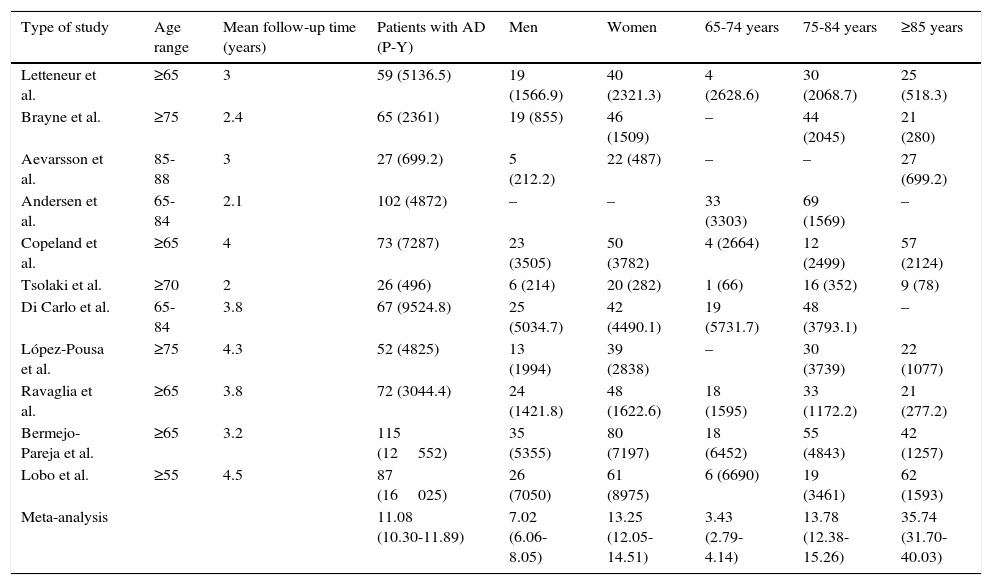
Meta-analysis of incidence of Alzheimer disease in Europe, broken down by sex and age group (person-years at risk).
| Type of study | Age range | Mean follow-up time (years) | Patients with AD (P-Y) | Men | Women | 65-74 years | 75-84 years | ≥85 years |
|---|---|---|---|---|---|---|---|---|
| Letteneur et al. | ≥65 | 3 | 59 (5136.5) | 19 (1566.9) | 40 (2321.3) | 4 (2628.6) | 30 (2068.7) | 25 (518.3) |
| Brayne et al. | ≥75 | 2.4 | 65 (2361) | 19 (855) | 46 (1509) | – | 44 (2045) | 21 (280) |
| Aevarsson et al. | 85-88 | 3 | 27 (699.2) | 5 (212.2) | 22 (487) | – | – | 27 (699.2) |
| Andersen et al. | 65-84 | 2.1 | 102 (4872) | – | – | 33 (3303) | 69 (1569) | – |
| Copeland et al. | ≥65 | 4 | 73 (7287) | 23 (3505) | 50 (3782) | 4 (2664) | 12 (2499) | 57 (2124) |
| Tsolaki et al. | ≥70 | 2 | 26 (496) | 6 (214) | 20 (282) | 1 (66) | 16 (352) | 9 (78) |
| Di Carlo et al. | 65-84 | 3.8 | 67 (9524.8) | 25 (5034.7) | 42 (4490.1) | 19 (5731.7) | 48 (3793.1) | – |
| López-Pousa et al. | ≥75 | 4.3 | 52 (4825) | 13 (1994) | 39 (2838) | – | 30 (3739) | 22 (1077) |
| Ravaglia et al. | ≥65 | 3.8 | 72 (3044.4) | 24 (1421.8) | 48 (1622.6) | 18 (1595) | 33 (1172.2) | 21 (277.2) |
| Bermejo-Pareja et al. | ≥65 | 3.2 | 115 (12552) | 35 (5355) | 80 (7197) | 18 (6452) | 55 (4843) | 42 (1257) |
| Lobo et al. | ≥55 | 4.5 | 87 (16025) | 26 (7050) | 61 (8975) | 6 (6690) | 19 (3461) | 62 (1593) |
| Meta-analysis | 11.08 (10.30-11.89) | 7.02 (6.06-8.05) | 13.25 (12.05-14.51) | 3.43 (2.79-4.14) | 13.78 (12.38-15.26) | 35.74 (31.70-40.03) |
P-Y: person-years at risk.
The populations came from the following countries: Spain, the Netherlands, Italy, France, Greece, United Kingdom, Sweden, and Denmark. Sample size ranged from 288 to 7528 participants.
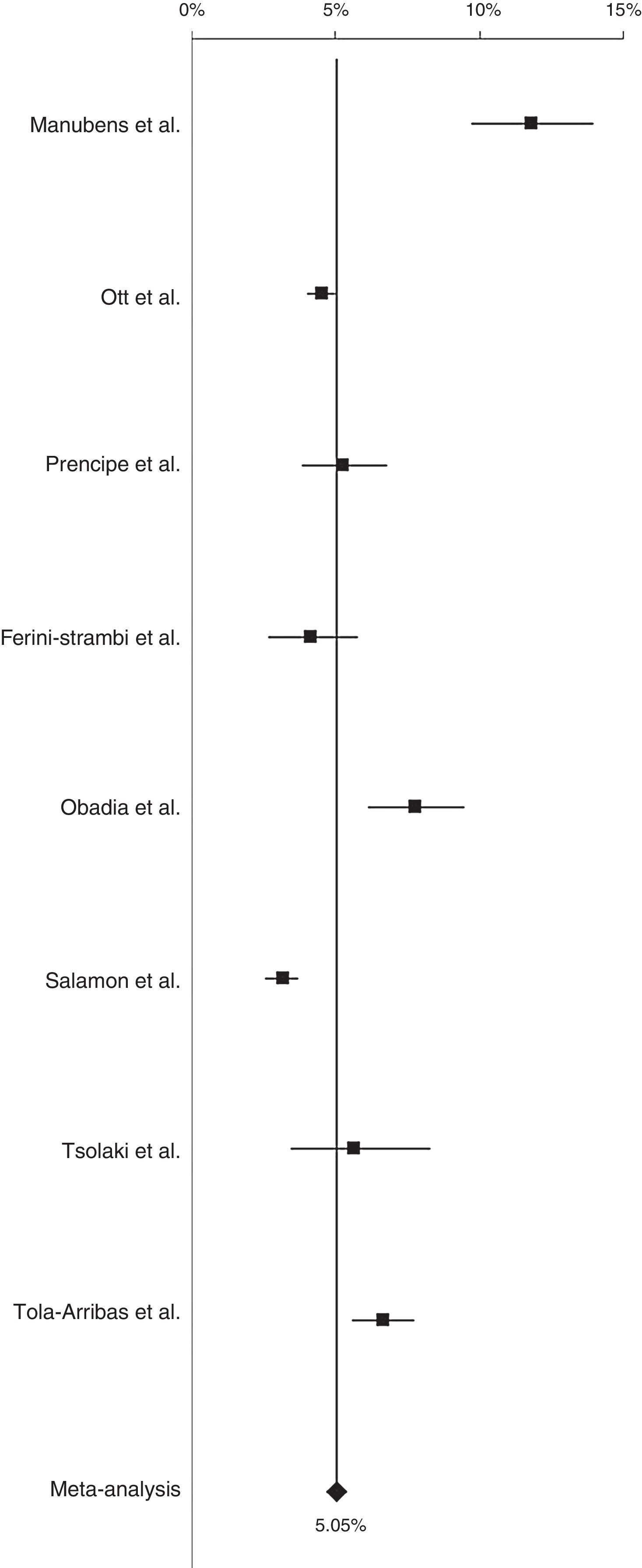
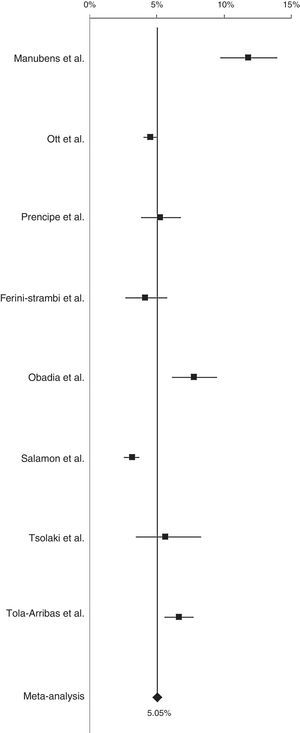
Prevalence of AD in Europe was 5.05% (95% CI, 4.73-5.39) (Fig. 2). After conducting a sensitivity analysis excluding the study by Manubens et al.18, prevalence was estimated at 4.66% (95% CI, 4.34-4.99). Prevalence of AD was 6.88% (95% CI, 6.19-7.61) in southern European countries (Spain, Italy, and Greece) and 4.31% (95% CI, 3.26-4.68) in northern European countries (France, the Netherlands).
Prevalence was 3.31% (95% CI, 2.85-3.80) in men and 7.13% (95% CI, 6.56-7.72) in women.
Prevalence of AD increased with age: 0.97%, 7.66%, and 22.53% for patients aged 65 to 74 years, 75 to 84 years, and 85 and older, respectively, and 3.18% and 14.04% for patients aged 79 and younger and those aged 80 and older, respectively (Table 2).
The heterogeneity analysis gave an I2 value of 42.42%, which indicates moderate heterogeneity. After the sensitivity analysis, I2 was 6.49%, indicating low heterogeneity; I2 values for southern and northern European countries were 28.9% and 57.40%, respectively.
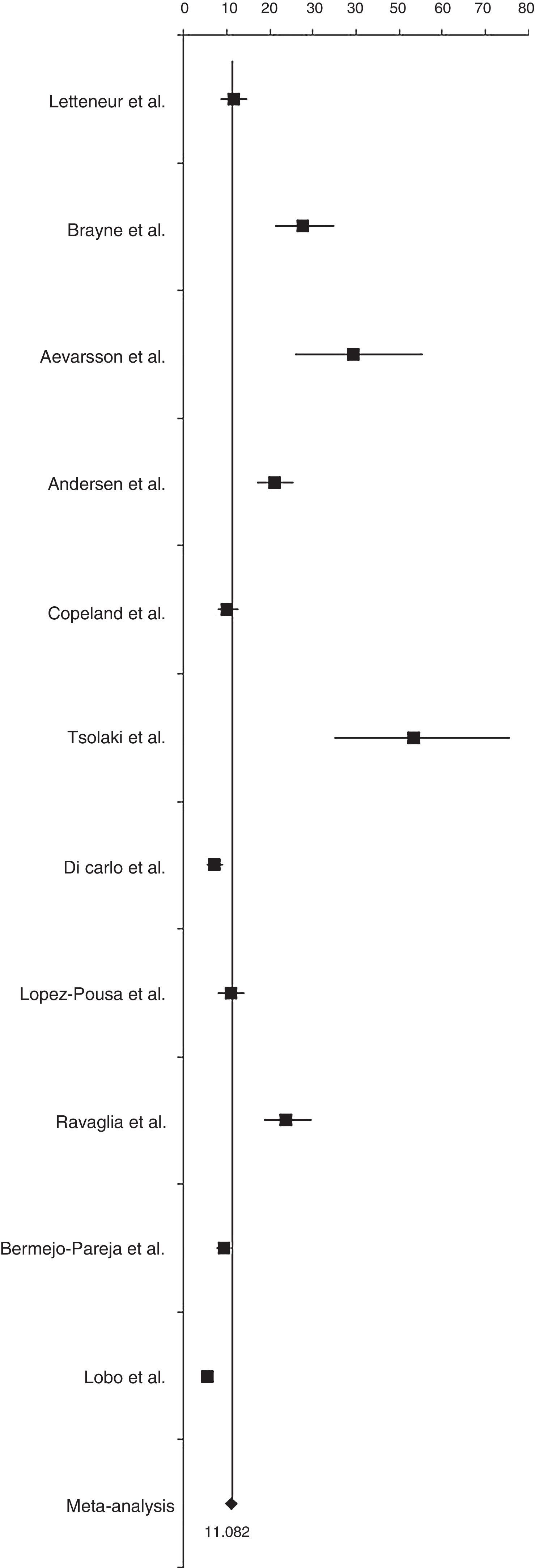
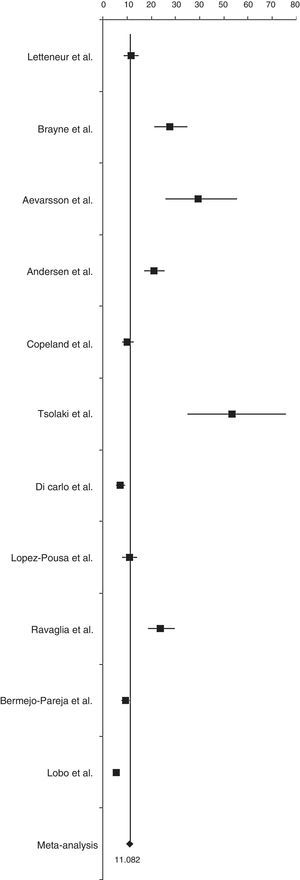
Incidence of AD was 11.08 cases per 1000 person-years (95% CI, 10.30-11.89) (Fig. 3). Sensitivity analyses, which excluded only the article by Tsolaki et al.,26 obtained an incidence rate of 10.78 cases per 1000 person-years (95% CI, 10.0-11.58). After excluding only the article by Aevarsson et al.22, incidence was estimated at 10.80 cases per 1000 person-years (95% CI, 10.02-11.60).
Incidence rates in southern European countries (Greece, Italy, and Spain) and northern European countries (France, United Kingdom, Sweden, and Denmark) were 8.97 cases per 1000 person-years (95% CI, 8.13-9.86) and 15.94 cases per 1000 person-years (95% CI, 14.25-17.72), respectively.
As with prevalence, incidence of AD was higher in women than in men: 13.25 cases per 1000 person-years (95% CI, 12.05-14.51) vs 7.02 cases per 1000 person-years (95% CI, 6.06-8.05).
Incidence increased with age: 3.43, 13.78, and 35.74 cases per 1000 person-years for patients aged 65 to 74 years, 75 to 84 years, and 85 and older, respectively (Table 3).
Heterogeneity was found to be high (I2=70.37%). After excluding the study by Tsolaki et al.26 and the study by Aevarsson et al.22from the sensitivity analysis, I2 values were estimated at 63.66% and 68.16%, respectively. In both cases, heterogeneity was high. I2 values for the incidence of AD in southern and northern European countries were 78.80% and 48.15%, respectively.
DiscussionImprovements in quality of life have led to an increase in life expectancy, which in turn involves increased incidence of ageing-related diseases. This meta-analysis estimated prevalence and incidence rates of AD in Europe.
Studies conducted in Europe showed that the age-standardised prevalence of AD was lower in patients older than 65 (4.4%),13 whereas incidence was estimated at 12.33 cases per 1000 person-years,35 a higher rate than that found in our study. Recent studies found a significant decrease in the prevalence of dementia in the United Kingdom,56 contrary to what we have observed in our study. In another study, disease prevalence was found to be stable and incidence displayed a non-significant decrease over time, which is in line with our findings.57
However, prevention of cardiovascular risk factors or higher education levels may have led to a significant decrease in the incidence of dementia in recent years.58
Our study showed a higher prevalence and incidence of AD in women, which is in line with other studies reporting a higher risk of AD in women,59,60 especially in those with lower education levels.61
In Asia, a study carried out in China showed that prevalence of AD was 1.27% in patients aged 65 to 69 years and 18.54% in those aged 85 to 89 years for the year 2010; prevalence rates for all age groups were higher in 2010 than in 1990. Incidence of AD in the population aged 60 or older was 6.25 cases per 1000 person-years.62
In Japan, prevalence of AD in patients older than 65 was 7%,63 with an incidence rate of 5.6 cases per 1000 person-years in the population older than 60.64 In South Korea, however, prevalence in the population older than 65 was 5.7%.65
These findings show that recent improvements in quality of life and living conditions, especially in China and South Korea, have led to population ageing. This, in turn, has resulted in an increase in the prevalence of age-related diseases such as AD, whose prevalence is expected to increase in the future due to lifestyle and risk factors influencing the development of dementia at advanced ages.66 Japan, on the other hand, has an older population, which may explain the higher prevalence of AD. The incidence rate is lower in Japan, however, which is probably due to the adoption of healthy lifestyle factors that may have a protective effect against AD, such as diet.67
In the United States, prevalence of AD in people older than 70 was estimated at 9.51%,68 a higher rate than that found in our study, whereas the incidence rate was 14.26 cases per 1000 person-years.69
The American population is comparable to the European population both in the proportion of elderly people and in terms of living conditions; differences may therefore be due to differences in lifestyle: some authors have associated the Mediterranean diet with a lower risk of AD, for example.70,71
Heterogeneity was found to be medium in the meta-analysis of prevalence and low in the sensitivity analysis, after excluding one study. However, the heterogeneity of incidence was found to be high and remained high with slight changes when we excluded some studies.
One of the strengths of this study is its novelty; as far as we know, no meta-analyses have been conducted to date on the prevalence and incidence of AD in Europe. Furthermore, our study provides surprising results with a high level of scientific evidence. One of our study's main limitations is the fact that we did not have access to more databases and were therefore unable to assess more articles.
In conclusion, we observed a slight increase in the prevalence of AD in Europe in the past few years and a decrease in incidence rates. These results bring our knowledge of the epidemiology of AD in Europe up to date. Similar studies and trend studies of AD in other regions of the world are also necessary.
FundingThis study received no public or private funding.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Niu H, Álvarez-Álvarez I, Guillén-Grima F, Aguinaga-Ontoso I. Prevalencia e incidencia de la enfermedad de Alzheimer en Europa: metaanálisis. Neurología. 2017;32:523–532.
This study has not been presented at the SEN's Annual Meeting or at any other conferences or congresses.