The COVID-19 pandemic has had a great impact on healthcare systems. Spain, where headache is the main reason for outpatient neurology consultation, is one of the countries with the most reported cases of the disease.
ObjectivesThis study aimed to analyse the impact of the COVID-19 pandemic on headache units in Spain and to evaluate how neurologists see the future of these units.
MethodsWe conducted a cross-sectional online survey of headache units during the sixth week of the state of alarm declared in Spain in response to the pandemic.
ResultsThe response rate was 74%, with the participation of centres with different characteristics and from all Autonomous Communities of Spain. Limitations in face-to-face activity were reported by 95.8% of centres, with preferential face-to-face consultation being maintained in 60.4%, and urgent procedures in 45.8%. In 91.7% of centres, the cancelled face-to-face activity was replaced by telephone consultation. 95.8% of respondents stated that they would use personal protection equipment in the future, and 86% intended to increase the use of telemedicine. The majority foresaw an increase in waiting lists (93.8% for initial consultations, 89.6% for follow-up, and 89.4% for procedures) and a worse clinical situation for patients, but only 15% believed that their healthcare structures would be negatively affected in the future.
ConclusionsAs a consequence of the pandemic, headache care and research activity has reduced considerably. This demonstrates the need for an increase in the availability of telemedicine in our centres in the near future.
La infección por SARS-CoV-2 ha tenido un enorme impacto en los sistemas sanitarios. España, donde la cefalea constituye el motivo principal de consulta ambulatoria en Neurología, es uno de los países con más casos notificados.
ObjetivoConocer el impacto de la pandemia COVID-19 en las Unidades de Cefaleas en España y evaluar cómo imaginan el futuro de estas estructuras los neurólogos responsables.
MétodosEstudio transversal mediante encuesta online distribuida a los responsables de las Unidades, realizada durante la sexta semana del Estado de Alarma.
ResultadosLa tasa de respuesta fue del 74%, con participación de centros de diferentes características y de todas las Comunidades Autónomas. El 95,8% describió limitaciones en la actividad presencial, un 60,4% mantuvo la consulta presencial preferente y el 45,8% los procedimientos urgentes. En el 91,7% de los centros la actividad presencial cancelada se sustituyó por consulta telefónica. El 95,8% de los encuestados afirmó que empleará material de protección personal en el futuro y el 86% pretende incorporar en mayor medida la telemedicina. La mayoría prevé un incremento en las listas de espera (93,8% en primeras visitas, 89,6% en revisiones y 89,4% en procedimientos) y una peor situación clínica de los pacientes, pero sólo un 15% cree que su estructura asistencial se verá debilitada.
ConclusionesComo consecuencia de la pandemia, la actividad asistencial e investigadora en cefaleas se ha reducido de manera notable. Esto pone de manifiesto la necesidad de un incremento de la oferta de telemedicina en nuestros centros en un futuro cercano.
The coronavirus disease 2019 (COVID-19) pandemic has unexpectedly changed healthcare provision in a matter of weeks. This new situation has had an unprecedented impact on healthcare systems worldwide and has affected all hospital departments, including neurology departments.1,2 As most healthcare resources have been reallocated to the management of patients with SARS-CoV-2 (a phenomenon that oncologists have referred to as the “distraction effect”3), the care provided to patients with other diseases, including neurological diseases, has inevitably decreased. Reallocation of human and material resources has led to a change in routine healthcare activities. Furthermore, patient visits to healthcare centres have decreased considerably; now, most in-person consultations have been cancelled or replaced by teleconsultations.2,4
A considerable percentage of patients attended at neurology departments have chronic diseases; in-person consultations with these patients are only held when strictly necessary to prevent the spread of the virus.5 This change in the healthcare model has had a considerable impact on such chronic neurological conditions as headache.6,7 Tension-type headache and migraine are the second and third most prevalent diseases worldwide.8 In Spain, headache is the most frequent reason for consultation with the neurology department.9 Furthermore, migraine is the second most frequent cause of years lived with disability worldwide.8 In the past decade, new treatments and invasive procedures have been developed, resulting in greater specialisation among neurologists and the creation of specialised units for comprehensive care of these patients.10–12
Telemedicine has become an essential tool for neurological care in the current situation.13 However, few studies have analysed its usefulness for the management of such conditions as headache. Recent studies support the use of telemedicine due to its low cost, effectiveness, and patient acceptance.14 However, the need for appropriate technology, the restrictions for patient confidentiality, and the increased use of interventional techniques may represent limitations for the generalised use of telemedicine for headache management.7
The first case of SARS-CoV-2 infection in Spain was reported on 31 January 2020; by the end of our study’s data collection period, 209 465 confirmed COVID-19 cases and 23 521 deaths due to SARS-CoV-2 infection had been recorded.15 This led to the declaration of a state of alarm,16 which brought about a radical change in health and social care whose consequences are still to be determined.
The purpose of this study was to evaluate the impact of the COVID-19 pandemic on headache units and clinics in Spain and how neurologists see the future of these centres.
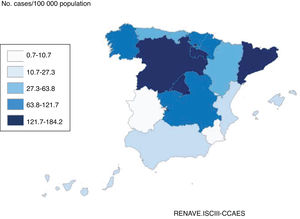
Material and methodsDesignWe conducted a cross-sectional observational study using an ad-hoc questionnaire including both open-ended and closed-ended questions (dichotomous and multiple-choice). The questionnaire was distributed to heads of headache units and specialist headache clinics from all Spanish autonomous communities. The participants were selected using the map of Spanish headache units and specialist clinics, a document including all healthcare facilities dedicating at least one day per week to patients with headache,17 published in November 2019 by the Spanish Society of Neurology’s Headache Study Group (GECSEN, for its Spanish initials). The questionnaire was sent by e-mail and could be completed using any electronic device within a period of 7 days, coinciding with the sixth week of the state of alarm in Spain.16Fig. 1 shows the number of infected individuals per 100 000 population in each autonomous community at the time the survey was closed.
The project was approved by the board of the GECSEN and the drug research ethics committee of the Valladolid Este health district (project no. PI 20-1759). The participating neurologists remained anonymous at all times.
The survey included 53 questions, grouped into 4 sections (Appendix A, available online):
Section 1. Characteristics of the headache unit/clinic and prior experience with telemedicine.
Section 2. Impact of the COVID-19 pandemic on healthcare and research activity: limitations on in-person consultations and use of teleconsultations.
Section 3. Adaptation of patients with headache to the new healthcare model and clinical status after the pandemic.
Section 4. Future impact of the pandemic on headache units/clinics and use of telemedicine after the pandemic.
Statistical analysisThe SPSS software (version 23.0) was used for all statistical analyses. Categorical variables are expressed as percentages, and quantitative variables as mean (standard deviation [SD]).
ResultsThe survey was sent to 65 neurologists; the response rate was 74%. Data were collected from centres in all autonomous communities. Fig. 2 shows the number of participating centres in each autonomous community.
Characteristics of the participating healthcare centresTable 1 presents the main results from section 1 of the survey. The healthcare centres included in the study provide care to heterogeneous reference areas, with a mean (SD) population of 341 434 (147 310). The mean time dedicated to headache consultations was 2.6 (1.5) days per week, with 417 (310) patients treated annually in first consultations and 1264 (1035) in follow-up consultations. The mean number of neurologists per unit dedicating at least one day per week to headache consultations was 1.9 (1.4). Before the pandemic, the mean waiting time was 10.3 (10.3) weeks for first consultations, 16.1 (11.9) for follow-up consultations, and 10.3 (9.5) for specific procedures.
Characteristics of the participating healthcare centres.
| % | |
|---|---|
| Type of facility | |
| Headache unit | 66.7 |
| Specialist headache clinic | 33.3 |
| Reference centre | |
| Yes | 70.8 |
| No | 29.2 |
| Performs procedures | |
| Yes | 85.4 |
| No | 14.6 |
| Nurse consultations | |
| Yes | 77.1 |
| No | 22.9 |
| No. neurologists specialising in headache | |
| < 2 | 37.5 |
| ≥ 2 | 62.5 |
| Exclusively dedicated to headache | 12.5 |
| Partially dedicated to headache | 87.5 |
| Fellowship programme | |
| Yes | 14.6 |
| No | 85.4 |
| Exclusively dedicated to headache | 61.5 |
| Partially dedicated to headache | 38.5 |
| Multicentre clinical trials | |
| Yes | 56.3 |
| No | 43.8 |
Limitations on in-person healthcare provision due to the pandemic were reported in 95.8% of participating units: 60.4% only held in-person consultations for critical or priority patients, and 45.8% only for emergency procedures. Table 2 shows data on in-person consultations (scheduled consultations and priority patients) during the pandemic, by autonomous community, and the cumulative incidence of COVID-19 during the 14 days prior to the end of the survey period.
In-person healthcare provision during the COVID-19 pandemic, by autonomous community.
| Autonomous community(no. participating centres) | No. cases/100 000 population | Consultations cancelled(%) | Priority consultations (%) | Scheduled consultations (%) | Emergency procedures (%) | Scheduled procedures (%) |
|---|---|---|---|---|---|---|
| Castile-Leon (3) | 182.78 | 93.3 | 66.7 | 33.3 | 66.7 | 0.0 |
| Region of Madrid (8) | 176.13 | 90.0 | 37.5 | 0.0 | 37.5 | 12.5 |
| Catalonia (10) | 168.87 | 88.4 | 60.0 | 0.0 | 100.0 | 0.0 |
| Castile-La Mancha (1) | 167.94 | 100.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| La Rioja (1) | 119.63 | 100.0 | 100.0 | 0.0 | 100.0 | 0.0 |
| Navarre (3) | 93.09 | 65.0 | 33.3 | 66.7 | 33.3 | 66.7 |
| Cantabria (1) | 72.08 | 75.0 | 100.0 | 0.0 | 0.0 | 100.0 |
| Galicia (1) | 64.12 | 90.0 | 10.0 | 0.0 | 100.0 | 0.0 |
| Basque Country (2) | 60.60 | 80.0 | 100.0 | 0.0 | 50.0 | 0.0 |
| Aragon (4) | 57.53 | 37.5 | 50.0 | 25.0 | 25.0 | 50.0 |
| Extremadura (1) | 34.37 | 80.0 | 100.0 | 0.0 | 100.0 | 0.0 |
| Asturias (1) | 28.65 | 90.0 | 100.0 | 0.0 | 0.0 | 0.0 |
| Balearic Islands (2) | 26.01 | 29.0 | 50.0 | 0.0 | 50.0 | 0.0 |
| Region of Valencia (3) | 24.46 | 70.0 | 100.0 | 0.0 | 100.0 | 0.0 |
| Andalusia (4) | 20.32 | 42.5 | 75.0 | 25.0 | 50.0 | 50.0 |
| Region of Murcia (1) | 10.91 | 50.0 | 50.0 | 0.0 | 0.0 | 100.0 |
| Canary Islands (2) | 10.63 | 42.5 | 100.0 | 0.0 | 50.0 | 50.0 |
In 77.1% of centres, in-person consultations were cancelled mainly due to the lockdown measures. In 37.5% of units, staff were reallocated to other areas of neurology, and in 47.9% of cases they were transferred to COVID-19 care teams. SARS-CoV-2 infection (27.1%) or quarantine (29.2%) of healthcare professionals working at headache units limited healthcare provision. Changes to be made to the healthcare model during the pandemic were established by hospital directors in 64.6% of units, the head of the department in 47.9%, and the autonomous community’s regional health ministry in 18.8%. In 45.8% of units, healthcare professionals were able to manage their own consultations at least partially.
In 33.3% of units, treatment with calcitonin gene–related peptide (CGRP) monoclonal antibodies (mAb) was started during the pandemic; patient education on the use of the drug was provided in person in 68.7% of units and in teleconsultations in the remaining units. In only 6.3% of centres where treatment had been started before the pandemic did the patient travel to the hospital for follow-up; in the remaining cases, follow-up consultations were held by telephone. In 47.9% of centres, patients travelled to hospital to collect the drug; only 13 units established a home delivery system.
Research activity decreased or was postponed in most units: 97.9% cancelled all consultations for patient inclusion in clinical trials, and only 20.8% continued holding follow-up consultations, 60% of which were teleconsultations.
Sixty-four percent of participants reported that patients had reacted favourably to the changes in healthcare provision during the pandemic; 45.8% reported clinical worsening of the patients evaluated during the pandemic, and 41.7% reported clinical stability.
Use of telemedicine before and during the COVID-19 pandemicTelemedicine was used before the pandemic at 89.6% of units; telephone (64.6%) and e-mail (54.2%) were the most widely used methods. Such other methods as hospital platforms (16.7%) and web pages (8.3%) were less frequently used.
During the pandemic, 91.7% of units attended patients by telephone. While 35.4% of units continued to use the telemedicine systems that were employed prior to the pandemic, 52.1% also incorporated new systems. The number of teleconsultations with primary care and emergency departments remained stable in 41.7% of centres and increased in 14.6%. However, 39.6% of units reported that no systems for communication with other departments were implemented during the pandemic. Regarding other forms of communication, 31.3% of the neurologists surveyed shared the GECSEN recommendations for patients with headache on social media, and 10.4% used social media to communicate the changes in healthcare provision implemented in their units.
Expected short-term impact of the COVID-19 pandemicLastly, we evaluated respondents’ opinions on the future impact of the pandemic on headache units and specialised consultations. A total of 41.7% of participants expected their units to function normally without additional staff. However, 31.3% and 6.3% believed that their units would require additional physicians and nurses, respectively, and 20.8% responded that they would need both. Table 3 shows participants’ opinions regarding the short-term impact of the pandemic on healthcare provision at their units.
Future impact of the COVID-19 pandemic.
| 1) In your opinion, will waiting times for first consultations increase? | |
|---|---|
| No | 6.3 |
| Yes, slightly | 41.7 |
| Yes, considerably | 52.1 |
| 2) In your opinion, will waiting times for follow-up consultations increase? | |
| No | 10.4 |
| Yes, slightly | 27.1 |
| Yes, considerably | 62.5 |
| 3) In your opinion, will waiting times for procedures increase? | |
| No | 10.4 |
| Yes, slightly | 35.4 |
| Yes, considerably | 54.2 |
| 4) In your opinion, will waiting times for treatment with CGRP mAb increase? | |
| No | 12.5 |
| Yes, slightly | 47.9 |
| Yes, considerably | 35.4 |
| 5) In your opinion, will restrictions on starting treatment with CGRP mAb change? | |
| No | 64.6 |
| Yes, there will be more restrictions | 31.3 |
| Yes, there will be fewer restrictions | 4.2 |
| 6) Will you increase the number of nurse consultations? | |
| Yes | 35.4 |
| I would like to | 50.0 |
| No | 14.6 |
| 7) Will you increase teleconsultations with primary care physicians or the emergency department? | |
| Yes | 12.5 |
| I would like to | 64.6 |
| No | 20.8 |
| 8) After the pandemic, do you expect your headache unit to: | |
| Have more resources | 25.0 |
| Remain the same | 60.4 |
| Have fewer resources | 14.6 |
| 9) After the pandemic, do you expect patients to request: | |
| In-person consultations | 29.2 |
| More teleconsultations | 45.8 |
| Both | 25.0 |
CGRP mAB: monoclonal antibodies against the calcitonin gene–related peptide; COVID-19: coronavirus disease 2019.
Spain is one of the European countries with the most confirmed cases of SARS-CoV-2 infection,18 which has posed a challenge in maintaining scheduled consultations in most hospitals. In-person outpatient consultations have either been cancelled or replaced by teleconsultations. This change in healthcare provision has had a considerable impact on headache units and consultations in Spain, where 96% of neurologists have experienced limitations to routine clinical practice and 75% have had to cancel in-person consultations. Restrictions on in-person consultations have also affected patients with such other neurological diseases as multiple sclerosis,19 epilepsy,20 and neuromuscular disorders.21
Ours is the first European study to evaluate headache management during the COVID-19 pandemic; the participation of neurologists from all autonomous communities enables an overall view of the situation. The pandemic has not affected all autonomous communities equally; those with greater cumulative SARS-CoV-2 incidence in the last 14 days (data from the Spanish Ministry of Health15) cancelled over 80% of in-person consultations, as shown in Table 2. Our study includes information from different types of headache management services, ranging from large multidisciplinary units with several neurologists specialising in headache and intense research activity to specialist headache clinics in hospitals serving smaller populations. Despite these differences, all centres experienced changes in healthcare provision during the pandemic.
In recent years, interventional techniques have become an essential tool for the management of migraine. Due to the pandemic, fewer than 20% of the participating units or clinics were able to perform these procedures (anaesthetic block of pericranial nerves, botulinum toxin) as normal, with most procedures being delayed or cancelled.
These procedures involve close contact with the patient, which increased the risk of infection. Therefore, use of other preventive treatments has been encouraged with a view to decreasing the risk of infection7; healthcare professionals should use personal protective equipment during these procedures if the patient presents symptoms of COVID-19.
The rapid spread of the virus has caused worry among healthcare professionals, who are at greater risk of infection during their work.22 According to data from the Health Alert and Emergency Coordination Centre of the Spanish Ministry of Health, over 25 000 healthcare professionals have been infected with SARS-CoV-2 in Spain.23 The neurologists managing headache units or clinics in Spain are concerned about the safety of healthcare professionals, and most expected that they would need to use personal protective equipment in the future, especially when close contact with the patient is needed.
Although treatment with CGRP mAb may be self-administered at home, these drugs are dispensed at hospitals; this hindered treatment during the state of alarm due to restrictions on the free movement of citizens. A recent Italian study reports that patients visited hospitals to collect medications despite such restrictions.6 In our study, patients collected their medications at hospital in 57.5% of units, with 13 healthcare centres offering home delivery. Our results underscore the importance of promoting new strategies for the distribution and administration of hospital medications.
Special emphasis should be placed on telemedicine, which became the main channel for healthcare provision in a matter of weeks. In our study, 90% of the participating headache management facilities used telemedicine (mainly telephone consultations) before the pandemic, and 92% replaced in-person visits with teleconsultations during the pandemic. Such tools as e-mail and hospital platforms were less frequently used, despite evidence of the usefulness of e-mail for communication between primary care and headache specialists.24
Increased use of telemedicine seems to have been well received by patients with headache; most of these patients understand the risk of exposure to SARS-CoV-2 and are willing to reduce hospital visits. The pandemic has reaffirmed the usefulness of telemedicine in patients with headache, but also demonstrates the need to further expand its use for communication with patients and other healthcare professionals. New strategies should be developed to improve management of patients with headache, particularly those visiting the hospital on a regular basis for certain procedures or parenteral treatments.7,25
Most neurologists managing headache units in Spain intend to implement or expand the use of telemedicine for routine management of their patients. Headache units have rapidly adapted to telemedicine, promoting teleconsultations to maintain contact with their patients.25 This seems to be consistent with the opinions of neurology department heads, who believe that the use of telemedicine will increase for the management of all neurological diseases.26
The last section of our survey addressed future perspectives. In the short and medium term, most survey respondents foresee a significant increase in waiting times for first consultations, follow-up consultations, and therapeutic procedures. Given the high prevalence of headache and the potential clinical worsening of these patients, it will be essential to ensure access to care for patients with poorer clinical status or those with no history of headache who present warning signs. Headache is one of the most frequent neurological symptoms of COVID-19, occasionally appearing as the only symptom of the disease.27
We should highlight the high rate of neurologists completing the survey in such a short time, during the sixth week of the state of alarm; this may be due to awareness among healthcare professionals of the magnitude of the problem.
The main limitation of our study is the possibility of a selection bias: although the participation rate was high, not all headache units and consultations are represented. The large disparities between the centres included in our study is both a strength, as it provides a comprehensive perspective of the problem, and a limitation, since the impact of the pandemic and the need to reallocate healthcare professionals varied greatly between centres. Our survey included closed-ended questions, which provide uniform results but do not allow for other response options. Finally, we asked the participants to make predictions about the future, but only in the medium-to-long term will we be able to determine their accuracy.
ConclusionsDuring the COVID-19 pandemic, 95% of the headache units participating in our study limited in-person consultations; 60% and 45% of units only held in-person consultations for critical patients and for emergency procedures, respectively. Only 33% of units started treatment with CGRP mAb during the pandemic. Initial consultations for inclusion of patients in research studies were either cancelled or reduced in 97% of units, with follow-up visits being held in only 21% of centres. Telemedicine was used in 91% of units, and 41% used teleconsultations to communicate with primary care physicians or emergency departments. Over 50% of the participating neurologists expected that their units would need more healthcare staff as a result of the pandemic.
Our study provides “real-time” data about the impact of the pandemic on centres offering specialised headache management in Spain and paves the way for further research after lockdown into the true impact of the pandemic and changes in the outlook in the coming months.
Conflicts of interestThe authors have no conflicts of interest to declare.
We wish to thank all the neurologists participating in our survey.
Please cite this article as: López-Bravo A, García-Azorín D, Belvís R, González-Oria C, Latorre G, Santos-Lasaosa S, et al. Impacto de la pandemia COVID-19 en la atención al paciente con cefalea en España: análisis de situación con una mirada al futuro. Neurología. 2020;35:372–380.