Obstructive sleep apnoea syndrome (OSAS) has numerous implications for health and can affect neurocognitive functions in patients.
ObjectiveTo evaluate the neuropsychological functions most affected by OSAS, the factors associated with OSAS severity that are related to those functional limitations, and the effect of therapy with continuous positive airway pressure.
Patients and methodThe sample consisted of 60 participants: 30 patients diagnosed with OSAS (clinical group) and 30 people without the disorder (control group). Memory, intellectual processes, and attention were analysed with selected subtests from the Luria-Nebraska neuropsychological battery (immediate memory, logical memory, intellectual processes, and attentional control subtests).
ResultsPatients obtained significantly lower scores than controls in most of the areas evaluated. Associations were identified between subjective sleep quality and conceptual activity (r=−0.279; p<.05) and attentional control (r=−0.392; p<.01); between oxygen saturation and both immediate memory (r=0.296; p<.05) and thematic drawings (r=0.318; p<.05); and between apnoea–hypopnoea index and immediate memory (r=−0.303; p<.05), logical memory (r=−0.359; p<.01), and thematic drawings (r=−0.302; p<.05). Continuous positive airway pressure was shown to be effective (p=.03) only for improving immediate memory in patients with OSAS.
ConclusionsPatients with severe OSAS showed memory and attentional limitations, associated with poorer quality of sleep and with worst AHI and SaO2 mean. The CPAP use improved memory of the patients evaluated.
El síndrome de apnea-hipopnea del sueño (SAHS) tiene numerosas repercusiones sobre la salud y puede afectar a las funciones neurocognitivas de los pacientes.
ObjetivoInvestigar las funciones neuropsicológicas que resultan más afectadas por el SAHS, los factores asociados a la gravedad del SAHS relacionados con tales limitaciones y el efecto de la terapia con presión positiva continua en la vía aérea.
Pacientes y métodoLa muestra estuvo compuesta por 60 participantes: 30 pacientes con diagnóstico de SAHS (grupo clínico) y 30 personas sin él (grupo control). La memoria, los procesos intelectuales y la atención fueron analizados por los subtests de la batería neuropsicológica de Luria-DNA (subtest de memoria inmediata, memoria lógica, dibujos temáticos y textos, actividad conceptual y discursiva y control atencional).
ResultadosLos pacientes mostraron puntuaciones significativamente inferiores a los controles en la mayoría de las áreas evaluadas. Se encontraron asociaciones de la calidad de sueño subjetiva con la actividad conceptual (r=−0,279; p<0,05) y con el control atencional (r=−0,392; p<0,01); de la saturación media de oxígeno con la memoria inmediata (r=0,296; p<0,05) y con los dibujos temáticos (r=0,318; p<0,05); del índice de apnea-hipopnea con la memoria inmediata (r=−0,303; p<0,05), con la memoria lógica (r=−0,359; p<0,01) y con los dibujos temáticos (r=−0,302; p<0,05) de la muestra total. La presión positiva continua en la vía aérea resultó eficaz solamente en la mejora de la memoria inmediata (p=0,03) de los pacientes con SAHS.
ConclusionesLos pacientes con SAHS grave mostraron alteraciones atencionales y mnésicas relacionadas con un empeoramiento de la calidad del sueño, con unos peores índices de apnea-hipopnea y saturación media de oxígeno. El tratamiento con presión positiva continua en la vía aérea mejoró el rendimiento en la memoria de los pacientes.
Obstructive sleep apnoea–hypopnoea syndrome (OSAS) is a disorder characterised by recurrent episodes of limited air flow during sleep leading to low oxygen saturation (O2sat) and micro-arousals.1 Despite being an underdiagnosed disease, in the Western world 24% of middle-aged men and 9% of middle-aged women have OSAS.2 Prevalence increases with age3 and is higher in populations with high obesity rates. OSAS has been linked to metabolic4 and cardiovascular5 disorders and is associated with high mortality rates.6 Patients with this disease have been observed to present a higher risk of traffic7 and occupational8 accidents.
Presence of OSAS negatively impacts patients’ quality of life9 since it interferes with daily activities and social relationships. Patients with OSAS usually display lower mood states with higher levels of anxiety and depression,10 a lack of vitality, and fatigue.11 The symptoms with the greatest impact on daily life are excessive daytime somnolence (EDS) and tiredness, which are caused by frequent arousals during the night and poor sleep quality. OSAS and somnolence also have a negative impact in the workplace as they lead to poor work performance and absenteeism.12,13
Cognitive deficits are frequently mentioned among the numerous consequences of OSAS. Several studies have analysed the impact of OSAS on such neuropsychological functions as memory, vigilance, attention, executive function, and reaction time.14–17 No effects of this syndrome on intellectual abilities have been observed.18 According to Alchanatis et al.,19 a higher level of intelligence may be a protective factor against OSAS-related cognitive deficits. Several studies have attempted to find the factors provoking neuropsychological alterations in patients with OSAS.20–23 According to some authors, these limitations could be directly linked to OSAS severity, measured with the apnoea–hypopnoea index (AHI),20,21 whereas other researchers suggest that oxygen desaturation is the agent responsible for poorer cognitive performance in these patients.22,23 However, there is no consensus on the impact of OSAS on neurocognitive function and the factors responsible for this damage.
Continuous positive airway pressure (CPAP) is the treatment of choice for OSAS.24 According to the literature, CPAP can improve EDS and mood even after very short periods of treatment.25 Several studies have tried to explain the effect of CPAP on neurocognitive deficits, but no definitive conclusions have been reached as to the effects of CPAP on these deficits or even whether they are reversible. Barbé et al.26 conducted a randomised study with a control group treated with subtherapeutic CPAP and found no significant changes in cognitive performance in the domains of attention, vigilance, visual memory, coordination, or mental control after 6 weeks of CPAP therapy. A meta-analysis conducted by Kylstra et al.27 was aimed at analysing the effectiveness of CPAP for rehabilitating neurocognitive function. According to their results, the effects of CPAP are limited and significant only in the case of attention. However, other review articles report significant effects of CPAP on vigilance, memory, and such executive functions as working memory, mental flexibility, verbal fluency, reasoning, and behavioural inhibition.14,17,22,28
The lack of agreement between the conclusions of these studies may be due to the differences in methodology and the analysed neuropsychological measurements, the heterogeneity of patients’ clinical characteristics, and adherence to CPAP therapy.25 In light of the lack of consensus on the consequences of OSAS on neurocognitive skills and the effects of CPAP on these deficits, our study aimed to investigate the neuropsychological functions most affected by OSAS, the factors associated with OSAS that are related to these functional limitations, and the medium-term effect of CPAP therapy.
MethodsPatientsWe conducted a quasi-experimental study with a pre- and a post-intervention evaluation including 60 participants: 30 patients diagnosed with OSAS and treated with CPAP (clinical group), and 30 people with no OSAS (control group). Only active workers willing to participate and sign the informed consent form were selected. Exclusion criteria were a diagnosis of other sleep disorders or severe incapacitating diseases (NYHA class III congestive heart failure, hepatic cirrhosis, or kidney failure treated with dialysis), addiction to alcohol or other substances, and being treated with neuroleptics, tranquillisers, or any other drug which may alter sleep or cause daytime somnolence.
ProcedureData were collected between 2011 and 2012 in the unit for respiratory sleep disorders at Hospital Universitario Reina Sofía in Córdoba (Spain). All participants filled out a questionnaire aimed at gathering sociodemographic variables and data on general state of health and subjective symptoms of OSAS. Both the control group and the OSAS group were evaluated with the Luria-DNA neuropsychological battery.29 Patients with OSAS who were prescribed CPAP therapy underwent a neuropsychological evaluation before starting treatment and after 4 months of treatment.
Polysomnographic evaluationAll participants came from the same centre and were recruited consecutively. A diagnosis of OSAS was established based on an all-night sleep study conducted at the unit for respiratory sleep disorders of our hospital. We used 3 electroencephalography channels (F4-M1, C4-M1, and O2-M1), 2 electrooculography channels, 2 submental and 2 tibial electromyography channels, and an electrocardiography channel. We recorded peripheral O2sat, heart rate, and snoring frequency. Airflow was measured with a nasal pressure cannula and a thermistor. Elastic belts were used to measure thoracic and abdominal respiratory effort. Sleep studies were manually analysed by experts in accordance with the recommendations of the American Academy of Sleep Medicine.30 A diagnosis of OSAS was established using the AHI: symptomatic patients with an AHI ≥5 were diagnosed with OSAS.
Neuropsychological assessmentDaytime somnolence was assessed using the Epworth Sleepiness Scale31,32 and subjective sleep quality was measured with the Pittsburgh Sleep Quality Index.33,34 The neuropsychological evaluation focused on assessing 3 domains: memory, intellectual/conceptual processes, and attention. We used the following subtests from the Luria-DNA battery: immediate memory, logical memory, themed pictures and text, conceptual and discursive activity, and attention control.29 The Luria-DNA battery is a tool for analysing higher neuropsychological processes in adults. This battery includes 9 tests which assess different cognitive functions and skills grouped into 5 domains: (i) visuospatial (visual perception and spatial orientation subtests), (ii) language (receptive and expressive language subtests), (iii) memory (immediate memory and logical memory subtests), (iv) intellectual processes (themed pictures and text subtest and conceptual and discursive activity subtest), and (v) attention (attention control subtest). The factor analyses performed by the authors yielded a solution of 5 factors which confirms the factorial structure of the subtests included in the battery. Reliability analysis shows high scores in all the domains analysed (0.66 for memory, 0.75 for intellectual processes, and 0.83 overall). The neuropsychological tests were administered by a trained psychologist. Each patient was examined before and after treatment by the same rater.
Statistical analysisSample characteristics were expressed as means and standard deviations for quantitative variables, and as percentages and absolute values for qualitative variables. We used the t test to compare neuropsychological skills before and after CPAP therapy, and the Pearson chi-square test for categorical variables. The Pearson correlation coefficient was used to analyse the relationship between the variables related to OSAS and cognitive alterations. We used SPSS software v. 20.0.
The study was approved by the Clinical Research Ethics Committee of the hospital participating in the study. Subjects participated voluntarily, were duly informed regarding the study aims, and signed informed consent forms. We followed the rules proposed by Hartley to draft this article.35
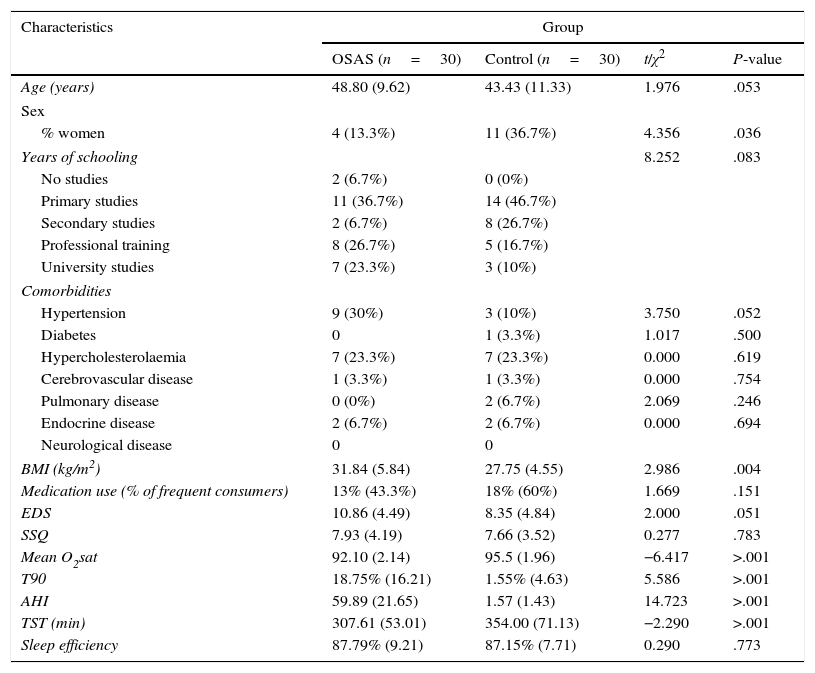
ResultsThe sample included 45 men (75%) and 15 women (25%) aged between 25 and 65 years (mean age, 46.12±10.77) and with a body mass index of 29.83±5.60kg/m2. Table 1 displays the sociodemographic, clinical, and polysomnographic characteristics of the sample. As the table shows, no age-related differences were seen between groups. However, we did find differences in sex and body mass index. Both groups obtained similar scores on the Epworth Sleepiness Scale and the Pittsburgh Sleep Quality Index but showed different scores for most polysomnographic variables.
Sociodemographic, clinical, and polysomnographic characteristics of patients with OSAS and controls.
| Characteristics | Group | |||
|---|---|---|---|---|
| OSAS (n=30) | Control (n=30) | t/χ2 | P-value | |
| Age (years) | 48.80 (9.62) | 43.43 (11.33) | 1.976 | .053 |
| Sex | ||||
| % women | 4 (13.3%) | 11 (36.7%) | 4.356 | .036 |
| Years of schooling | 8.252 | .083 | ||
| No studies | 2 (6.7%) | 0 (0%) | ||
| Primary studies | 11 (36.7%) | 14 (46.7%) | ||
| Secondary studies | 2 (6.7%) | 8 (26.7%) | ||
| Professional training | 8 (26.7%) | 5 (16.7%) | ||
| University studies | 7 (23.3%) | 3 (10%) | ||
| Comorbidities | ||||
| Hypertension | 9 (30%) | 3 (10%) | 3.750 | .052 |
| Diabetes | 0 | 1 (3.3%) | 1.017 | .500 |
| Hypercholesterolaemia | 7 (23.3%) | 7 (23.3%) | 0.000 | .619 |
| Cerebrovascular disease | 1 (3.3%) | 1 (3.3%) | 0.000 | .754 |
| Pulmonary disease | 0 (0%) | 2 (6.7%) | 2.069 | .246 |
| Endocrine disease | 2 (6.7%) | 2 (6.7%) | 0.000 | .694 |
| Neurological disease | 0 | 0 | ||
| BMI (kg/m2) | 31.84 (5.84) | 27.75 (4.55) | 2.986 | .004 |
| Medication use (% of frequent consumers) | 13% (43.3%) | 18% (60%) | 1.669 | .151 |
| EDS | 10.86 (4.49) | 8.35 (4.84) | 2.000 | .051 |
| SSQ | 7.93 (4.19) | 7.66 (3.52) | 0.277 | .783 |
| Mean O2sat | 92.10 (2.14) | 95.5 (1.96) | −6.417 | >.001 |
| T90 | 18.75% (16.21) | 1.55% (4.63) | 5.586 | >.001 |
| AHI | 59.89 (21.65) | 1.57 (1.43) | 14.723 | >.001 |
| TST (min) | 307.61 (53.01) | 354.00 (71.13) | −2.290 | >.001 |
| Sleep efficiency | 87.79% (9.21) | 87.15% (7.71) | 0.290 | .773 |
SSQ: subjective sleep quality; EDS: excessive daytime somnolence; AHI: Apnoea–Hypopnoea Index; BMI: body mass index; mean O2sat: mean oxygen saturation in blood; OSAS: obstructive sleep apnoea–hypopnoea syndrome; t: t test; TST: total sleep time; T90; percentage of time with an oxygen saturation below 90%; χ2: Pearson chi-square test.
Qualitative variables are presented as percentages and absolute values, and quantitative variables as means and standard deviations.
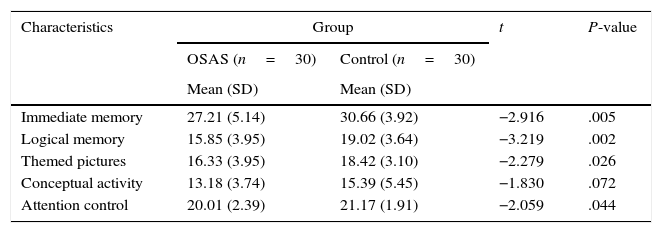
Table 2 compares the scores on each neuropsychological variable between the OSAS group and the control group. The control group scored higher on many neuropsychological tests; differences were statistically significant for all of them except for the conceptual activity test. If we compare scores between groups, we can observe that patient scores on the test on comprehension of themed pictures and text and the attention control tests are in the 50th percentile, while scores on the remaining tests fall between the 31st and 7th percentiles. Scores obtained by the control group were between the 50th and 69th percentiles.
Evaluation of neuropsychological variables in the 2 study groups.
| Characteristics | Group | t | P-value | |
|---|---|---|---|---|
| OSAS (n=30) | Control (n=30) | |||
| Mean (SD) | Mean (SD) | |||
| Immediate memory | 27.21 (5.14) | 30.66 (3.92) | −2.916 | .005 |
| Logical memory | 15.85 (3.95) | 19.02 (3.64) | −3.219 | .002 |
| Themed pictures | 16.33 (3.95) | 18.42 (3.10) | −2.279 | .026 |
| Conceptual activity | 13.18 (3.74) | 15.39 (5.45) | −1.830 | .072 |
| Attention control | 20.01 (2.39) | 21.17 (1.91) | −2.059 | .044 |
SD: standard deviation; OSAS: obstructive sleep apnoea–hypopnoea syndrome; t: t test.
The scores reported are raw scores. Score range for each subtest: immediate memory: 0-42; logical memory: 0-24; themed pictures: 0-23; conceptual activity: 0-27; attention control: 0-22.
Table 3 shows correlations between the subjective and objective variables related to OSAS and the neurocognitive variables analysed in the total patient sample. This table shows a connection between sleep quality, mean O2sat, AHI, and some of the analysed neurocognitive functions. The analysis of correlations between clinical and polysomnographic variables and neurocognitive functions conducted in patients with OSAS showed an association only between AHI, immediate memory (r=0.437; P=.023), and comprehension of themed pictures and text (r=0.484; P=.010).
Association between sleep and cognitive variables in the total sample.
| Immediate memory | Logical memory | Themed pictures | Conceptual activity | Attention control | |
|---|---|---|---|---|---|
| EDS | −0.142 | −0.014 | 0.038 | −0.069 | −0.206 |
| SSQ | −0.208 | −0.048 | −0.126 | −0.279* | −0.392** |
| Mean O2sat | 0.296* | 0.205 | 0.318* | 0.122 | 0.119 |
| AHI | −0.303* | −0.359** | −0.302* | −0.181 | −0.158 |
SSQ: subjective sleep quality; EDS: excessive daytime somnolence; AHI: Apnoea–Hypopnoea Index; mean O2sat: mean blood oxygen saturation.
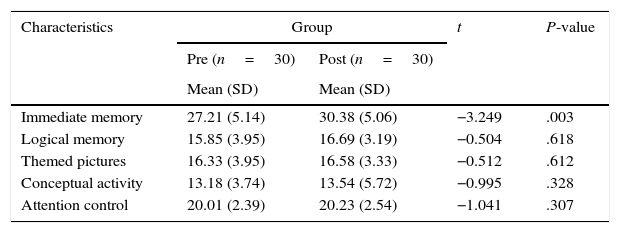
The patients treated with CPAP reported a mean use of the therapy of 6.7±0.7 days per week, and 6.1±0.5hours per night. With regards to the effects of CPAP on the subjective variables of EDS and sleep quality, we observed a significant improvement only in the EDS (pre-intervention score: 10.91±4.2; post-intervention score: 8.18±5.0; P=.013). Table 4 compares scores for neuropsychological variables before CPAP therapy and after 4 months of therapy. We observed statistically significant improvements only in the immediate memory subtest (memory domain). Compared with the score of the general population,29 the patients’ scores on the immediate memory test reached the 50th percentile of the scales. In the rest of the analysed domains, especially logical memory and conceptual and discursive activity, scores are below the 50th percentile even after 4 months of CPAP therapy.
Evaluation of neuropsychological variables in the group of patients with OSAS before and after 4 months of CPAP treatment.
| Characteristics | Group | t | P-value | |
|---|---|---|---|---|
| Pre (n=30) | Post (n=30) | |||
| Mean (SD) | Mean (SD) | |||
| Immediate memory | 27.21 (5.14) | 30.38 (5.06) | −3.249 | .003 |
| Logical memory | 15.85 (3.95) | 16.69 (3.19) | −0.504 | .618 |
| Themed pictures | 16.33 (3.95) | 16.58 (3.33) | −0.512 | .612 |
| Conceptual activity | 13.18 (3.74) | 13.54 (5.72) | −0.995 | .328 |
| Attention control | 20.01 (2.39) | 20.23 (2.54) | −1.041 | .307 |
CPAP: continuous positive airway pressure; SD: standard deviation; OSAS: obstructive sleep apnoea–hypopnoea syndrome; t: t test.
The scores reported are raw scores. Score range for each subtest: immediate memory: 0–42; logical memory: 0–24; themed pictures: 0–23; conceptual activity: 0–27; attention control: 0–22.
Our study aimed to determine the neuropsychological functions most affected by OSAS, analyse the factors associated with OSAS severity that are related to those functional limitations, and measure the medium-term effects of CPAP therapy. Our results indicate that OSAS has a negative impact on a number of cognitive functions, including memory, and such intellectual processes as conceptual and discursive activity. Likewise, our study shows an association between subjective sleep quality, conceptual activity, and attention control, whereas no associations were found between these functions and EDS. We also observed that some variables associated with OSAS severity, such as mean O2sat and AHI, are linked to memory and the comprehension of themed pictures and text. CPAP therapy seems effective in improving immediate memory only; no significant changes were observed in the remaining neurocognitive variables analysed.
In our study, patients with OSAS scored significantly lower than people without the disorder in most of the evaluated neurocognitive functions. If we compare the data from the OSAS group using the scales proposed by Manga and Ramos,29 we observe that patients with OSAS obtain scores below the 50th percentile in most of the analysed neuropsychological domains, with the exception of attention and comprehension of themed pictures and text. These data partly confirm results from other studies reporting neuropsychological symptoms in patients with OSAS. According to a study by Bawden et al.,36 performance in the memory domain was poorer in patients with OSAS than in controls. These authors, however, also reported limitations in the attention domain. Ferini-Strambi et al.37 found statistically significant differences between patients with OSAS and control subjects with regards to different neurocognitive functions, such as sustained attention, visuospatial learning, executive function, motor performance, and constructional abilities. However, no differences were observed in memory. A review study by Olaithe and Bucks14 showed that OSAS has an important negative impact on such executive functions as fluid reasoning, inhibition, shifting, and updating.
Our study analysed which subjective and objective variables linked to OSAS were associated with neurocognitive dysfunction in these patients. Our data reveal a significant correlation between subjective sleep quality and the cognitive variables of conceptual activity and attention control, unlike in the case of EDS. Our results agree with other studies that report no correlation between EDS and neurocognitive functions.38,39 Our study, especially in the group of patients with OSAS, reveals a relationship between AHI and limitations in the domains of memory and comprehension of themed pictures and text. The studies addressing this topic do not agree on the connection between the polysomnographic variables associated with OSAS and neurocognitive functions. For example, Ferini-Strambi et al.37 found a relationship between verbal fluency and time of sleep spent with O2sat below 90% (T90), and between visuoconstructional abilities and minimum O2sat, but they found no association between memory and respiratory or sleep indices. Quan et al.23 conducted a multi-centre, randomised, double-blind study including a very large sample of patients with OSAS, and also found no relationships between AHI and neurocognitive functions. These authors only observed associations between the percentage of time in stage 1 sleep and psychomotor functions, as well as between O2sat and intelligence, reaction time, calculation ability, and auditory information processing speed. However, similarly to our study, other authors have reported strong relationships between AHI and cognitive deficits in patients with OSAS.21,28
Our study demonstrated that CPAP showed limited effectiveness in improving neuropsychological symptoms; this treatment results in significant changes only in the memory domain. Nevertheless, Antic et al.40 reported differences between scores obtained before and after 3 months of CPAP therapy in the domains of verbal memory and executive functions, although not in reaction times. Lau et al.41 obtained similar results since the performance of treated patients was comparable to that of the control group in basic working memory tasks; however, these patients still presented significant alterations in more complex functions requiring attention, executive functions, and psychomotor speed. In a study by Kushida et al.,42 CPAP had no effect on neurocognitive functions since the efficacy of the therapy was transient and limited to executive and frontal-lobe function. Lim et al.38 analysed the short-term effects of CPAP therapy (2 weeks) vs oxygen supplementation and placebo-CPAP on neurocognitive functions and reported greater effectiveness of CPAP in comparison with the other treatments only in one neurocognitive task which measured speed of information processing, sustained attention, and alertness.
We should point out that our study presents some limitations. Firstly, we could not analyse the effect of subtherapeutic pressure on the analysed neurocognitive functions due to the lack of a sham-CPAP control group. Furthermore, the sample size of the 2 groups was somewhat small.
In conclusion, our study reveals that OSAS has a number of negative effects on patients’ neurocognitive functions, especially with respect to memory and conceptual activity. Among all subjective and objective variables of OSAS severity, subjective sleep quality, AHI, and mean O2sat were the factors most significantly related with neurocognitive limitations. Likewise, the effectiveness of CPAP therapy was shown to be limited, since only immediate memory improved after 4 months of therapy.
FundingThis article was funded by a training grant for teaching and research staff awarded by the Regional Government of Andalusia to the Department of Personality, Evaluation, and Psychological Treatment of the Faculty of Psychology at the University of Granada, Spain.
Conflict of interestThe authors have no conflict of interest to declare.
This article was possible thanks to a training grant for teaching and research staff specialising in under-researched areas awarded by the Regional Government of Andalusia to the Department of Personality, Evaluation, and Psychological Treatment of the Faculty of Psychology at the University of Granada, Spain.
Please cite this article as: Jurádo-Gámez B, Guglielmi O, Gude F, Buela-Casal G. Efectos del tratamiento con presión positiva continua en la vía aérea sobre las funciones cognitivas en pacientes con apnea del sueño grave. Neurología. 2016;31:311–318.