An increased risk of stroke has been reported in patients under 60 who have received radiation therapy (RT) for head and neck neoplasms, due to the fact that irradiation of these regions causes accelerated atherosclerosis, enhanced by the coexistence of vascular risk factors. The onset of cerebral ischemia symptoms usually occurs 10 years after radiation therapy,1 although the exact course of post-RT arteriopathy and the most adequate treatment have not been properly established.
We report the case of a young stroke patient in relation to a major, progressive post-RT arteriopathy of extracranial cerebral arteries.
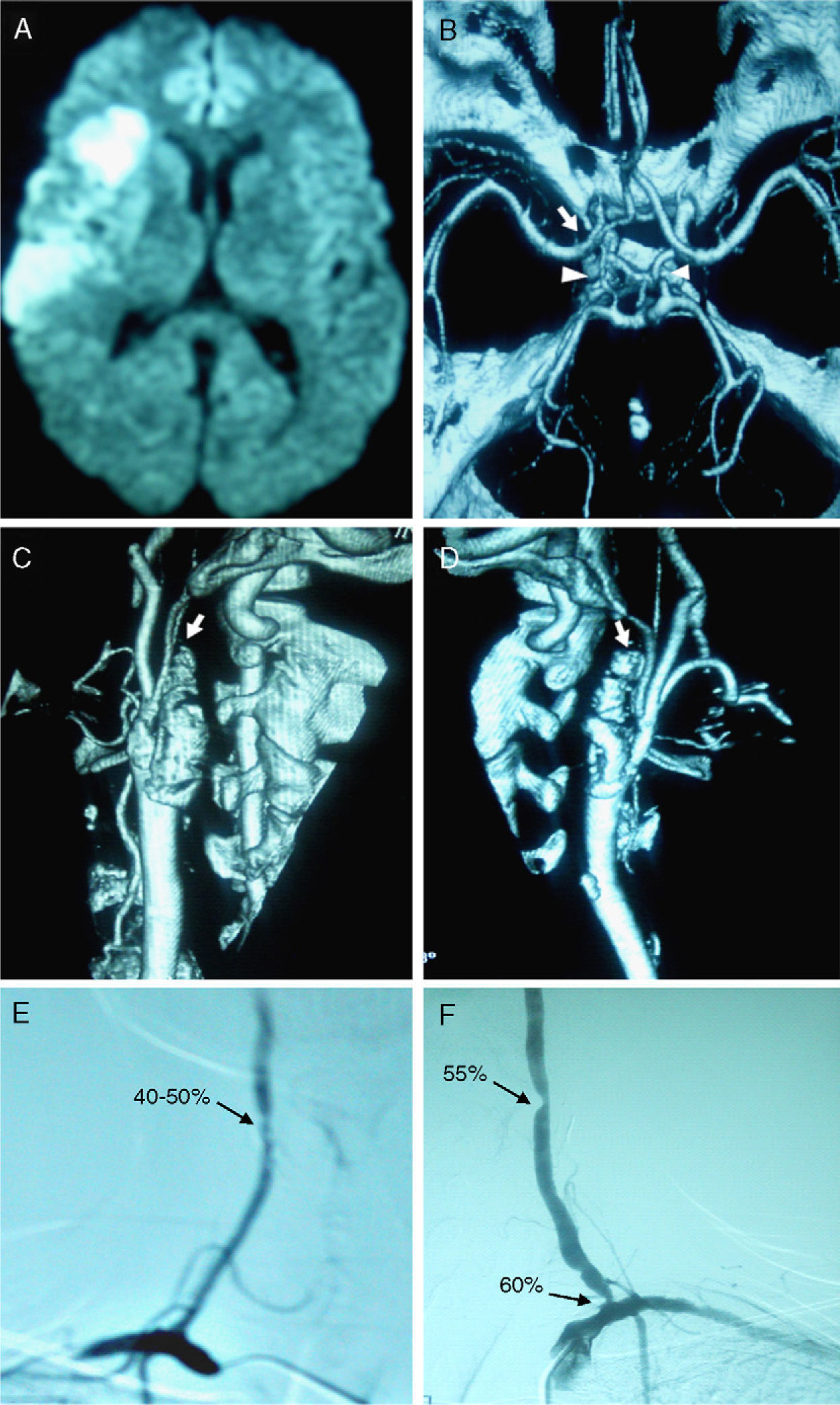
The patient was a 45-year-old male, a heavy ex-smoker with a history of nasopharyngeal carcinoma treated with RT at age 25. The total dose of RT received by the patient was 70Gray (Gy), at a rate of 2Gy daily. The irradiated area encompassed the nasopharynx (area of primary tumour) and lymph node chains (cervical region). He came to the emergency service due to a loss of strength in the left side of the body and dysarthria upon awakening. In the previous 2 days, he had presented self-limited episodes of neurological symptoms consisting of tongue paresthesia and a feeling of dizziness. We performed cranial CT scans, an electroencephalogram, chest radiography and laboratory studies, which all resulted normal. The patient was admitted at a stroke unit, where an MRI revealed an acute ischemic lesion in the right fronto-temporal region (Fig. 1A). The transcranial Doppler (TCD) showed a very significant acceleration of the right middle cerebral artery (R-MCA) and a moderate acceleration of the left anterior cerebral artery (L-ACA); slight acceleration of the left carotid siphon; and mild-moderate acceleration of both vertebral arteries (VA) and basilar artery. We calculated the cerebral haemodynamic reserve of the patient using the apnoea test with TCD, obtaining a decreased Breath Holding Index in the anterior region (0.54 in R-MCA and 0.51 in L-MCA), but with values considered normal in the posterior region (1.01 in R-PCA and 1.29 in L-PCA). The duplex of extracranial cerebral arteries showed an occlusion of both internal carotid arteries (ICA). CT-angiography of the circle of Willis found good filling of vessels, with tortuous but permeable posterior communicating arteries, retrograde filling of the right carotid siphon and almost no filling of the left siphon (Fig. 1B). CT-angiography of the extracranial cerebral arteries confirmed the occlusion of both ICA (Fig. 1C and D) with good quality, permeable VA. After 1 year of monitoring, the patient began to present pre-syncopal episodes in the context of low blood pressure (BP) levels (approximately 100/60mmHg). We performed a new duplex of the extracranial cerebral arteries, which revealed the maintenance of ICA occlusion, but which also showed an acceleration of VA, both at the medium level and at the origin. An arteriography confirmed 60% stenosis at the origin of the left VA and 55% in the distal extracranial region of the vessel, associated with 40–50% stenosis of the right VA, also extracranial. The arteries of the circle of Willis presented no alterations, showing collateral circulation at the expense of the posterior communicating arteries (Fig. 1E and F). A second brain MRI found no new ischemic lesions. We opted for conservative management with measures to increase BP, such as increasing salt content in the diet, and observed a favourable evolution. At present we are conducting close clinical monitoring of the patient.
(A) Diffusion MRI scan showing an acute ischemic lesion in the region of the right middle cerebral artery. (B) CT-angiography scan of the circle of Willis showing good filling of intracranial vessels, with tortuous but permeable posterior communicating arteries (arrowhead), as well as retrograde filling of the right carotid siphon and almost no filling of the left siphon (arrow). (C and D) CT-angiography scan of extracranial cerebral arteries showing occlusion of the right (C) and left (D) internal carotid arteries (arrows). (E) Arteriography of the vertebral arteries showing a 40–50% stenosis in the distal third of the right vertebral artery. (F) Image showing 60% stenosis at the origin of the left vertebral artery, as well as 55% stenosis in its distal cervical track.
Post-RT arteriopathy usually affects the ICA, with percutaneous transluminal angioplasty with stent placement being indicated in the case of symptomatic stenosis.2,3 However, there is no scientific evidence of the most effective therapeutic approach in the case of VA stenosis after RT, as there are only a few reported cases, with variable evolution.
To date, the most accepted treatment for symptomatic VA stenosis due to RT, which often affects the origin and the subclavian artery, has been surgical repair of both arteries.4 The literature only contains 1 case of angioplasty with stent in the case of VA stenosis after RT, in which dissection of the artery occurred as a complication of the procedure, leading to surgical repair treatment.5
This case presented peculiarities making it unique. There was extensive and severe arteriopathy of the main extracranial arteries, with occlusion of both ICA and stenosis of the VA. In addition to cerebral stroke in the anterior region, the patient started with pre-syncopal episodes, associated with progressive stenosis of the VA. The therapeutic challenge was great. On the one hand, only the low BP levels could be the cause of the symptoms, so their elevation was the immediate option chosen. However, the progressive VA stenosis required us to monitor the patient closely, since the need for endovascular or surgical treatment to restore blood flow could appear at any given time. Surgical treatment presented the most complications in this type of arteriopathy,2 but angioplasty with stent also carried the risk of arterial rupture. This would have been a dramatic event in this patient, since his cerebral vascular substitution was limited to just the 2 vertebral arteries.
Large multicentre studies are required to determine the most appropriate treatment in severe, progressive arteriopathy post-RT. These should also establish the most appropriate therapeutic action, especially in the case of concomitant involvement of the ICA and VA.
Please cite this article as: Prefasi D, et al. Oclusión carotídea bilateral y estenosis progresiva de arterias vertebrales posradioterapia en paciente joven. Neurología. 2011;27:122–4.