Cysticercosis is caused by the cestode Taenia solium or pork tapeworm. T. solium infection arises from ingestion of contaminated food or water and ingestion of raw or undercooked pork and may result in taeniasis (caused by the adult tapeworm living in the small intestine) and/or cysticercosis. Neurocysticercosis (NCC) is caused by invasion of the larvae into the central nervous system (CNS) in humans. Cysticercosis is endemic in Central and South America, Sub-Saharan Africa, Indian Ocean and large regions of Asia. However, immigration and travel result in many cases of NCC in non-endemic countries. NCC is the most common parasitic disease of the human central nervous system. The most frequent clinical manifestations of NCC are seizures, headaches, and intracranial hypertension.1 Movement disorders can occur in a small percentage of patients affected by neurocysticercosis, being parkinsonism and ataxia the most common symptoms,2 although tremor was also reported.3 Herein we described a case of neurocysticercosis presenting with dystonic head tremor and partial seizures.
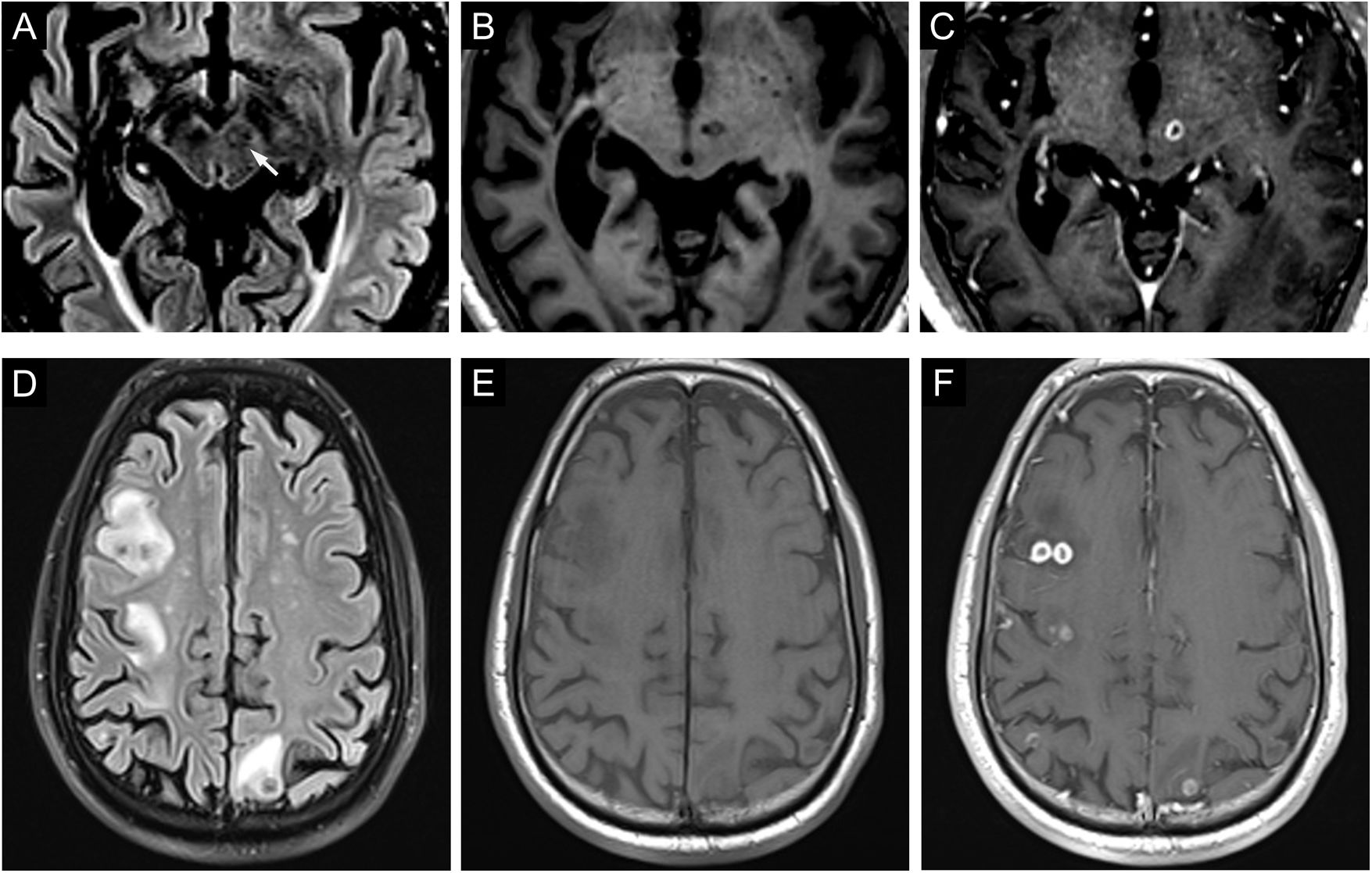
A 49-year-old male patient was admitted to our emergency room because of slow, regular cervical involuntary postural jerks (Video 1), worsening during voluntary movements, which had appeared two days before. Left faciobrachial clonic movements appeared some hours previous to the admission. Level of consciousness was normal. He had a previous history of generalized seizures due to a right parietal subarachnoid hemorrhage occurred several years before. A brain magnetic resonance showed multiple focal, cortical and subcortical, lesions with calcifications and surrounding edema involving both hemispheres, midbrain and cerebellum, suggesting a cysticercoid infection (Fig. 1). One lesion was settled in the left subthalamic and red nuclei. Anti-epileptic drugs were started, with improvement of the faciobrachial clonic movements but without any change in cervical movements. EEG showed no epileptiform activity, although it was performed after starting anti-epileptic drugs. Dystonic head tremor secondary to neurocysticercosis was diagnosed. Treatment with anthelmintic drugs, such as praziquantel or albendazole, was considered; however, the large brain disease led us to delay their use in order to avoid a severe inflammatory reaction. The cephalic movements did not respond to beta-blockers nor to primidone. Partial improvement after botulinum toxin infiltrations was observed.
Top row. (A) Axial fluid-attenuation inversion recovery (FLAIR), (B) axial T1 and (C) axial T1 after Gadolinium administration show a focal enhancing lesion in the subthalamic nucleus expanding to the medial and anterior aspect of left mesencephalon. Additionally, a subcortical right insular and a temporal siderotic lesion causing dilation of the lateral ventricle were observed. Bottom row, axial fluid-attenuation inversion recovery (FLAIR) (D), axial susceptibility weighted images (E) and axial T1 sequence after gadolinium administration (F) show several low T2 signal cortically based lesions with peripheral enhancement and surrounding edema which are consistent with neurocysticercosis in a colloidal-vesicular stage.
Abnormal involuntary movements, such as tremor or dystonia, secondary to lesions involving the dopaminergic nigrostriatal system and the cerebello-thalamo-cortical or dentate-rubro-olivary pathways have been described.4,5 These abnormal movements usually affect upper limbs, although other body parts can be also involved. They commonly develop between 1 and 24 months after the central nervous system insult. It has been hypothesized that this delayed onset might be due to neuronal plastic changes. Imaging studies are usually abnormal, although in some cases no lesion can be demonstrated.6 In the case presented here, the dystonic head tremor was mostly regular, present also during voluntary movements, and its response to botulin toxin infiltrations support its dystonic nature. Probably, we cannot explain the movement disorder of our patient only because of a single brain lesion. However, the presence of a lesion in the subthalamic and left red nucleus, part of the cerebello-thalamo-cortical pathway, could be related to his movement disorder. The faciobrachial clonic movements were considered seizures since they disappeared after initiating antiepileptic drugs.
Although the clinical presentation of neurocysticercosis is wide, movement disorders are not the most frequent phenomenology and they are rare as the initial symptom of this entity. However, the clinical characterization of this infectious disease is still ongoing and we consider that dystonic head tremor should be included as part of its clinical spectrum.
Conflicts of interestThe authors declare no conflict of interests.