Anaesthetic blocks, whether used alone or combined with other treatments, are a therapeutic resource for many patients with headaches. However, usage patterns by different professionals show significant heterogeneity.
Material and methodsThe Headache Study Group of the Spanish Society of Neurology (GECSEN) designed a self-administered cross-sectional survey and sent it to all group members through the SEN's scientific area web platform in February 2016. The objective was to ascertain the main technical and formal aspects of this procedure and compare them with data obtained in a similar survey conducted in 2012.
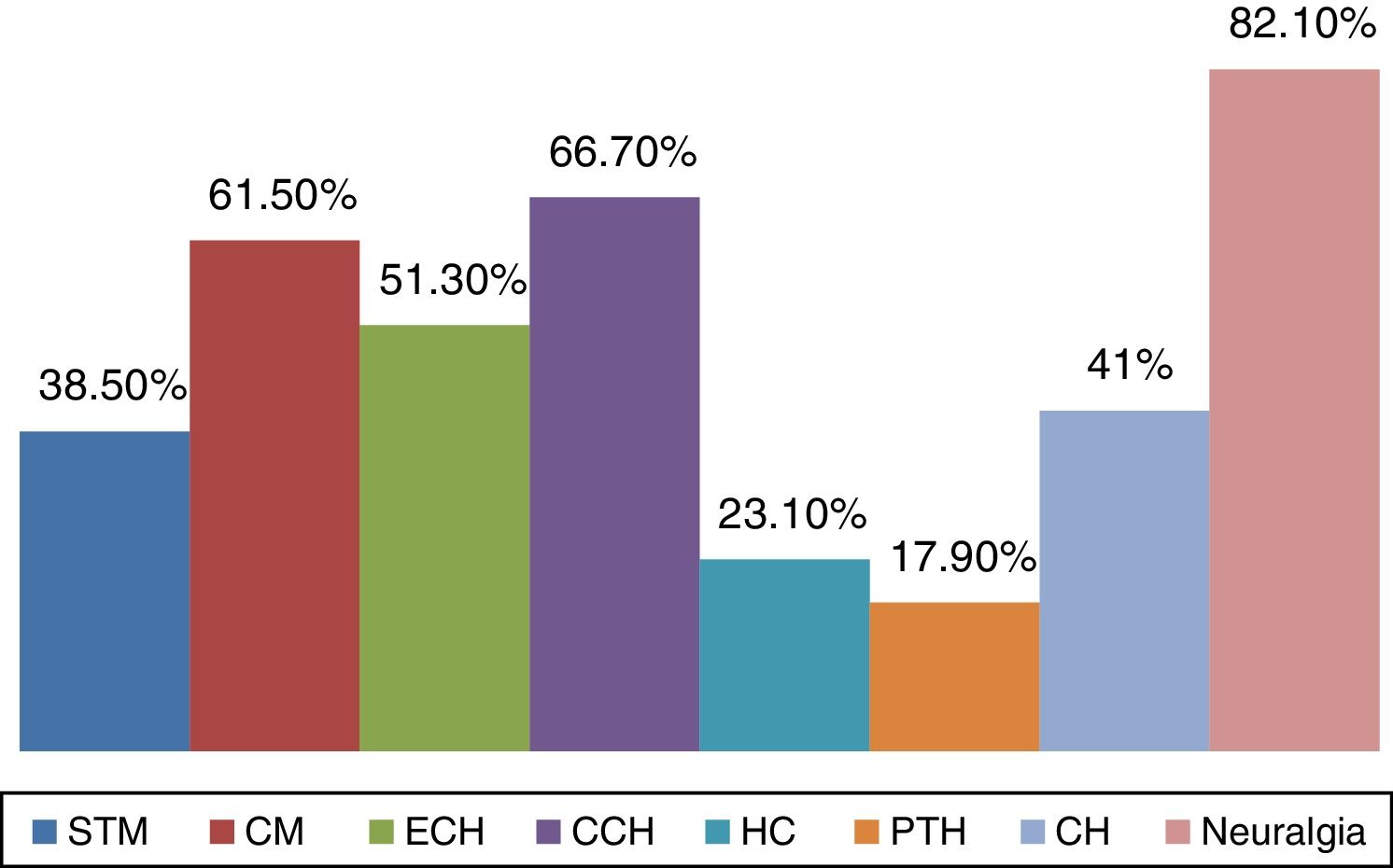
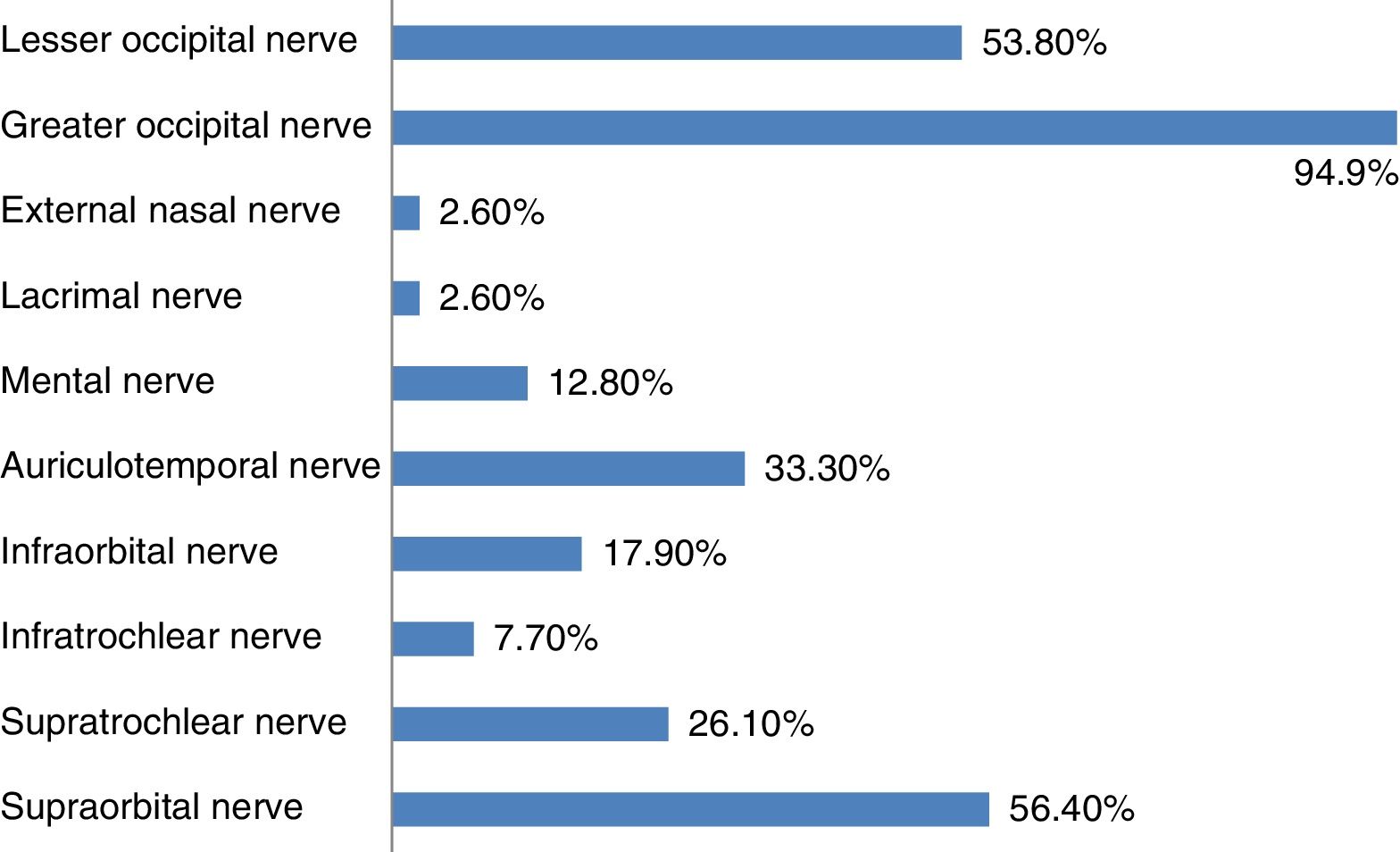
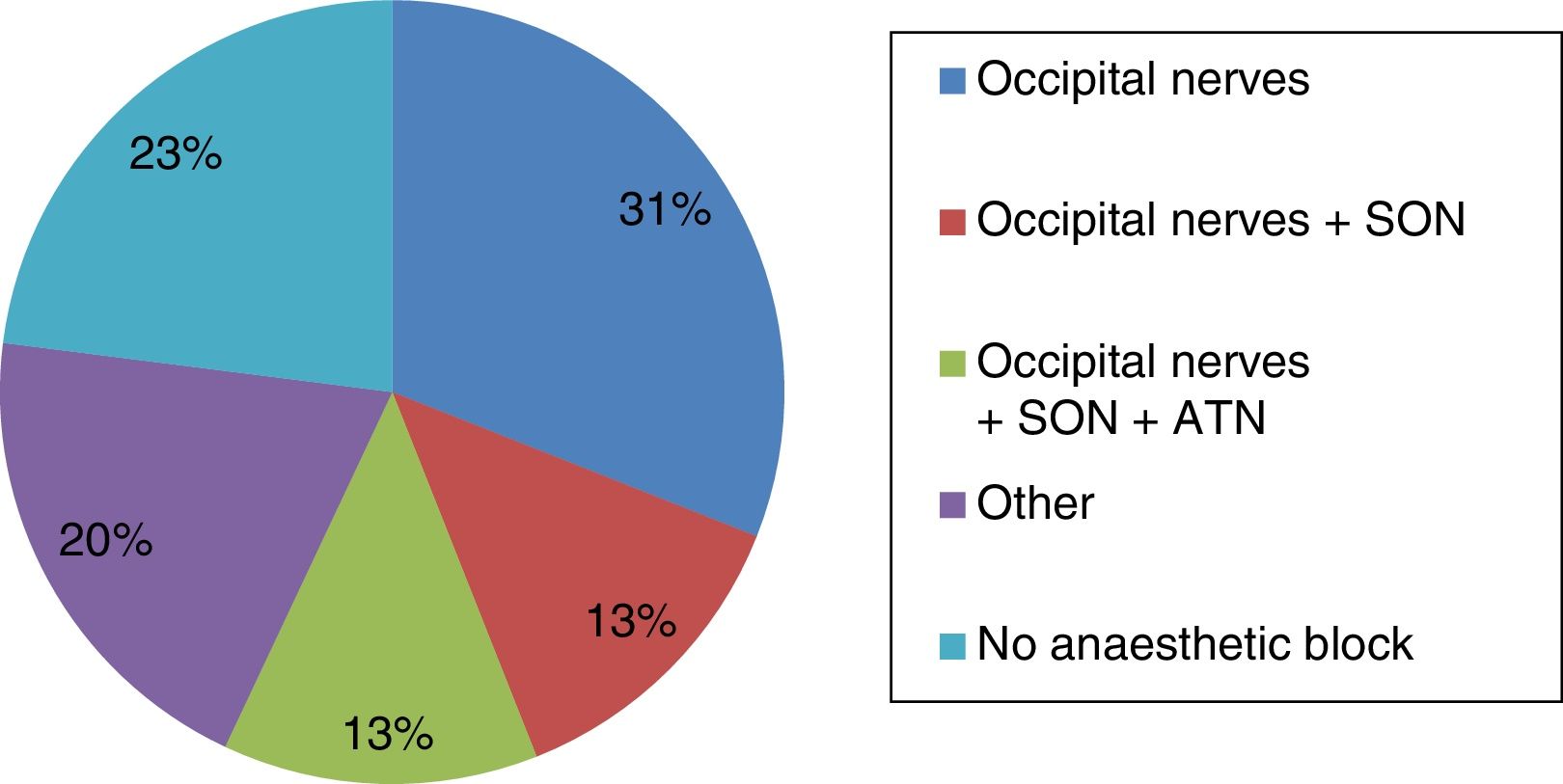
ResultsA total of 39 neurologists (mean age 41.74 years; SD: 9.73), 23 men (43.7 years; SD: 9.92) and 16 women (38.94 years; SD: 9.01) participated in this survey. Of these respondents, 76.9% used anaesthetic block in their clinical practice (79.16% in a tertiary-care hospital). The main indications were diagnosis and treatment of neuralgia (100%), prevention of chronic migraine (61.7%), episodic cluster headache (51.3%), and chronic cluster headache (66.7%). AB was used by 31% of the respondents to block only the lateral occipital complex, 13% also infiltrated the supraorbital nerve, and another 13% infiltrated the auriculotemporal nerve as well.
ConclusionsThe indications for anaesthetic blocks and the territories most frequently infiltrated are similar to those cited in the earlier survey. However, we observed increased participation in this latest survey and a higher percentage of young neurologists (35.89% aged 35 or younger), indicating that use of this technique has entered mainstream clinical practice.
Los bloqueos anestésicos constituyen un recurso terapéutico en muchos pacientes con cefalea, de forma aislada o en combinación con otros tratamientos. Sin embargo existe una importante heterogeneidad en los patrones de uso entre los distintos profesionales.
Material y métodoSe diseñó desde el Grupo de Estudio de Cefaleas de la Sociedad Española de Neurología (GECSEN) una encuesta transversal autoadministrada enviada a través de la plataforma del área científica de la SEN en febrero del 2016 a todos los miembros del grupo. El objetivo era conocer los principales aspectos técnicos y formales en relación con este procedimiento y compararlos con los datos obtenidos en una encuesta similar realizada en el año 2012.
ResultadosParticiparon 39 neurólogos (edad media: 41,74 años; DE: 9,73), 23 varones (43,7 años; DE: 9,92) y 16 mujeres (38,94 años; DE: 9,01). El 76,9% integraba los bloqueos anestésicos en su práctica clínica (el 79,16% en hospital de tercer nivel). Las principales indicaciones fueron: diagnóstico y tratamiento de las neuralgias (100%), prevención de migraña crónica (61,7%) y cefalea en racimos episódica (51,3%) y crónica (66,7%). El 31% de los encuestados bloquea solo el complejo occipital, el 13% infiltra además el nervio supraorbitario y otro 13% también el nervio auriculotemporal.
ConclusionesLas indicaciones del bloqueo anestésico así como los territorios infiltrados son similares en ambos años. Destacamos sin embargo una participación más activa en esta última encuesta y un porcentaje mayor de neurólogos jóvenes (el 35,89% tiene 35 años o menos) que indican una generalización de esta técnica en la práctica asistencial.
Anaesthetic block (AB) is increasingly used to treat headache both in Spain and abroad.1–13 This therapeutic resource may be used alone or in combination with other treatments. Although ABs are common practice in numerous specialised headache units, usage patterns vary greatly between professionals.
The results of a survey on the use of the technique conducted by the Spanish Society of Neurology's (SEN) Headache Study Group (GECSEN) were disclosed at the SEN's Annual Meeting in 2012.14 Four years after the publication of those findings, we analyse the current situation of ABs for headache and compare our results with those of previous years.
This survey is part of an ambitious project which aims to publish a consensus document that may serve as a guide for neurologists who wish to incorporate ABs into their management of patients with headache.
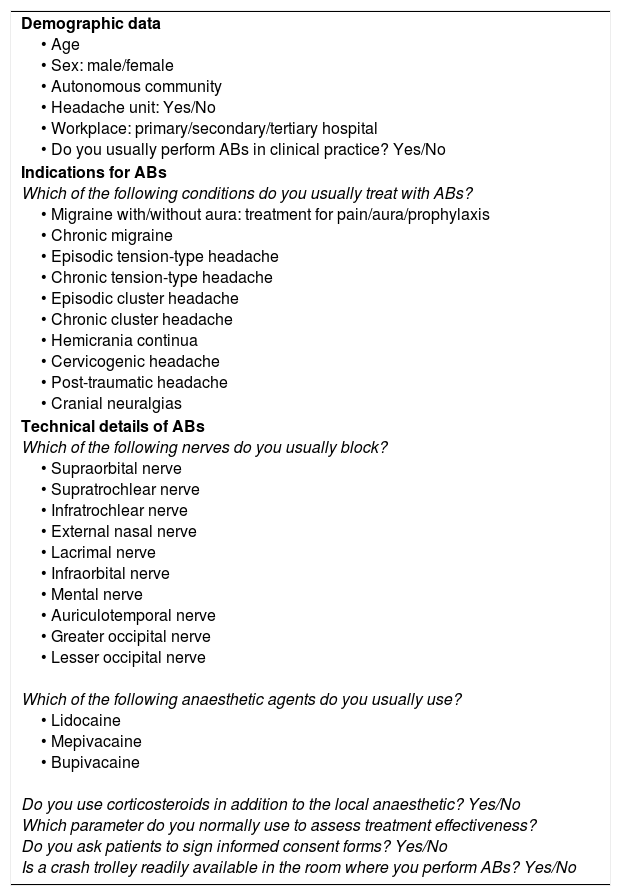
Material and methodsGECSEN's executive board designed a cross-sectional self-administered survey including open-ended and closed-ended questions (Table 1). As in the 2012 survey, the SEN's scientific division sent the survey to all GECSEN members by e-mail. Survey respondents remained anonymous at all times. We gathered data on the following variables:
- (a)
Responder data: sex, age, autonomous community, place of work (primary/secondary/tertiary hospital), whether they worked at a headache unit (yes/no), and whether they performed ABs in clinical practice (yes/no).
- (b)
Type of headache for which they administered AB: migraine (symptomatic treatment/prophylaxis), trigeminal autonomic cephalalgias (cluster headache, hemicrania continua), cervicogenic headache, tension-type headache, post-traumatic headache, occipital neuralgia, trigeminal neuralgia.
- (c)
Technical details: nerve receiving AB (occipital [lesser or greater occipital nerve], supraorbital, supratrochlear, infratrochlear, lacrimal, external nasal, infraorbital, auriculotemporal, mental), type of anaesthetic agent and whether it was combined with corticosteroids, whether patients signed an informed consent form, and availability of a cardiopulmonary resuscitation system.
Survey sent to the members of the Spanish Society of Neurology's Headache Study Group.
| Demographic data • Age • Sex: male/female • Autonomous community • Headache unit: Yes/No • Workplace: primary/secondary/tertiary hospital • Do you usually perform ABs in clinical practice? Yes/No |
| Indications for ABs Which of the following conditions do you usually treat with ABs? • Migraine with/without aura: treatment for pain/aura/prophylaxis • Chronic migraine • Episodic tension-type headache • Chronic tension-type headache • Episodic cluster headache • Chronic cluster headache • Hemicrania continua • Cervicogenic headache • Post-traumatic headache • Cranial neuralgias |
| Technical details of ABs Which of the following nerves do you usually block? • Supraorbital nerve • Supratrochlear nerve • Infratrochlear nerve • External nasal nerve • Lacrimal nerve • Infraorbital nerve • Mental nerve • Auriculotemporal nerve • Greater occipital nerve • Lesser occipital nerve Which of the following anaesthetic agents do you usually use? • Lidocaine • Mepivacaine • Bupivacaine Do you use corticosteroids in addition to the local anaesthetic? Yes/No Which parameter do you normally use to assess treatment effectiveness? Do you ask patients to sign informed consent forms? Yes/No Is a crash trolley readily available in the room where you perform ABs? Yes/No |
Qualitative variables are expressed as percentages and quantitative variables as means±SD.
ResultsThe survey was sent in February 2016 and completed by 39 neurologists (mean age: 41.74±9.73 years [range, 27-60]; 23 men [43.7±9.92] and 16 women [38.94±9.01]). Most respondents were from Madrid (30.8%), Catalonia (15.4%), and Andalusia (10.3%). Sixty-one percent of respondents worked at tertiary hospitals, 33.87% at secondary hospitals, and only 5.12% worked at primary hospitals. Broadly speaking, 71.8% of respondents worked in headache units, and 76.9% regularly performed ABs (79.16% in tertiary hospitals).
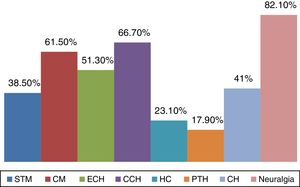
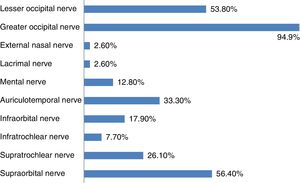
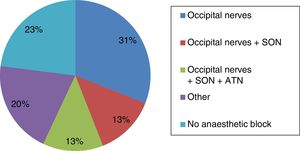
Treatment indications for AB included neuralgia (response to AB is a diagnostic criterion15), chronic migraine prevention (61.7%), episodic cluster headache (51.3%), and chronic cluster headache (66.7%). The main indications for AB are shown in Fig. 1. The nerves most frequently receiving ABs are the greater occipital nerve (94.9%), the supraorbitary nerve (56.4%), the lesser occipital nerve (53.8%), and the auriculotemporal nerve (33.3%) (Fig. 2). As shown in Fig. 3, 31% of respondents perform ABs to the occipital nerves only, 13% also administer them to the supraorbital nerve, and 13% to the auriculotemporal nerve in addition to the other 2 nerves. Improvements in the frequency and/or intensity of pain are the parameters most frequently used to assess treatment response.
Regarding the technical details, 54% of respondents frequently asked patients to sign informed consent forms before the procedure, and 30% had a crash trolley or a cardiopulmonary resuscitation system available. All respondents used amides (lidocaine, bupivacaine, mepivacaine) for AB; there was no significant difference between amide types. Corticosteroids were only used to treat cluster headache.
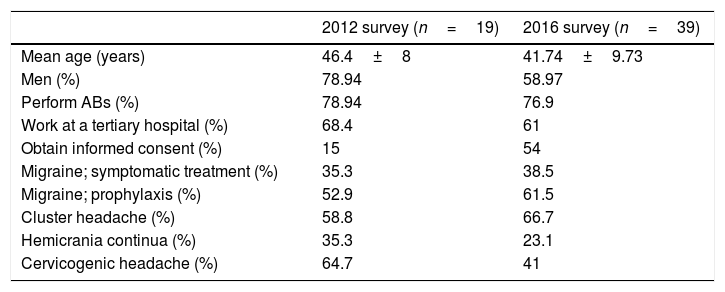
Table 2 shows a comparative analysis of the data obtained in the 2012 and 2016 surveys.
Comparative analysis of the data obtained in the 2012 and 2016 surveys.
| 2012 survey (n=19) | 2016 survey (n=39) | |
|---|---|---|
| Mean age (years) | 46.4±8 | 41.74±9.73 |
| Men (%) | 78.94 | 58.97 |
| Perform ABs (%) | 78.94 | 76.9 |
| Work at a tertiary hospital (%) | 68.4 | 61 |
| Obtain informed consent (%) | 15 | 54 |
| Migraine; symptomatic treatment (%) | 35.3 | 38.5 |
| Migraine; prophylaxis (%) | 52.9 | 61.5 |
| Cluster headache (%) | 58.8 | 66.7 |
| Hemicrania continua (%) | 35.3 | 23.1 |
| Cervicogenic headache (%) | 64.7 | 41 |
AB: anaesthetic block.
The results of the 2016 survey reveal that AB has become a frequently used therapeutic resource in clinical practice. Unlike in other, purely clinical neurology subspecialties, headache has a very active therapeutic component, combining conventional oral pharmacological treatment with more specialised techniques. Numerous studies conducted into AB over the past 10 years have enabled researchers to establish levels of evidence and grades of recommendation for different types of headache.16–18
The results of the 2012 survey, however, reveal highly variable usage patterns.14 Although the 2012 study included a smaller sample (n=19; age, 46.4±8 years; 78.94% men), 78.94% performed ABs, a similar rate to that obtained in the 2016 survey. The greater participation in the second survey shows the widespread use of this technique. Although these results cannot be generalised, they suggest that neurologists specialising in headache management in 2016 are younger (35.89% were aged under 36) and have incorporated AB into their clinical practice.
In 2012, ABs were indicated not only for patients with neuralgia of terminal branches of the trigeminal nerve, but also for migraine prophylaxis (52.9%), symptomatic treatment of migraine (35.3%), cluster headache (58.8%), hemicrania continua (35.3%), cervicogenic headache (64.75%), and tension-type headache (41.2%). Four years later, both the literature and our own clinical experience support similar indications for ABs, except for treating tension-type headache, as shown in the most recent version of the GECSEN's clinical practice guidelines for headache.16–18
AB was most frequently administered to the occipital nerves (≥95%) in both 2012 and 2016, followed by supraorbital nerve AB. The type of anaesthetic agent (amines in all cases) used also varied greatly in 2012. We should note, however, that only 3 neurologists (15.78%) obtained informed consent from patients in 2012, compared to 54% in the 2016 survey. Although AB is a safe technique, it may also cause adverse effects19–29; these are usually mild and reversible. Obtaining informed consent is therefore essential (a model informed consent form is available on the SEN's website30).
The comparative analysis of the results from the 2 cross-sectional surveys suggests that AB has entered mainstream clinical practice. Given the high variability in AB usage patterns, there is a need for prospective studies to be performed in order to gain a deeper knowledge of the technique and to gather more data on the indications, effectiveness, and response to AB for each nerve.
Our results should be interpreted with caution due to the study's sampling bias: the neurologists who completed the survey are very likely to perform ABs regularly to treat patients with headache or to have an interest in the procedure, and are therefore not representative of the population. Furthermore, as most of the questions in the survey were closed-ended, the results are more uniform but do not include other possible responses.
Although pericranial nerve block is common in other medical specialties, performing the technique correctly does not necessarily result in an adequate or uniform response. The medical histories of headache patients should include pain characteristics and location, associated symptoms, response to symptomatic/preventive treatment, and the presence of risk factors for progression to chronic headache. It is also essential to differentiate between neuralgia of intra- or epicranial origin, based on pain location and characteristics,31,32 and to systematically palpate the nerve territories and craniofacial structures where pain is located. Only in this way will we be able to provide our patients with individualised treatment and ensure an adequate response.
Conflicts of interestThe authors have no conflicts of interest to declare.
We would like to thank the SEN's scientific division for participating in the project.
Please cite this article as: Santos Lasaosa S, Gago Veiga A, Guerrero Peral ÁL, Viguera Romero J, Pozo-Rosich P. Patrones de bloqueo anestésico de nervios pericraneales en el paciente con cefalea. Neurología. 2018;33:160–164.