Congenital left ventricular aneurysm or diverticulum, recently brought together with the term left ventricular outpouchings (LVO), are infrequent heart defects that can cause embolic phenomena. Although they usually present in isolation, LVOs are sometimes associated with such other defects as patent foramen ovale (PFO).
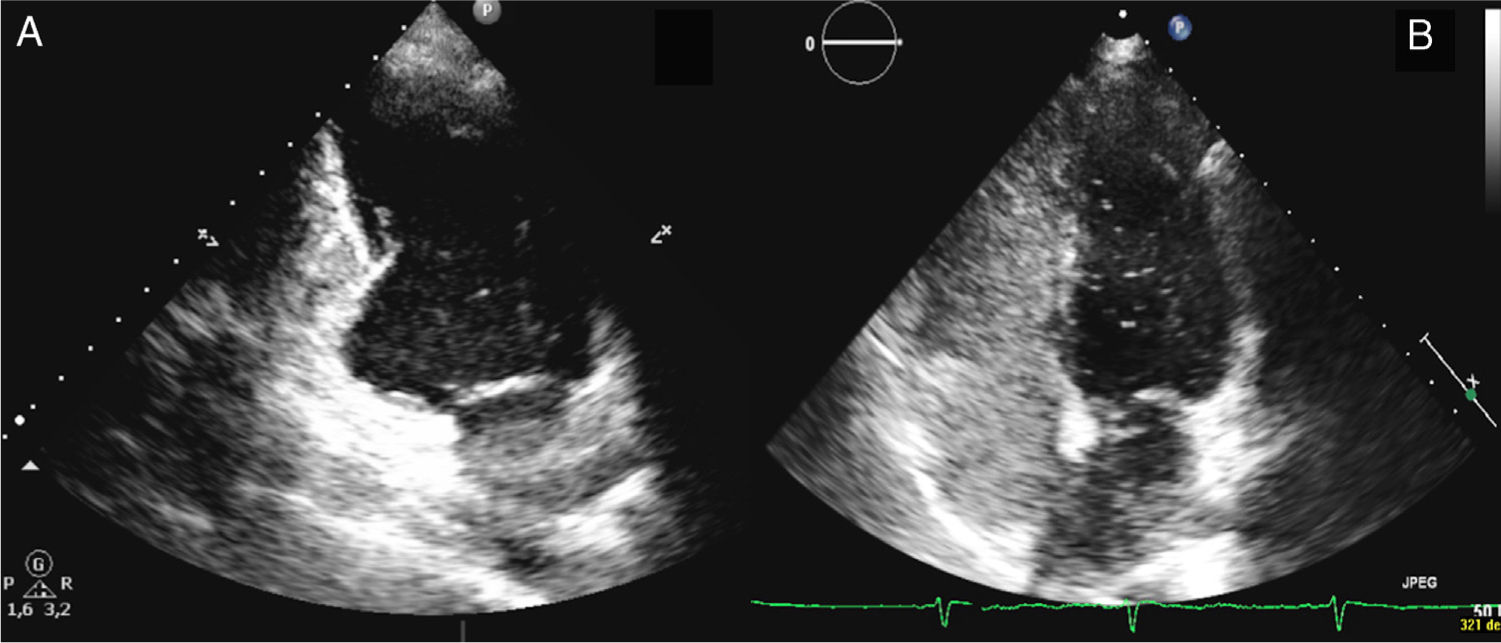
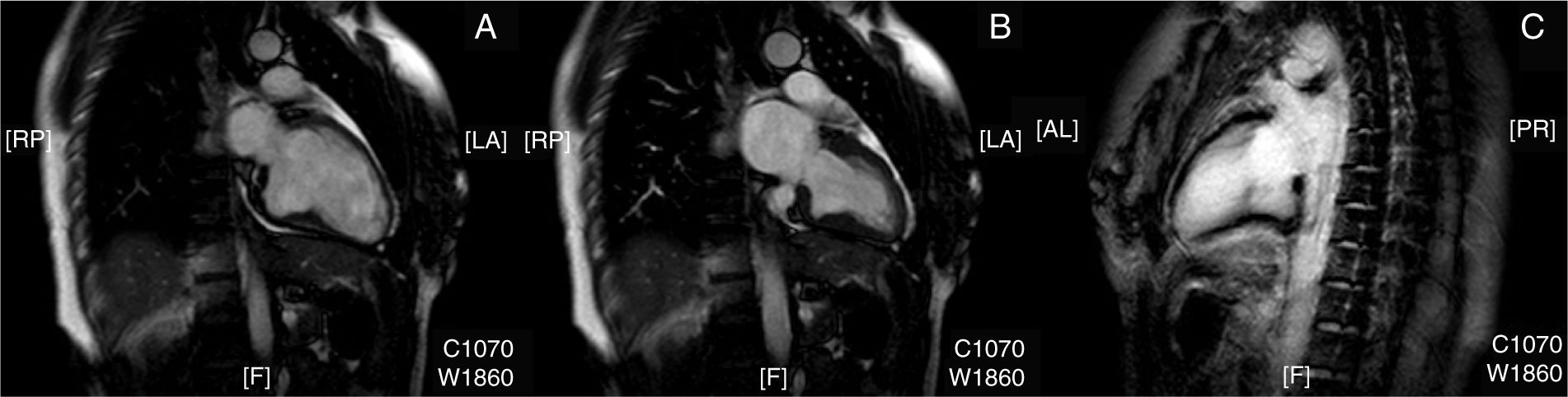
We present the case of a 39-year-old woman, a former smoker previously diagnosed with migraine with visual aura, who attended our emergency department due to difficulty speaking of sudden onset, with no other associated symptom. Physical examination revealed motor aphasia, with normal results in the neurological examination. An electrocardiogram showed sinus rhythm at 72bpm with no alterations; a CT angiography of the brain and aortic trunks revealed millimetric hypointense foci in the cerebellum, compatible with older strokes; no other anomalies were detected. The patient was admitted to the stroke unit, and clinical symptoms completely resolved approximately 2hours after onset. A Doppler ultrasonography of the supra-aortic trunks showed normal findings, and a brain MRI scan confirmed the presence of older small cerebellar infarcts, with no alterations on diffusion sequences. A transthoracic echocardiogram revealed a protrusion of the inferobasal wall of the left ventricle (Fig. 1A) and the presence of PFO after injection of agitated saline solution (Fig. 1B). We also performed a CT angiography of the coronary arteries, which ruled out atherosclerotic disease; a cardiac MRI scan confirmed the presence of the anomaly observed in the transthoracic echocardiogram, connected to the ventricular cavity by a wide neck; wall thickness and contractility (Fig. 2A-B) were normal, and no late gadolinium uptake was observed (Fig. 2C). Approximately 90minutes after symptom onset, the patient fully recovered the ability to speak, remaining asymptomatic during hospitalisation. The case was discussed in a multidisciplinary meeting where we decided to adopt a conservative approach, prescribing oral anticoagulant treatment (acenocoumarol at doses adjusted by the haematology department) and outpatient follow-up.
Congenital left ventricular aneurysm and diverticulum are rare primary heart defects first described in 1816. They may be associated with other cardiac, vascular, and thoracoabdominal malformations; very pronounced cases are part of the pentalogy of Cantrell.1 Two entities have classically been differentiated: aneurysm, defined as an akinetic or dyskinetic protrusion of the ventricular wall with a neck diameter/maximum diameter ratio >1; and diverticulum, characterised by normal contractility and a ratio <1.2 Although this differentiation may seem simple, the literature includes multiple unclear examples, and the terms are even used interchangeably. Therefore, in 2014, Malakan Rad et al.3 developed a new classification aimed at standardising these definitions. Under the common term LVO, they described 4 types of malformations (I, IIa, IIb, and IIc), classified according to the thickness and contractility of the walls.3 LVOs are usually diagnosed incidentally by imaging studies requested for another reason, with symptoms including those secondary to embolic phenomena or heart rate alterations.4
Our patient presented isolated motor aphasia, a frequent manifestation of cardioembolic stroke5; complementary studies revealed an LVO. After ruling out coronary artery disease, we concluded that this finding corresponds to a congenital malformation. After analysing its anatomical characteristics, the lesion is difficult to classify as an aneurysm or a diverticulum following classical criteria, as it presents a neck diameter/maximum diameter ratio >1 (compatible with the first) and normal wall thickness and contractility (suggestive of the second). However, it could be considered a type I LVO according to the Malakan Rad et al.3 classification; therefore, we believe that using this classification may help in homogenising the terms used in reference to these malformations. Furthermore, our patient presented PFO, an association which is not frequently documented in the literature (1% of cases of LVO).4 Copresence of both entities makes it difficult to ascertain the cause of the cerebral ischaemic events. On the one hand, the association of PFO with cryptogenic stroke in young patients seems to be increasingly documented, with some authors estimating it to be 5 times more likely in this patient group than in the general population.6 On the other hand, although LVOs usually progress asymptomatically and are diagnosed incidentally, the number of reported cases of these anomalies associated with stroke is increasing;7 however, this association remains exceptional, as demonstrated by the absence of LVO as the aetiology of cardioembolic stroke in a consecutive series of 402 patients.8 Therefore, and given the controversy regarding treatment of these entities in isolation, we opted to implement oral anticoagulant treatment and outpatient follow-up, with other treatment alternatives such as isolated surgical resection of the LVO or surgical closure of the PFO reserved for the potential case of symptom recurrence.
Please cite this article as: Lapeña-Reguero M, et al. Evaginación ventricular izquierda congénita y foramen oval permeable: una combinación potencialmente embolígena. Neurología. 2020;35:334–335.