Cardiac arrhythmias are frequent in acute stroke. Stroke units are widely equipped with cardiac monitoring systems. Pre-existing heart diseases and heart–brain interactions may be implicated in causing cardiac arrhythmias in acute stroke. This article analyses cardiac arrhythmias detected in patients hospitalised in a stroke unit.
MethodProspective observational study of consecutive patients admitted to a stroke unit with cardiac monitoring. We collected clinical data from patients and the characteristics of their cardiac arrhythmias over a 1-year period (2013). Time of arrhythmia onset, associated predisposing factors, and the therapeutic decisions made after detection of arrhythmia were examined. All patients underwent continuous cardiac monitoring during no less than 48hours.
ResultsOf a total of 332 patients admitted, significant cardiac arrhythmias occurred in 98 patients (29.5%) during their stay in the stroke unit. Tachyarrhythmia (ventricular tachyarrhythmias, supraventricular tachyarrhythmias, complex ventricular ectopy) was present in 90 patients (27.1%); bradyarrhythmia was present in 13 patients (3.91%). Arrhythmias were independently associated with larger size of brain lesion and older age. In 10% of the patient total, therapeutic actions were taken after detection of significant cardiac arrhythmias. Most events occurred within the first 48hours after stroke unit admission.
ConclusionsSystematic cardiac monitoring in patients with acute stroke is useful for detecting clinically relevant cardiac arrhythmias. Incidence of arrhythmia is higher in the first 48hours after stroke unit admission. Age and lesion size were predicted appearance of arrhythmias. Detection of cardiac arrhythmias in a stroke unit has important implications for treatment.
Las arritmias cardiacas son frecuentes en el ictus agudo. La monitorización cardiaca telemétrica es una técnica extendida en las unidades de ictus. La aparición de arritmias en el ictus agudo puede relacionarse con las interacciones cerebro-corazón o con la patología cardiaca. Se analiza las arritmias relevantes en pacientes ingresados en una unidad de ictus.
MétodoEstudio descriptivo observacional prospectivo de pacientes ingresados en una unidad de ictus con monitorización cardiaca. Se analizan las características de los pacientes y las arritmias registradas durante un año (2013). Se investigó el tiempo de aparición, su asociación con factores predisponentes y las consecuencias terapéuticas de la detección. Todos los pacientes al menos tuvieron 48h de monitorización cardiaca.
ResultadosSe analizó a 332 pacientes, de los cuales 98 (29,5%) presentaron algún tipo de arritmia relevante. Se registraron taquiarritmias (taquiarritmias ventriculares, taquiarritmias supraventriculares, actividad ectópica ventricular compleja) en 90 pacientes (27,1%), y bradiarritmias en 13 pacientes (3,91%). La aparición de arritmias se asoció a un mayor tamaño de la lesión y mayor edad de los pacientes. La detección de arritmias relevantes tuvo consecuencia terapéuticas en el 10% de todos los pacientes. La incidencia de arritmias fue mayor durante las primeras 48h.
ConclusionesLa evaluación sistemática de la monitorización cardiaca en pacientes con ictus agudo permite detectar arritmias cardiacas clínicamente relevantes. Su incidencia es mayor durante las primeras 48h. La edad y el tamaño de la lesión cerebral se relacionan con su aparición. La detección de arritmias en una unidad de ictus tiene consecuencias terapéuticas fundamentales.
Cardiac arrhythmias, a frequent complication during the acute phase of cerebral ischaemia, are associated with increased morbidity and mortality.1–3 Their presence is related not only to a history of heart disease but also to a number of other factors, including autonomic dysfunction secondary to heart–brain interactions.3–7 Cardiac monitoring is a widely used technique in stroke units that enables better management of any cardiac arrhythmias that may arise.8 Although the utility of cardiac monitoring is widely recognised, some aspects of great practical importance, such as time of monitoring, have not yet been fully explained in guidelines for acute ischaemic stroke management.9,10
In light of the above, and with a view to furthering our knowledge of cardiac arrhythmias in stroke units, we have designed a study with the following objectives: to describe the types of cardiac arrhythmias usually detected while monitoring patients in the acute phase of stroke, to identify profiles at a high risk of presenting clinically relevant arrhythmias, and to evaluate the therapeutic consequences of detecting arrhythmias in cardiac monitoring.
Material and methodsPatientsWe conducted a prospective observational descriptive study of patients admitted to the stroke unit at the Complejo Asistencial Universitario de León, in Spain, between 1 January and 31 December 2013. We included all patients admitted to our stroke unit with a diagnosis of ischaemic stroke, transient ischaemic attack, or intraparenchymal haemorrhage. Patients had to meet 2 additional inclusion criteria: being admitted within 48hours of symptom onset and being monitored by telemetry for more than 48hours.
Diagnoses at admission to the stroke unit were based on clinical and radiological findings. We excluded all patients who at discharge received a definitive diagnosis of a condition other than any one of the 3 events indicated in the inclusion criteria.
MethodsAll patients underwent a 12-lead electrocardiogram (ECG) at admission and subsequently received continuous cardiac monitoring. Our unit was equipped with 5 monitoring beds: 4 for 3-lead ECG monitoring and one for 5-lead ECG monitoring. Continuous monitoring was performed using the DASH 3000 (GE); patient monitoring data were displayed on both a bedside patient monitor and a central station monitor (GE CDA19 T). Cardiac monitoring was continuous but in some patients had to be interrupted for short periods while they were transferred to other departments for complementary tests.
Arrhythmias were identified in 2 ways: 1) by reviewing each patient's telemetry monitoring data in the central station on a daily basis with the aim of confirming that arrhythmias had been correctly identified and classified, and 2) by using the automatic arrhythmia detection system, which emits light and sound alarms if an arrhythmia is detected, at both the patient monitor and the central station. The alarm was set to activate for asystole, irregular rhythm, tachycardia (>120bpm), bradycardia (<40bpm), and ventricular arrhythmias. If the alarm went off, a nurse in the stroke unit checked whether the arrhythmia had been recorded correctly and informed the head or on-call neurologist. When necessary, an additional 12-lead ECG was performed to have a more accurate record of arrhythmias. In case of diagnostic or therapeutic uncertainty, we consulted the cardiology department at our hospital. In addition, all patients underwent a complete neurosonology study, tests for blood pressure and blood glucose levels, and in many cases an echocardiogram. To measure lesion size, we compared all the axial slices acquired in neuroimaging studies during hospitalisation and used the one that best showed lesion size in each patient; we used cranial CT images in some cases and brain MR images in other cases.
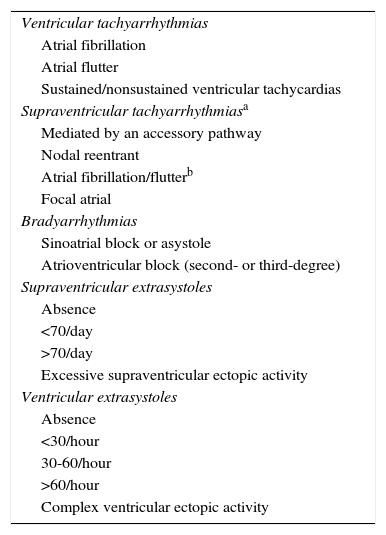
Arrhythmias were considered to be clinically relevant if they caused symptoms or were detected by ECG based on the following classification (Table 1): a) ventricular tachyarrhythmias; b) supraventricular tachyarrhythmias (lasting>30s and at a rate>130 bps, excluding sinus tachycardias); c) bradyarrhythmias (pauses lasting over 3s or a heart rate drop below 30bpm for more than 30s); d) supraventricular extrasystoles (only excessive supraventricular ectopic activity was considered to be clinically relevant and was therefore used for data analysis); and e) ventricular extrasystoles (only complex ventricular ectopic activity was considered clinically relevant and was therefore used for data analysis).
Cardiac arrhythmia classification used in this study.
| Ventricular tachyarrhythmias |
| Atrial fibrillation |
| Atrial flutter |
| Sustained/nonsustained ventricular tachycardias |
| Supraventricular tachyarrhythmiasa |
| Mediated by an accessory pathway |
| Nodal reentrant |
| Atrial fibrillation/flutterb |
| Focal atrial |
| Bradyarrhythmias |
| Sinoatrial block or asystole |
| Atrioventricular block (second- or third-degree) |
| Supraventricular extrasystoles |
| Absence |
| <70/day |
| >70/day |
| Excessive supraventricular ectopic activity |
| Ventricular extrasystoles |
| Absence |
| <30/hour |
| 30-60/hour |
| >60/hour |
| Complex ventricular ectopic activity |
We used the term ‘excessive supraventricular ectopic activity’ based on previous studies and its possible relationship with atrial fibrillation11; it is defined as the presence of either more than 30 supraventricular ectopic complexes per hour or runs of ≥20 supraventricular ectopic complexes. Likewise, the term ‘complex ventricular ectopic activity’ was used for: polymorphic ventricular extrasystoles, R-on-T phenomena, early-coupled ventricular extrasystoles, ventricular premature beats at a rate>300/h, and ventricular bigeminy of >30s. During the analysis, patients with ventricular tachyarrhythmias, supraventricular tachyarrhythmias, and complex ventricular ectopic activity were included in the tachyarrhythmia group. As explained in the caption for Table 1, only patients with de novo atrial fibrillation or atrial flutter were used in the statistical analysis, meaning that we did not include those patients with a history of atrial fibrillation or flutter.
Our study was approved by the Clinical Research Ethics Committee at Complejo Asistencial Universitario de León.
Statistical analysisData were analysed using SPSS statistical software, version 15.0 for Windows. Quantitative variables were expressed as either means±SD or medians (p25, p75) and qualitative variables as absolute and relative frequencies. In the univariate analysis, we used the chi-square test or the Fisher exact test for categorical variables, and the t test or the Kruskal–Wallis test for continuous variables. We conducted a multivariate analysis to determine the factors independently and significantly associated with the dependent variable (developing clinically relevant arrhythmias) using binary logistic regression techniques. Statistical significance was set at P<.05 for all tests.
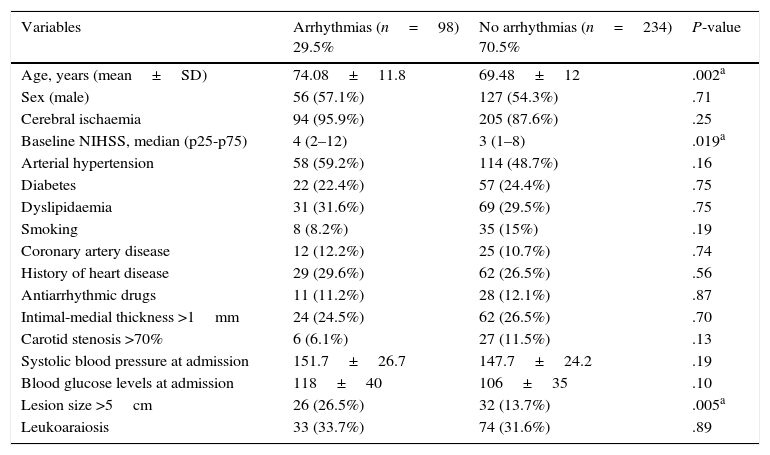
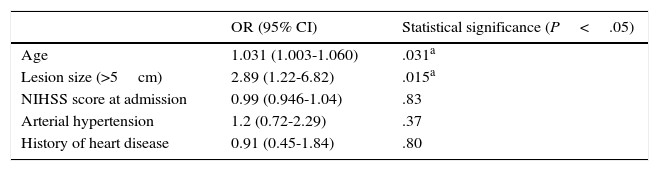
ResultsWe gathered data from 332 patients; arrhythmias were detected in 29.5% of them (n=98). The occurrence of arrhythmias was correlated with several variables: patient clinical data, vascular risk factors, comorbidities, radiological characteristics of the lesion, and a history of heart disease. In the univariate analysis, which included the baseline characteristics of the 2 groups (Table 2), 3 variables were shown to reach statistical significance in the arrhythmia group: age, NIHSS score at admission, and lesion size (either > or <5cm). In the multivariate analysis, however, only 2 variables showed a statistically significant association with developing arrhythmias: age and lesion size (Table 3).
Univariate analysis of the baseline characteristics of the 2 groups.
| Variables | Arrhythmias (n=98) 29.5% | No arrhythmias (n=234) 70.5% | P-value |
|---|---|---|---|
| Age, years (mean±SD) | 74.08±11.8 | 69.48±12 | .002a |
| Sex (male) | 56 (57.1%) | 127 (54.3%) | .71 |
| Cerebral ischaemia | 94 (95.9%) | 205 (87.6%) | .25 |
| Baseline NIHSS, median (p25-p75) | 4 (2–12) | 3 (1–8) | .019a |
| Arterial hypertension | 58 (59.2%) | 114 (48.7%) | .16 |
| Diabetes | 22 (22.4%) | 57 (24.4%) | .75 |
| Dyslipidaemia | 31 (31.6%) | 69 (29.5%) | .75 |
| Smoking | 8 (8.2%) | 35 (15%) | .19 |
| Coronary artery disease | 12 (12.2%) | 25 (10.7%) | .74 |
| History of heart disease | 29 (29.6%) | 62 (26.5%) | .56 |
| Antiarrhythmic drugs | 11 (11.2%) | 28 (12.1%) | .87 |
| Intimal-medial thickness >1mm | 24 (24.5%) | 62 (26.5%) | .70 |
| Carotid stenosis >70% | 6 (6.1%) | 27 (11.5%) | .13 |
| Systolic blood pressure at admission | 151.7±26.7 | 147.7±24.2 | .19 |
| Blood glucose levels at admission | 118±40 | 106±35 | .10 |
| Lesion size >5cm | 26 (26.5%) | 32 (13.7%) | .005a |
| Leukoaraiosis | 33 (33.7%) | 74 (31.6%) | .89 |
Multivariate analysis of occurrence of arrhythmias.
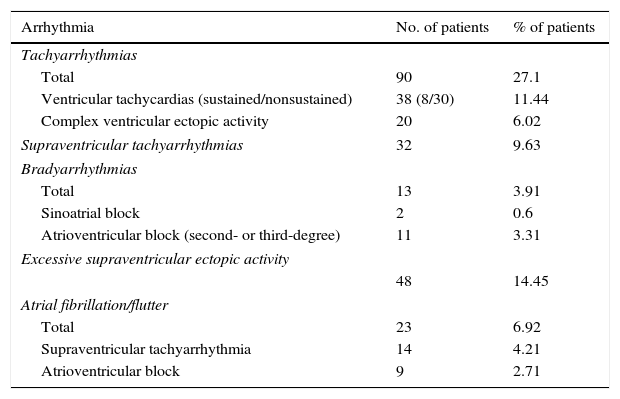
According to the study of all recorded cardiac arrhythmias (Table 4), tachyarrhythmias were much more common than bradyarrhythmias among our patients (27.1% vs 3.91%). We recorded 38 ventricular tachyarrhythmias, 30 of which were due to nonsustained ventricular tachycardias and 8 due to sustained ventricular tachycardias. De novo atrial fibrillation or flutter were detected in 23 patients (6.9% of the total). In 9 of these patients, atrial fibrillation or flutter presented as bradyarrhythmia, that is, in the context of atrioventricular block, whereas in the rest it presented as supraventricular tachyarrhythmia. Excessive supraventricular ectopic activity was detected in 14.4% of the patients.
Recorded cardiac arrhythmias.
| Arrhythmia | No. of patients | % of patients |
|---|---|---|
| Tachyarrhythmias | ||
| Total | 90 | 27.1 |
| Ventricular tachycardias (sustained/nonsustained) | 38 (8/30) | 11.44 |
| Complex ventricular ectopic activity | 20 | 6.02 |
| Supraventricular tachyarrhythmias | 32 | 9.63 |
| Bradyarrhythmias | ||
| Total | 13 | 3.91 |
| Sinoatrial block | 2 | 0.6 |
| Atrioventricular block (second- or third-degree) | 11 | 3.31 |
| Excessive supraventricular ectopic activity | ||
| 48 | 14.45 | |
| Atrial fibrillation/flutter | ||
| Total | 23 | 6.92 |
| Supraventricular tachyarrhythmia | 14 | 4.21 |
| Atrioventricular block | 9 | 2.71 |
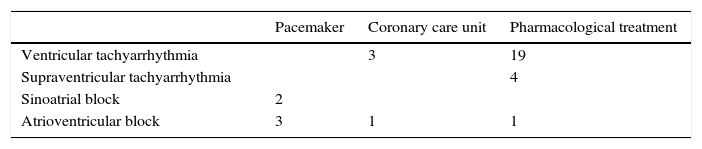
The patients who were treated with anticoagulants upon detection of atrial fibrillation or flutter were excluded from the analysis of treatment decisions following detection of cardiac arrhythmias (Table 5). Around 10% of our patients received some type of cardiology treatment as a consequence of detecting cardiac arrhythmias while monitoring them in the stroke unit. However, if we consider only the patients with arrhythmias, the percentage of patients receiving cardiology treatment reaches 33%. Antiarrhythmic drugs were the most frequent treatment option, although some patients were transferred to the coronary care unit or underwent a permanent pacemaker implantation. None of the patients with arrhythmias required emergency electrical cardioversion.
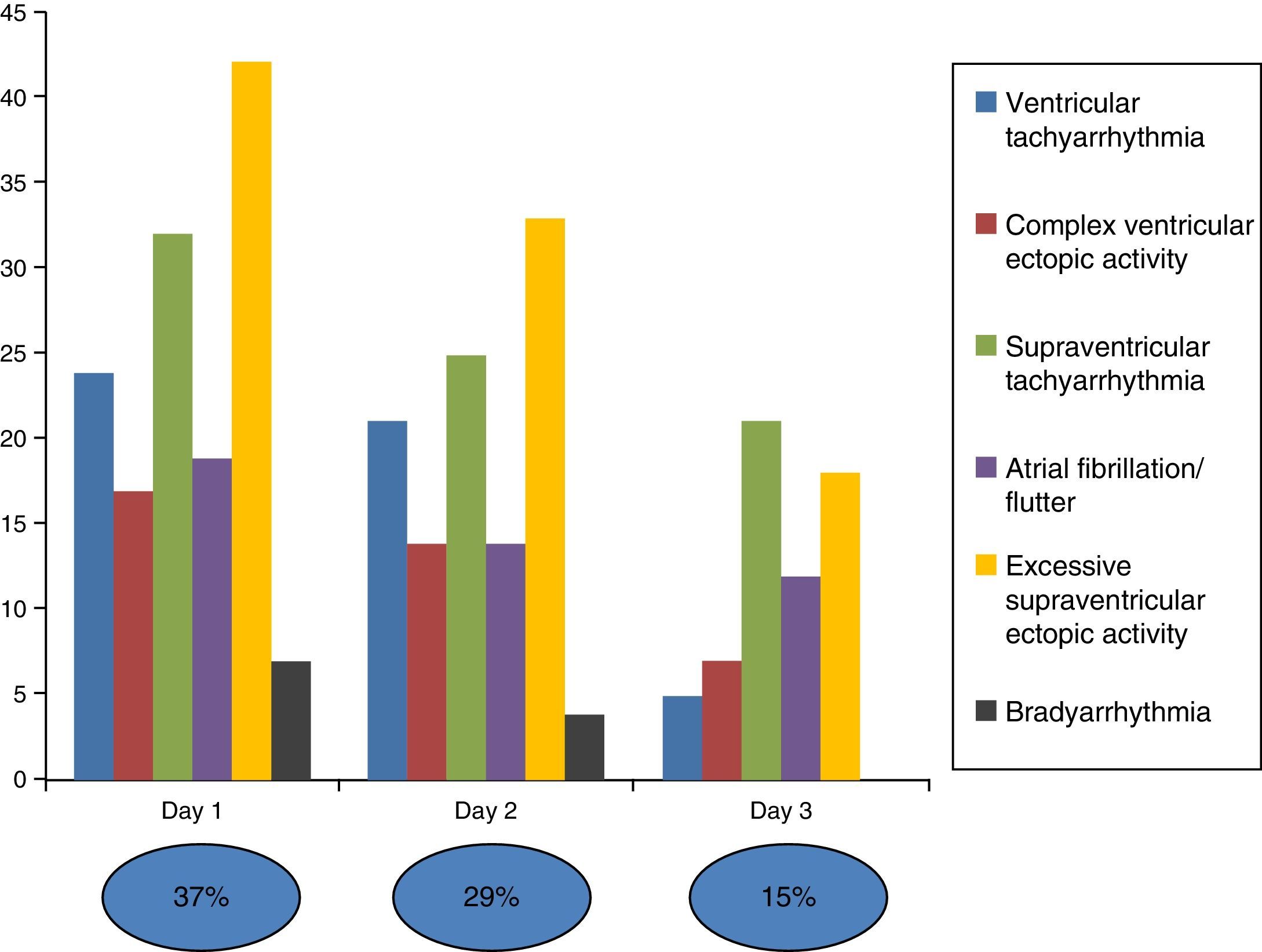
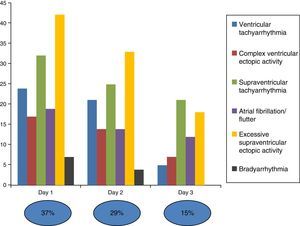
Fig. 1 analyses the percentage of occurrence of arrhythmias by time of monitoring: most of the arrhythmias were recorded within the first 48hours, and the percentage begins to decrease by the third day in both absolute and relative terms.
DiscussionCardiac arrhythmias, specifically atrial fibrillation, are an important aetiological factor for ischaemic stroke.12 However, investigating the aetiology of ischaemic stroke is not the only reason for cardiac monitoring in stroke units: cardiac arrhythmias are frequent complications during the acute phase of cerebrovascular events (whether ischaemic or haemorrhagic) and may even lead to sudden death.
In our study, we recorded cardiac arrhythmias in 332 patients admitted to the stroke unit and analysed their incidence, temporal profile, correlation with other predictive variables, and the therapeutic consequences of detecting arrhythmias.
Our results show that systematically reviewing cardiac monitoring output in patients with acute stroke helps detect clinically relevant cardiac arrhythmias. More specifically, 29.5% of our patients presented some type of clinically relevant arrhythmias, meaning that roughly 1 in 3 patients required medical assessment of ECG findings.
Regarding patient subgroups at a higher risk of clinically relevant arrhythmias, these complications were observed to be more frequent in older patients and in those with greater lesion sizes. Both variables have already been associated with the occurrence of arrhythmias in previous, similar studies.13–15 These 2 variables are involved in heart–brain interactions. Age may be considered a risk factor associated with the occurrence of clinically relevant arrhythmias based on the high prevalence of heart disease and cardiovascular risk factors in the elderly.16,17 In our study, however, the independent variables of history of heart disease and history of other diseases (arterial hypertension, diabetes, dyslipidaemia, etc.) showed no statistically significant association with the occurrence of arrhythmias. Autonomic cardiovascular dysfunction is common after stroke, which explains why brain lesions may be regarded as a cause of cardiac arrhythmias.3–7 According to our study, lesion size is associated with the occurrence of cardiac arrhythmias regardless of the aetiology of the lesion (ischaemic or haemorrhagic). Although we did not analyse lesion location as a factor in the occurrence of arrhythmias, this factor is likely to play a relevant role.18 Clinical severity of brain lesions, assessed using the NIHSS, showed a statistically significant association with the occurrence of arrhythmias in the univariate analysis. In the multivariate analysis, however, this association was found to be statistically non-significant. The NIHSS reflects neurological deficits in the acute phase of stroke, which do not necessarily correspond to the area of brain parenchyma that is eventually damaged. This means that heart–brain interactions may be more related to lesion location than to the clinical expression of stroke in the acute phase.
Analysing the temporal profile of clinically relevant arrhythmias is interesting given the practical importance of establishing the duration of cardiac monitoring in stroke units. According to previous studies, serious cardiac adverse events peak within the first 2-3 days after stroke.19 In our study, all the patients were monitored for at least 48hours. Our results show a greater incidence of arrhythmias within the first 48hours; from that point, incidence dropped. Therefore, and in light of these findings, cardiac monitoring should last a minimum of 48hours, and even longer in high-risk patients.19
Lastly, one of the purposes of the present study was to evaluate the therapeutic consequences of detecting cardiac arrhythmias in the study population. In 33% of the patients with cardiac arrhythmias (10% of the total sample), detection of arrhythmias had important implications for treatment. Although pharmacological treatment was the most frequent therapeutic option, some patients required more straightforward measures, including transfer to the coronary care unit and permanent pacemaker implantation. We hypothesise that, in a significant percentage of our patients, cardiac monitoring may have been key to receiving optimal cardiology treatment, which may in turn have improved quality of life and short- and long-term survival.
A number of factors must be considered before comparing our results with those of other similar studies. Some of these were conducted decades ago,1,2,20–22 which means there are major methodological differences between these and our study. Some of the results of other more recent studies13–15 coincide with our own, as in the case of the association between age or lesion size and the risk of presenting arrhythmias. However, they differ in some points. For example, the incidence of atrial fibrillation or flutter is considerably lower in our study, probably because we only included de novo episodes. Data on extrasystoles were also dissimilar, as we included only excessive supraventricular ectopic activity and complex ventricular ectopic activity in the statistical analysis. Likewise, the high incidence of ventricular tachycardias in our study is also noteworthy: we hypothesise that methodically analysing telemetry results of each patient on a daily basis may have played a crucial role in our results. A high percentage of nonsustained ventricular tachycardias lasted for a very short time and, as a result, the alarm of the monitoring device did not go off. This underscores the importance of the staff at the stroke unit reviewing telemetry results every day.
Our study has a number of limitations. First, it is an observational study conducted at a single centre, and the patients included in our study were those admitted to our stroke unit. As a result, patients with clinically severe impairment requiring mechanical ventilation, or with subarachnoid haemorrhage, were not included in the study population. However, the prevalence of cardiac arrhythmias in these patients is known to be high.14,23,24 Likewise, all patients were monitored for a minimum of 48hours, but monitoring times varied between patients based on individualised clinical criteria that may have biased the results. In any case, we feel our results are relevant in that they lead to a better knowledge of a subject of great practical importance which has received little attention.
FundingThis study has received no funding of any kind.
Conflicts of interestThe authors have no conflicts of interest to declare.
We wish to thank all the doctors, nurses, and nursing assistants working at the neurology department of Complejo Asistencial Universitario de León. This study would not have been possible without their hard work and dedication.
Please cite this article as: Fernández-Menéndez S, García-Santiago R, Vega-Primo A, González Nafría N, Lara-Lezama LB, Redondo-Robles L, et al. Arritmias cardiacas en la unidad de ictus: análisis de los datos de la monitorización cardiaca. Neurología. 2016;31:289–295.
Preliminary results from this study have been presented at the 65th Annual Meeting of the Spanish Society of Neurology and the 23rd European Stroke Conference.