Cerebral cavernous malformations (CCM), also known as cavernomas or cavernous haemangiomas, are vascular malformations of the central nervous system characterised by a well-defined collection of enlarged, thin-walled blood vessels with a single layer of endothelium and a thin, fibrous tunica adventitia layer, and containing blood components in different developmental stages.1
CCMs are usually located in the supratentorial region, subcortical parenchyma, basal ganglia, or brainstem.2,3 Their prevalence, formerly estimated at 0.02% to 0.5%, has in recent decades increased to 0.4% to 0.9% due to the introduction of MRI in clinical practice.4
CCMs typically present between the ages of 20 and 40.5 The most frequent clinical symptoms include seizures, headache, focal neurological signs, bleeding, and very occasionally, movement disorders.6 Chorea, in particular, is rare in these patients; when it does occur, it is usually caused by involvement of the caudate nucleus. We present the case of a patient with hemichorea associated with a CCM in the contralateral insula and review published case reports of patients with chorea who were managed without surgery.
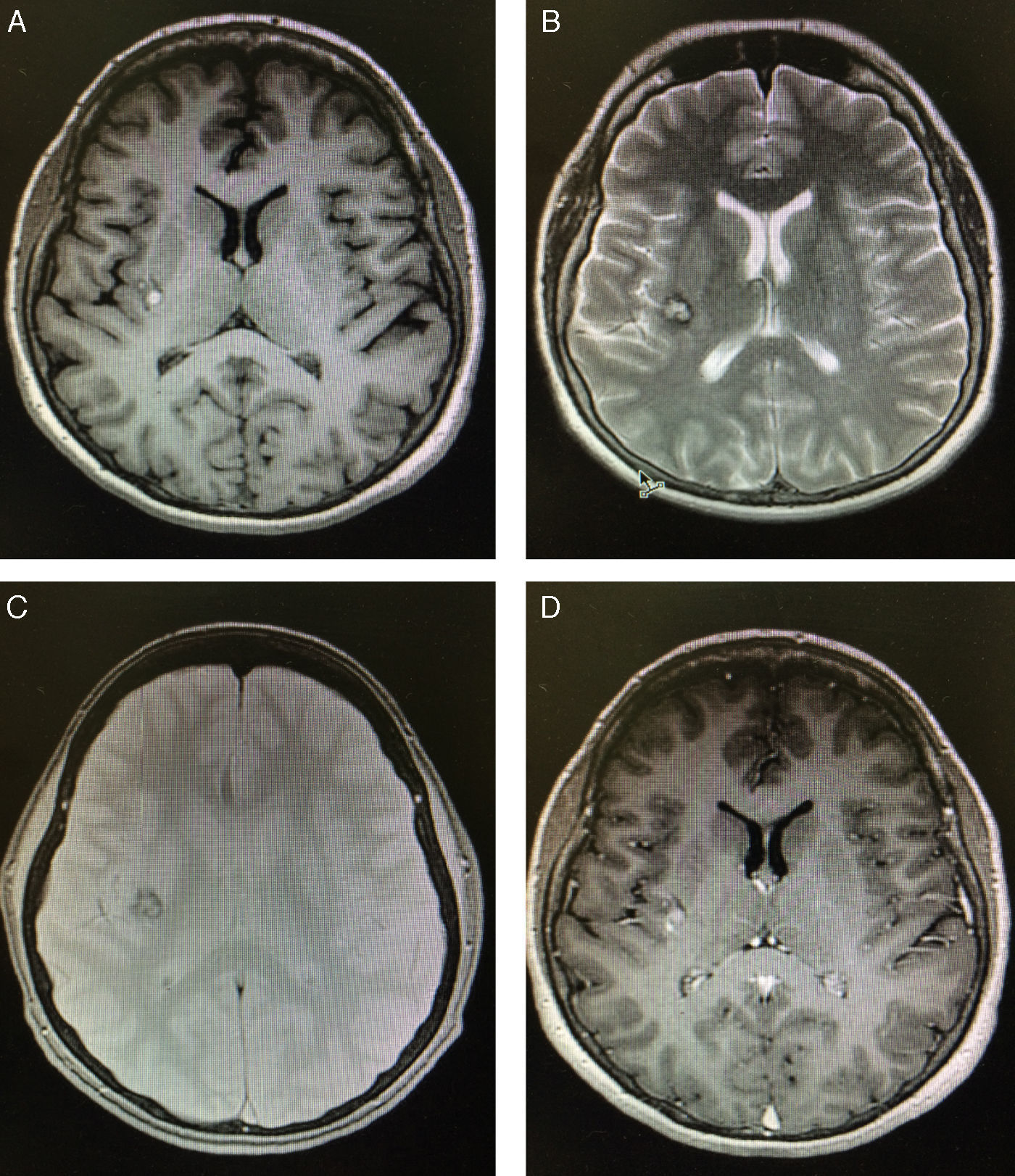
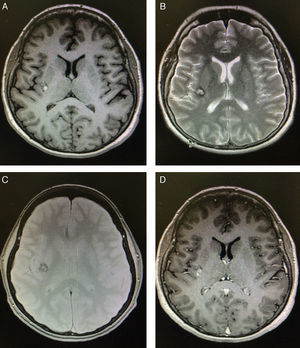
Case reportA 45-year-old woman was brought to the National Institute of Neurology and Neurosurgery in Mexico City due to a one-month history of ataxic gait and involuntary movements in the left side of her body. Left hemichorea had appeared spontaneously. The physical examination detected no alterations, whereas the neurological examination revealed choreic movements which were exacerbated by stress. Cognitive function, muscle strength, sensitivity, and cerebellar function were normal, and the patient displayed no pathological reflexes. An electrocardiogram, a complete blood count, and tests for erythrocyte sedimentation rate, serum electrolyte levels, hepatic and renal function, and thyroid profile all yielded normal results. The patient tested positive for antinuclear antibodies and negative for anticardiolipin antibodies and rheumatoid factor. A cranial CT scan revealed only a small distortion at the level of the posterior portion of the internal capsule. A T1-weighted brain MRI sequence displayed a hyperintense lesion in the right insula; a T2-weighted sequence revealed a heterogeneous hyperintense lesion with a hypointense rim measuring 6.93mm×7.09mm×8.09mm. A gradient-echo sequence displayed an irregular mass with an isointense centre and a hypointense rim, with no mass effect. An additional MRI scan performed 4 months later revealed no changes (Fig. 1).
Brain MRI scan performed 24hours after admission. (A) Non-contrast T1-weighted MRI sequence showing a small, well-defined hyperintense lesion in the right insula. (B) T2-weighted MRI sequence revealing a heterogeneous lesion consisting of a hyperintense area with a hypointense rim; the grey matter is not affected. (C) Gadolinium-enhanced T1-weighted MRI sequence showing homogeneous contrast enhancement. (D) Gradient-echo MRI sequence revealing a lesion in the right insula with a dark rim (haemosiderin), demonstrating a “popcorn” appearance.
Haloperidol dosed at 10mg/day led to complete resolution of choreic movements after 2 months.
DiscussionChorea is characterised by abrupt involuntary movements resulting from a continuous flow of random involuntary muscle contractions.7,8 Onset of chorea may be acute or subacute and may have a number of causes, including infection, autoimmune diseases, genetic mutations, neurodegeneration, infarction, neoplasia, drug use, and metabolic diseases.7 Unilateral choreic movements, known as hemichorea, represent approximately 0.7% of all movement disorders. Hemichorea usually appears in patients with structural conditions, such as vascular lesions in the contralateral side.2 In the light of the above, we concluded that left hemichorea in our patient was caused by the contralateral CCM.
The pathophysiological mechanisms of chorea are poorly understood. This condition may be due to dysfunction of a neural network connecting motor cortical areas and a group of subcortical nuclei to the basal ganglia.9 Furthermore, several studies suggest that selective impairment of striatal neurons projecting to the lateral globus pallidus10 disrupts basal ganglia connectivity, which may in turn lead to chorea.11,12
In our case, the lesion mostly affected the insula probably causing partial damage to the indirect pathway connected to the right basal ganglion and nearby areas, leading to hemichorea.
The first step in managing chorea is to identify and resolve the underlying disorder; in clinical practice, however, most choreic syndromes require symptomatic treatment, since no treatments targeting the aetiological factors of chorea are available.7,13
Antidopaminergics constitute the treatment of choice for patients with chorea, regardless of the aetiology. As a general rule, the stronger the blocking effects of the dopamine D2 receptor antagonist (haloperidol), the greater its effectiveness against chorea.7 This may be explained by the fact that dopamine stimulates striatopallidal neurons in the direct pathway and inhibits them in the indirect pathway; in other words, increased dopaminergic activity exacerbates chorea, whereas decreased dopaminergic activity has the opposite effect.12
In our patient, whose CCM was uncomplicated, medical treatment with haloperidol managed symptoms satisfactorily (chorea disappeared after 2 months of treatment).
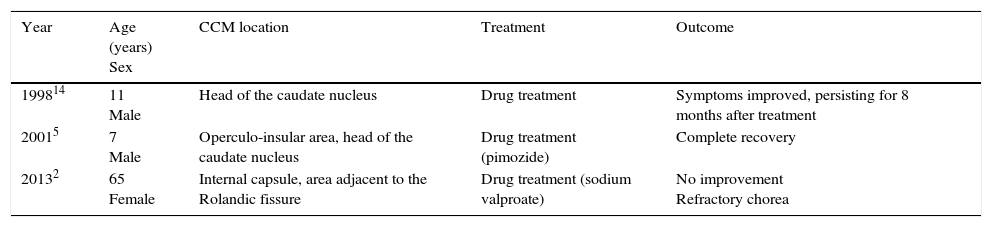
A literature search yielded only 3 case reports of patients with chorea associated with CCMs and treated with medication; ours is the first case of chorea associated with a CCM located in the insula (Table 1).
Characteristics of patients with chorea associated with cerebral cavernous malformations and treated with medication.
| Year | Age (years) Sex | CCM location | Treatment | Outcome |
|---|---|---|---|---|
| 199814 | 11 Male | Head of the caudate nucleus | Drug treatment | Symptoms improved, persisting for 8 months after treatment |
| 20015 | 7 Male | Operculo-insular area, head of the caudate nucleus | Drug treatment (pimozide) | Complete recovery |
| 20132 | 65 Female | Internal capsule, area adjacent to the Rolandic fissure | Drug treatment (sodium valproate) | No improvement Refractory chorea |
CCM: cerebral cavernous malformation.
In conclusion, we present the case of a patient with hemichorea who responded well to haloperidol. Variability in lesion location supports the hypothesis that a functional global network of the basal ganglia is involved in movement control, with disruptions at different points of the network resulting in the same symptoms. In our case, a CCM in the contralateral insula, which damaged peripheral structures of the caudate nucleus, may be involved in the underlying pathogenic mechanisms of chorea.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Espinoza López DA, Serrano Rubio AA, Perdomo Pantoja A. Malformación cavernomatosa cerebral en mujer presentándose con hemicorea: respuesta al haloperidol. Neurología. 2017;32:554–556.