Primary care (PC) and general neurology clinics (NC) assume the leading role in the health care of patients with dementia. There are hardly any studies on the satisfaction of the caregiver at these settings of health care.
MethodsA questionnaire was designed and distributed to 75 caregivers of patients with dementia who were reviewed in an NC and who had been referred from PC. The questionnaire included questions associated with the care, the use of services, and satisfaction. Sociodemographic and clinical variables were also collected. The results of the questionnaire are described and a simple correlation analysis (Spearman r) was performed to determine the factors associated with satisfaction.
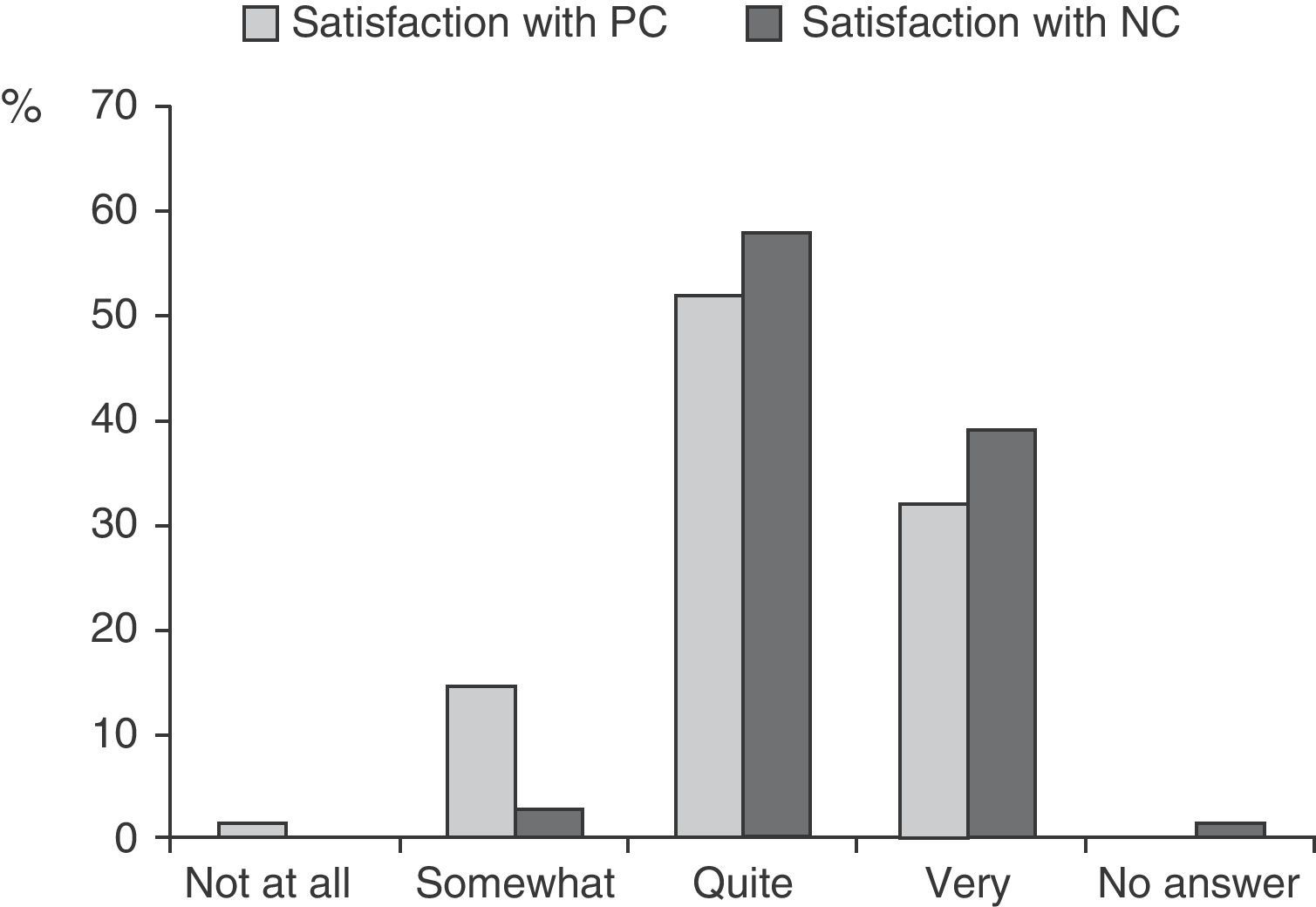
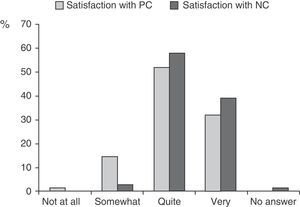
ResultsThe majority of carers were sons or daughters (60%) or spouses (31%), of which 73% were women. The service most used was home help (36%), but 41% of patients had no services available. Satisfaction was high (84% quite or very satisfied with PC, 97% quite or very satisfied with the NC, P<.01). A greater number of years giving care was associated with a lower satisfaction with PC ((r=−0.37, P<.005), while institutionalisation was associated with a lower satisfaction with the NC (r=−0.30, P<.01).
ConclusionsIn a context of a scarcity of resources, the satisfaction of the caregivers of patients with dementia, as regards health care, was high, possibly due to the motivation of the health professionals and the positive attitude of the caregivers themselves.
La atención primaria (AP) y las consultas de neurología general (CN) asumen la principal carga en la asistencia sanitaria de los pacientes con demencia. Apenas se dispone de estudios acerca de la satisfacción del cuidador con estos ámbitos asistenciales.
MétodosSe diseñó y administró una encuesta a 75 cuidadores de pacientes con demencia que acudieron a revisión a una CN y que habían sido remitidos desde la AP. La encuesta incluía cuestiones relacionadas con los cuidados, la utilización de servicios y la satisfacción. Se recogieron, además, variables sociodemográficas y clínicas, se describieron los resultados de la encuesta y se realizó un análisis de correlaciones simples (r de Spearman) para explorar los factores asociados a la satisfacción.
ResultadosLos cuidadores fueron mayoritariamente hijas/os (60%) o cónyuges (31%). El 73% eran mujeres. El servicio más utilizado fue la ayuda en el domicilio (36%), pero el 41% de los pacientes no disponía de ningún servicio. La satisfacción fue alta (84% bastante o muy satisfechos con la AP, 97% bastante o muy satisfechos con la CN, p<0,01). Un mayor número de años cuidando se asoció a una menor satisfacción con la AP (r=−0,37, p<0,005), mientras que la institucionalización se asoció a una menor satisfacción con la CN (r=–0,30, p<0,01).
ConclusionesEn un contexto de escasez de recursos, la satisfacción de los cuidadores de pacientes con demencia respecto de la asistencia sanitaria fue alta, posiblemente debido a la motivación de los profesionales y a la actitud positiva de los cuidadores.
Social and health care advances have brought about not only increased life expectancy, but also increases in processes associated with ageing, including forms of dementia.1 In cases in which there is no curative treatment, these chronic and usually degenerative processes require an integrated care model. In such models, quality of life is the key factor, for both the patient and the caregiver.2 With this in mind, achieving equitable, universal and sustainable service coverage would appear to be a top social priority.3
In Spain, 70%–80% of the population with dementia remains at home, and most people are assisted by family members or close acquaintances who are not paid for providing this service.4,5 As dementia progresses, these informal caregivers become more and more relevant. In most cases, they come to be the key players who guarantee provision, continuity and coordination of all other health and social services.
The main burden of medical assistance for dementia rests on primary care professionals (PCPs).6 These professionals are generally supported by neurology, geriatric care and psychiatric departments. In generalist or specialist clinics, they work together to confirm the diagnosis, begin specific pharmacological treatment and consult on complex or unusual problems.7–9
User satisfaction is one of the main quality indices for healthcare and related services.10 Surprisingly, a very few studies have been dedicated to understand and analyse the needs and level of satisfaction of informal caregivers of dementia patients (DP) with respect to the medical care those patients receive. The few published studies are qualitative11 or describe very specific aspects of specialist care.9,12 There are no studies describing level of satisfaction with the 2 main levels of care, and potential causes of dissatisfaction have not been analysed either. A study of these aspects would help us orient available resources and develop new lines of service.
The present study contemplates 4 objectives: (a) describe characteristics of DPs and their caregivers in a general neurology clinic; (b) ascertain caregivers’ level of satisfaction with the care received by patients; (c) analyse possible causes or factors determining satisfaction, and (d) propose means of introducing improvements.
Subjects and methodsWe invited all caregivers who attended a general neurology outpatient clinic (NC) between July and December 2008 to participate. Patients and caregivers met the following inclusion criteria:
Patient previously diagnosed with dementia (as per DSM-IV-TR criteria)13 attending an appointment at the NC in the company of an unpaid caregiver.
The patient had been referred to the NC by a PCP due to an unconfirmed suspicion of cognitive decline.
The caregiver self-identified as the primary caregiver.
The caregiver gave verbal consent for participating in the study.
The research team (a resident doctor/general practitioner, a nurse and a neurologist) drew up a survey to ascertain the needs and level of satisfaction of non-professional DP caregivers. They formulated questions which, to the team's best knowledge, might be related to the caregiver's sensation of burden and satisfaction with the patient's healthcare. They specifically investigated the time dedicated to care, prior relationship with the patient, motivation for providing care, informal assistance, services used and how those services were financed. Two questions regarding satisfaction with care on both the PC and NC levels were also included. The survey also contained 3 free response questions on aspects of PC that might be improved, aspects of the NC that might be improved, and any other suggestions or observations the caregiver wished to make. The survey ended with a list of questions regarding what a caregiver might require and expect from a hypothetical support programme. The results from these two parts of the survey (areas needing improvement and a support programme for caregivers) are not described in this article.
The neurologist invited caregivers to participate in the study at the end of the scheduled visit. The survey was conducted by the resident or by the nurse in another room. We intended for caregivers to fill in the survey alone, but offered assistance if they had difficulties reading or understanding it, sensory deficit or questions left unanswered.
We also recorded the following variables which were potentially related to caregiver satisfaction and needs:
Mini-mental state examination (MMSE).14 This test evaluates the patient's cognitive capacities. Scores range from 0 (worst state) to 30 (best state).
Functional assessment staging test (FAST).15 This test measures independence in activities of daily living (ADLs) in 16 stages from 1 (the best) to stage 7f (the worst).
Affective or behavioural disorder. This was measured using an ordinal scale with 4 levels designed ad hoc. Its score ranged from 0 (no problems) to 3 (severe disorders).
Global deterioration scale (GDS).16 This scale measures stages of dementia. Stages on the scale progress from 1 (no cognitive decline) to 7 (severe dementia).
Zarit caregiver burden interview (CBI).17 This 22-question self-completed survey measures the perceived burden of providing care. Scores on the scale range from 0 (no burden) to 88 (highest level of burden).
Clinical variables were recorded by the neurologist on the day the survey was completed. For cognitive variables (MMS), functional variables (FAST) and global variables (GDS), we also recorded values at the time of the first visit to the NC (data available in the medical history). We recorded data on 2 different occasions in order to investigate a potential association between the patient's rate of deterioration and caregiver satisfaction. Caregivers filled in the CBI after the survey, with the help of the resident or the nurse.
Descriptive statistics were used to present characteristics of patients and caregivers, survey results, and the values from the scales that were used. Possible determining factors for satisfaction were investigated using a simple correlation analysis (Spearman's rho).18 This analysis was completed twice in order to evaluate satisfaction with PC separately from satisfaction with NC.
ResultsWe identified 83 patient–caregiver pairs; 75 were included in the study (6 caregivers could not complete the study due to time constraints and another 2 caregivers declined to participate). Patients included belonged to 16 different PC centres in Health District 1 in the city of Madrid. Of the patients, 7 (9.3%) resided in institutions.
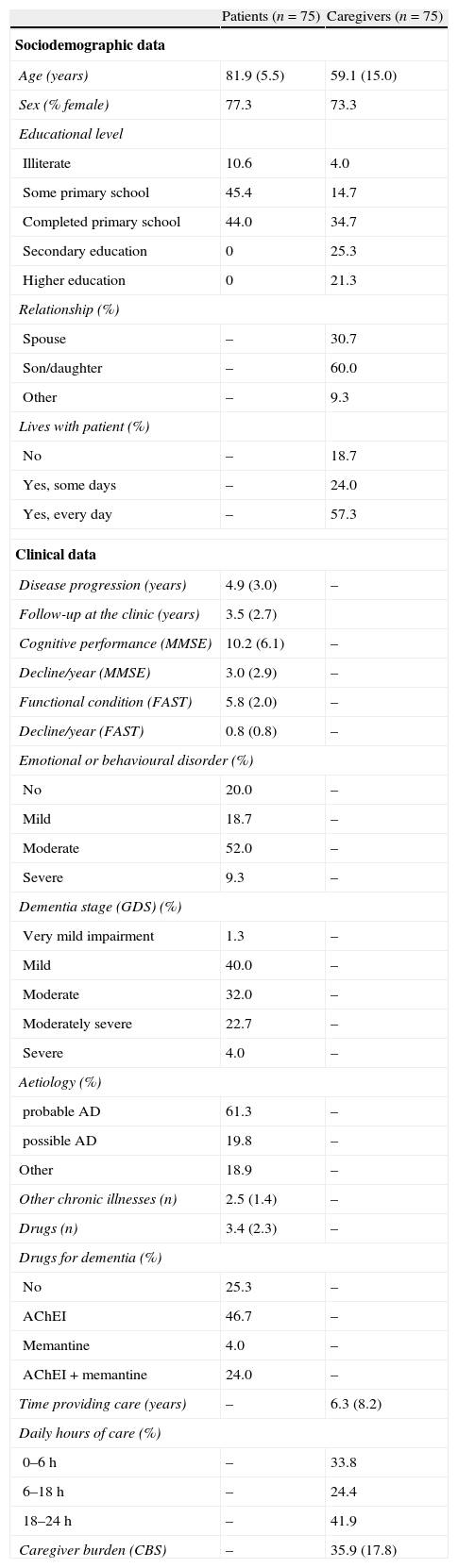
Patient and caregiver characteristics at the time of the survey and changes in clinical data between the first visit to the NC and the time of the survey are shown in Table 1. Mean patient age was 81.9 years (range, 65–96) and 77.3% were female. The mean elapsed duration of disease was 4.9 years (range, 3.6–13.6) with a mean annual decrease of 3 points on the MMSE. Most patients (58.7%) suffered from moderate or severe dementia, and its most common cause was Alzheimer disease (AD) (81.1%). Of the patient total, 74.7% were treated with a drug specific to dementia (acetylcholinesterase inhibitors, memantine or both).
Patient and caregiver characteristics.
| Patients (n=75) | Caregivers (n=75) | |
| Sociodemographic data | ||
| Age (years) | 81.9 (5.5) | 59.1 (15.0) |
| Sex (% female) | 77.3 | 73.3 |
| Educational level | ||
| Illiterate | 10.6 | 4.0 |
| Some primary school | 45.4 | 14.7 |
| Completed primary school | 44.0 | 34.7 |
| Secondary education | 0 | 25.3 |
| Higher education | 0 | 21.3 |
| Relationship (%) | ||
| Spouse | – | 30.7 |
| Son/daughter | – | 60.0 |
| Other | – | 9.3 |
| Lives with patient (%) | ||
| No | – | 18.7 |
| Yes, some days | – | 24.0 |
| Yes, every day | – | 57.3 |
| Clinical data | ||
| Disease progression (years) | 4.9 (3.0) | – |
| Follow-up at the clinic (years) | 3.5 (2.7) | |
| Cognitive performance (MMSE) | 10.2 (6.1) | – |
| Decline/year (MMSE) | 3.0 (2.9) | – |
| Functional condition (FAST) | 5.8 (2.0) | – |
| Decline/year (FAST) | 0.8 (0.8) | – |
| Emotional or behavioural disorder (%) | ||
| No | 20.0 | – |
| Mild | 18.7 | – |
| Moderate | 52.0 | – |
| Severe | 9.3 | – |
| Dementia stage (GDS) (%) | ||
| Very mild impairment | 1.3 | – |
| Mild | 40.0 | – |
| Moderate | 32.0 | – |
| Moderately severe | 22.7 | – |
| Severe | 4.0 | – |
| Aetiology (%) | ||
| probable AD | 61.3 | – |
| possible AD | 19.8 | – |
| Other | 18.9 | – |
| Other chronic illnesses (n) | 2.5 (1.4) | – |
| Drugs (n) | 3.4 (2.3) | – |
| Drugs for dementia (%) | ||
| No | 25.3 | – |
| AChEI | 46.7 | – |
| Memantine | 4.0 | – |
| AChEI + memantine | 24.0 | – |
| Time providing care (years) | – | 6.3 (8.2) |
| Daily hours of care (%) | ||
| 0–6h | – | 33.8 |
| 6–18h | – | 24.4 |
| 18–24h | – | 41.9 |
| Caregiver burden (CBS) | – | 35.9 (17.8) |
AD: Alzheimer disease; CBI: caregiver burden interview17; FAST: stage according to functional assessment screening tool15; GDS: global deterioration scale score16; AChEI: acetylcholinesterase inhibitor; MMSE: mini-mental state examination score14; –: not applicable.
Values are expressed as mean (SD) except where (%) is indicated.
Most of the caregivers were either sons/daughters or spouses of the patient (90.7%), and most were female (73.3%). Caregivers’ educational levels were clearly higher than those of patients (44.6% of caregivers, and none of the patients, had completed secondary or university studies). The patient and the caregiver lived together (continuously or at least 1 day per week) in most cases (81.3%). Caregivers had been caring for the patient an average of 6.3 years (range, 0–50 years). We observed a biphasic distribution in the number of daily hours of care, especially among those caregivers providing the most hours of care (41.9% stated that their mean number of hours employed providing care or direct supervision ranged between 18 and 24hours daily). On average, caregivers perceived their burden as moderate (mean score of 35.9 on the CBI; range, 0–76, maximum possible score, 88).
The survey was very well accepted by caregivers participating in the study. Only 3 caregivers did not provide answers to some of the multiple-choice questions (answers not received corresponded to the following questions: recognition by other family members, recourse to private insurance and satisfaction with NC).
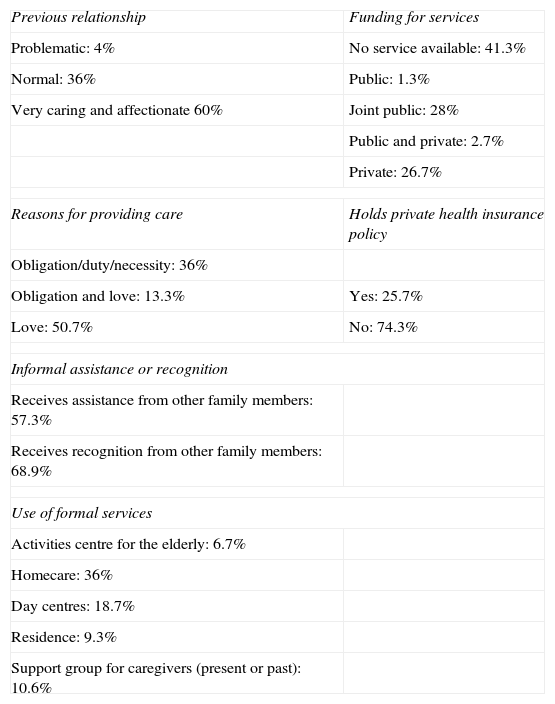
Survey questions related to time providing care appear at the end of Table 1. Results for all other questions on the survey are presented in Table 2. In answering “What motivates you to care for your family member?” (with the possibility of selecting a multiple-choice answer or responding freely), reasons given were love or friendship (50%), obligation or necessity (43%) and other (7%). Caregivers described the previous relationship with the patient as problematic (2.7%), normal (36.5%) or very caring and affectionate (60.9%). Only 56.8% of the caregivers received help from other family members, but in answer to the following question, 65.5% believed that they received recognition for their caregiving activity.
Results from the caregiver survey.
| Previous relationship | Funding for services |
| Problematic: 4% | No service available: 41.3% |
| Normal: 36% | Public: 1.3% |
| Very caring and affectionate 60% | Joint public: 28% |
| Public and private: 2.7% | |
| Private: 26.7% | |
| Reasons for providing care | Holds private health insurance policy |
| Obligation/duty/necessity: 36% | |
| Obligation and love: 13.3% | Yes: 25.7% |
| Love: 50.7% | No: 74.3% |
| Informal assistance or recognition | |
| Receives assistance from other family members: 57.3% | |
| Receives recognition from other family members: 68.9% | |
| Use of formal services | |
| Activities centre for the elderly: 6.7% | |
| Homecare: 36% | |
| Day centres: 18.7% | |
| Residence: 9.3% | |
| Support group for caregivers (present or past): 10.6% | |
Few caregivers used formal social or health care services (home care, day centres, etc). The most commonly used service was home care (provided to 36% of patients) in the form of general domestic help not specifically trained for dementia patients. No additional services were provided to 41% of the patient total (Table 2).
Most caregivers expressed satisfaction with both primary care centres and neurology care clinics, although they were more satisfied with the NC (Wilcoxon test, Z=−2.731, P=.006) (Fig. 1). The main reasons cited for satisfaction with both NC and PC, given as free answers, were “friendly and personalised service” and “professionalism”.
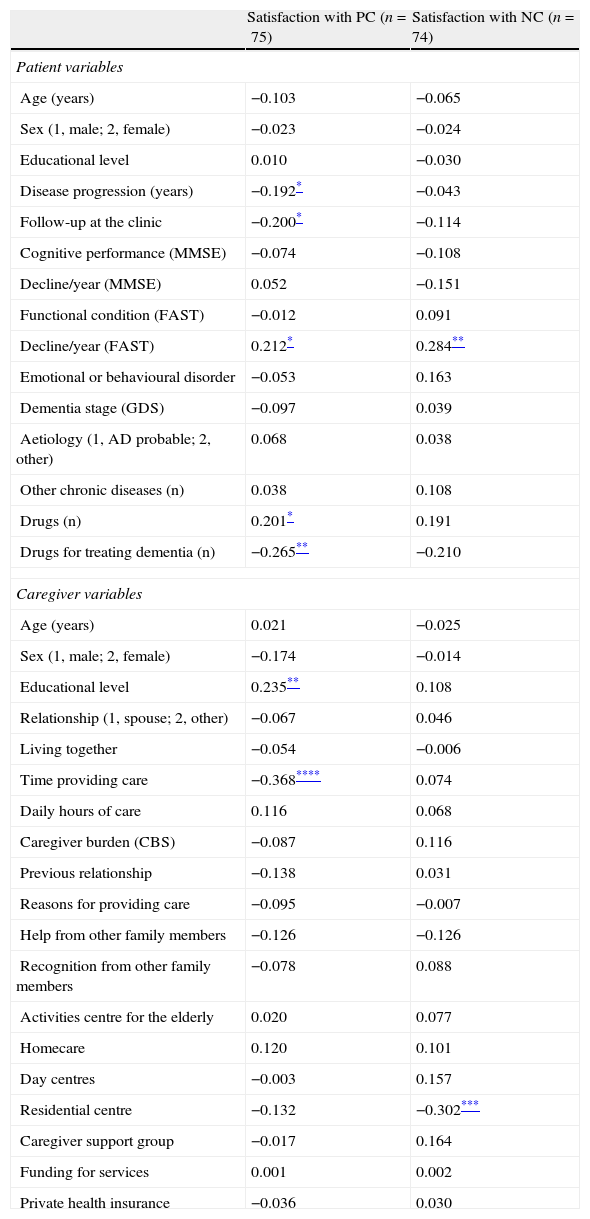
Caregivers who expressed less satisfaction with PC were those who had been providing care for longer periods of time, those whose family member was taking more drugs specifically for dementia, and caregivers with a lower educational level. This only reached the moderate correlation range in the case of longer time providing care (r=0.37, P<.005). Lower satisfaction with NC was associated, to a lesser degree, with institutionalised patients and slower functional decline (Table 3).
Correlates of caregivers’ satisfaction with health care.
| Satisfaction with PC (n=75) | Satisfaction with NC (n=74) | |
| Patient variables | ||
| Age (years) | −0.103 | −0.065 |
| Sex (1, male; 2, female) | −0.023 | −0.024 |
| Educational level | 0.010 | −0.030 |
| Disease progression (years) | −0.192* | −0.043 |
| Follow-up at the clinic | −0.200* | −0.114 |
| Cognitive performance (MMSE) | −0.074 | −0.108 |
| Decline/year (MMSE) | 0.052 | −0.151 |
| Functional condition (FAST) | −0.012 | 0.091 |
| Decline/year (FAST) | 0.212* | 0.284** |
| Emotional or behavioural disorder | −0.053 | 0.163 |
| Dementia stage (GDS) | −0.097 | 0.039 |
| Aetiology (1, AD probable; 2, other) | 0.068 | 0.038 |
| Other chronic diseases (n) | 0.038 | 0.108 |
| Drugs (n) | 0.201* | 0.191 |
| Drugs for treating dementia (n) | −0.265** | −0.210 |
| Caregiver variables | ||
| Age (years) | 0.021 | −0.025 |
| Sex (1, male; 2, female) | −0.174 | −0.014 |
| Educational level | 0.235** | 0.108 |
| Relationship (1, spouse; 2, other) | −0.067 | 0.046 |
| Living together | −0.054 | −0.006 |
| Time providing care | −0.368**** | 0.074 |
| Daily hours of care | 0.116 | 0.068 |
| Caregiver burden (CBS) | −0.087 | 0.116 |
| Previous relationship | −0.138 | 0.031 |
| Reasons for providing care | −0.095 | −0.007 |
| Help from other family members | −0.126 | −0.126 |
| Recognition from other family members | −0.078 | 0.088 |
| Activities centre for the elderly | 0.020 | 0.077 |
| Homecare | 0.120 | 0.101 |
| Day centres | −0.003 | 0.157 |
| Residential centre | −0.132 | −0.302*** |
| Caregiver support group | −0.017 | 0.164 |
| Funding for services | 0.001 | 0.002 |
| Private health insurance | −0.036 | 0.030 |
PC: primary care; NC: neurology clinic; AD: Alzheimer Disease; BI: burden interview17; FAST: stage according to functional assessment screening tool15; GDS: global deterioration scale16; AChEI: acetylcholinesterase inhibitor; MMSE: mini-mental state examination.14
The Spearman correlation coefficient is shown (<0.20, negligible; 0.20–0.34, slight correlation; 0.35–0.50, moderate correlation; >0.50, strong correlation.18
Over a 2-month period in a general neurology clinic, we identified 83 patients with a previous diagnosis of dementia who attended their appointments accompanied by a non-professional primary caregiver. These figures represent a rate of 2–3 appointments for dementia patients per day (in a clinic receiving 10 new patients and 10 follow-up appointments 4 days a week). They attest to both the workload associated with treating dementia in NCs7 and to the irreplaceable role played by the family caregiver.
In line with prior studies undertaken in Spain, most of the patients were very elderly women with a low educational level, dementia due to AD,5,9 and cared for by their daughters.9,12 The yearly decrease of 3 points on the MMSE which we observed is greater than that described in studies conducted under normal clinical practice conditions, but we must point out that our study did not exclude patients due to aetiology of the dementia or to comorbidity.19 It would therefore seem that our study sample represents most of the DPs that are seen at PC centres and specialist clinics in Spain.
Caregivers who had been providing care for longer periods of time were less satisfied with PC in particular (Table 3). Prolonged and continuous contact of caregivers with PC professionals may have led to decreased motivation or “burnout” in both parties. Several remedies must be applied to this situation. Obviously, professionals need more training and time for attending dementia patients in PC centres. PC professionals could also establish closer contact with specialists for cases in which caregivers are unmotivated or faced with a heavy burden. In addition, healthcare resources, especially day centres and programmes for caregivers, should be more available and accessible. In addition to decreasing the time spent providing care (objective burden), day centres are staffed by professionals (therapists, social workers, etc) who respond to caregivers’ considerable demand for training and support.20 On the other hand, programmes specifically designed to aid caregivers, which are usually created by family member support groups, social services or PC centres, increase caregivers’ psychological well-being and delay institutionalisation.21 Unfortunately, only 18.7% of patients in our series made use of a day centre, and only 10.6% of caregivers had participated in a specific training or support programme (Table 2). This is especially worrisome in a sample in which more than half of all patients (59%) had moderate or severe dementia (Table 1).
Satisfaction with NC was lower among caregivers of institutionalised patients, although the correlation was weak (r=−0.30) (Table 3) and there were only 7 institutionalised patients in the sample. While the study contains the limitations listed above, this finding should be examined by neurologists, and perhaps by other specialists, in light of the possibility of there being lower levels of involvement and commitment in the care for these patients.
All in all, the main finding from this study was that caregivers expressed a high level of satisfaction with both PC and NCs (Fig. 1). The finding that the level of satisfaction was slightly lower with respect to PC is questionable, since the survey was administered after an appointment in the NC by personnel employed there. This consideration makes the high level of satisfaction with PC (84% stated they were quite or very satisfied) all the more valid and relevant.
A very few previously published studies address the issue of caregiver satisfaction in healthcare for dementia patients. To the authors’ best knowledge, this is the first study to measure caregivers’ levels of satisfaction with both PC and NCs, and analyse possible determining factors. One study carried out in Spain included 829 caregivers for AD patients treated with an acetylcholinesterase inhibitors or memantine, under the care of an outpatient clinic specialised in neurology, geriatric medicine or psychiatry. Satisfaction with medical care was high in general, with mean satisfaction (SD) at 77.3 (20.8) on a scale of 0–100.9 Another study analysed satisfaction with a telephone consult system in a dementia unit. High or very high levels of satisfaction were reported by 86.5% of caregivers.12
What might explain such high levels of satisfaction, given a panorama of lack of resources and the patient's illness in which we would expect caregivers to be dissatisfied?11,22,23 In this study, the neurologist responsible for the NC was especially dedicated to both dementia research and clinical care for dementia (offering hospital consults as a specialist in the field one day per week). On the other hand, 75% of patients received a specific treatment for dementia (acetylcholinesterase inhibitors, memantine or both) (Table 1). This percentage was somewhat lower than that described in another large-scale study carried out in Spain.18 However, neither increased use of drugs specific to dementia nor less cognitive or functional decline was associated with a higher level of satisfaction. In fact, tendencies and associations were observed in the opposite sense (Table 3). What would then explain the caregivers’ satisfaction?
It is clear that the NC team which undertook this study (a nurse, a resident and a neurologist) was fully motivated and properly prepared to make full use of resources available to it. Another important factor is that more than half of the caregivers characterised their previous relationship with the patient as “very caring and affectionate” and cited “love” as the main reason they provided care (Table 2). This convergence of positive factors and human attitudes therefore explains the level of satisfaction. These factors and attitudes must be strengthened by health care and social decision-makers. Special training and dedication in specific diseases should be promoted, and more resources should be available to caregivers.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Olazarán Rodríguez J, et al. Asistencia sanitaria en las demencias: satisfacción y necesidades del cuidador. Neurología. 2012;27:189–96.