Bronchial artery embolisation (BAE) is considered the most effective and least invasive technique for the treatment of massive or recurrent haemoptysis. Surgery is the treatment of choice only in cases of chest trauma, iatrogenic pulmonary artery rupture,1 or complications from previous BAEs. The most frequent complications of BAE are transient chest pain and dysphagia, reported in 1.4%-34.5% and 0.7%-30% of cases, respectively. Other complications include postembolisation syndrome (leukocytosis, fever, pain), vascular injury (vasospasm, dissection, perforation), haematoma, and pseudoaneurysm at the puncture site.2
The most frequent neurological complication is spinal cord ischaemia secondary to embolisation of the anterior spinal artery, with involvement of the artery of Adamkiewicz in up to 6.5% of cases.2,3 A rare, puzzling complication of BAE is ischaemic stroke, most frequently affecting the vertebrobasilar territory. In a literature search, we identified 9 reported cases.4–11
We present the case of a patient treated with BAE who presented an ischaemic stroke in the territory of the posterior circulation, and review the possible pathogenic mechanisms of this phenomenon.
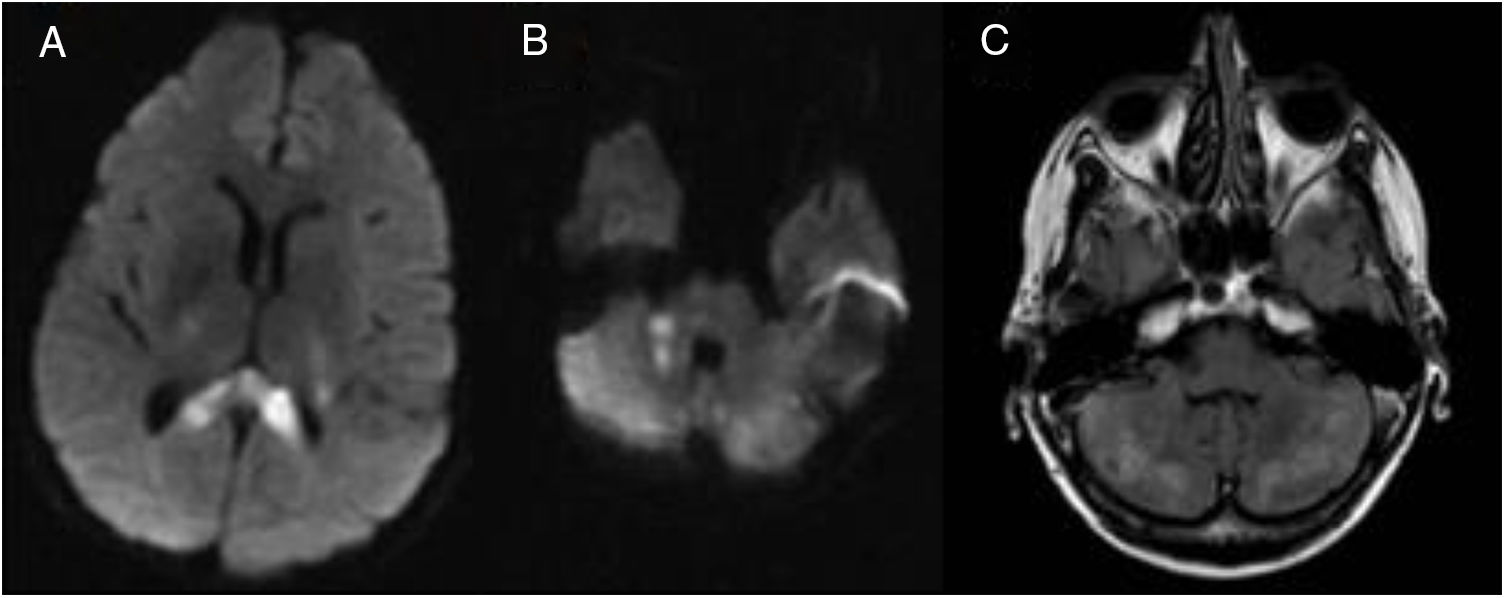
Our patient was a 57-year-old woman, a former smoker, with history of type 1 diabetes mellitus, ankylosing spondylitis, and bronchiectasis associated with recurrent haemoptysis. She had undergone BAE 3 years previously without complication. Another BAE was scheduled due to recurrence of haemoptysis. An angiography study of the bronchial arteries was carried out in order to perform selective microcatheter embolisation with 400-µm polyvinyl alcohol particles. During the procedure, the patient presented headache, nausea, vomiting, and decreased visual acuity, associated with high blood pressure (180/90 mmHg) and hyperglycaemia (400 mg/dL). After the procedure, she displayed dysarthria and ataxic gait. An emergency head CT scan revealed hypodense lesions in both cerebellar hemispheres, with no contrast uptake. A CT angiography study of the supra-aortic trunks and circle of Willis revealed no significant pathological findings or anatomical variants at the origin of the vertebral arteries. A brain MRI scan showed multiple acute ischaemic infarcts in both cerebellar hemispheres, the right middle cerebellar peduncle, and extensive areas of the splenium of the corpus callosum (Fig. 1). The remaining complementary tests (complete blood count, biochemistry study, coagulation study, electrocardiography, transthoracic echocardiography, and 24-h Holter monitoring) showed no significant alterations except for known hyperglycaemia and glycosuria. Pulmonary angiography found no vascular shunts.
Non-contrast brain MRI scan. A) Diffusion sequence showing an acute ischaemic infarct in the splenium of the corpus callosum. B) Diffusion sequence showing an acute ischaemic infarct in the right middle cerebellar peduncle. C) T2-weighted FLAIR sequence showing multiple ischaemic infarcts in both cerebellar hemispheres.
Symptoms improved during hospitalisation, but unsteady gait and subjective visual alterations persisted at discharge.
The patient has subsequently presented further episodes of mild haemoptysis, which resolved with medical treatment. Although the emboligenic source of stroke could not be identified, the pulmonology department contraindicated any further BAE due to the episode described previously, although the available literature has not established any formal contraindications.
Cerebrovascular embolism is a rare complication of BAE; some review articles report a frequency of 0.6%-2%.2
Most of the cases reported to date have been described in patients with chronic pulmonary disease, which is associated with the formation of shunts between the pulmonary and the systemic circulation; most of these cases present involvement of the posterior cerebral circulation. Several hypotheses may explain the predisposition for this territory.
The following pathogenic mechanisms have been proposed to explain intracranial embolisation in patients undergoing BAE:
- a)
Presence of collateral circulation or shunts between bronchial arteries and systemic arteries, including the vertebral and subclavian arteries
- b)
Anatomical variations of the origin of the vertebral arteries
- c)
Paradoxical embolism secondary to arteriovenous shunt between the pulmonary arteries and the pulmonary microcirculation or to intracardiac communication.4,11
Only the first 2 mechanisms may explain a predisposition for the vertebrobasilar territory.
Our patient presented multiple infarcts in areas dependent on the posterior circulation, and had underlying chronic pulmonary disease. However, no pulmonary shunts, anatomical variations of the origin of the vertebral arteries, or intracardiac communication were observed; therefore, the source of the emboli could not be identified.
Please cite this article as: Calle Calle R, Triguero Cueva L, Espigares Molero A, Maestre Moreno JF. Ictus isquémico en territorio posterior como complicación de embolización de arterias bronquiales. Neurología. 2020;35:588–589.