We present the case of a male aged 74 years suffering from long-term rheumatoid arthritis with no pharmacological treatment. He visited the emergency department due to sudden loss of strength in both right limbs. In the preceding few months he had experienced asthenia and weight loss due to hyporexia. Physical examination revealed significant joint deformities, mild right hemiparesis with hyperreflexia and right-sided Babinski reflex.
His symptoms led us to frame the following differential diagnosis: cerebrovascular disease, intracranial infection or inflammation, neoplasia, or toxic-metabolic disorders.
As cerebrovascular disease was the first suspected diagnosis, doctors ordered a blood test (including haemogram, biochemical, coagulation, immunology, tumour markers, and serology studies), an electrocardiogram, a chest radiography, a transcranial vertebrobasilar Doppler ultrasound, carotid duplex scan, and an emergency brain CT. Results from the electrocardiogram, transcranial Doppler and carotid duplex scan were normal. Brain CT showed left subcortical frontoparietal cerebral oedema with leptomeningeal impairment.
Complementary test results did not permit us to rule out the aetiologies contemplated in the initial evaluation (neoplasia, intracranial infection or inflammation). We therefore decided to admit the patient and complete an extended diagnostic study.
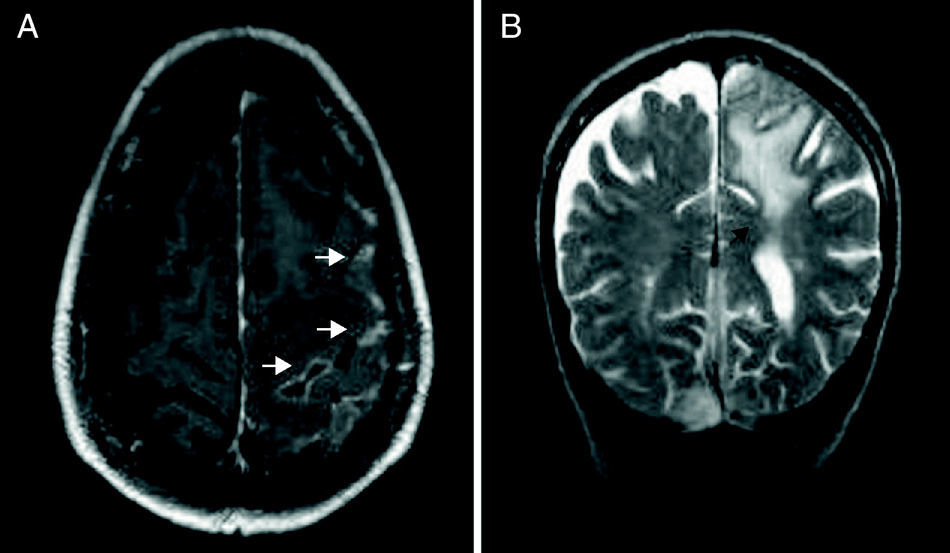
Laboratory analyses revealed an increase in acute-phase reactants (fibrinogen 531mg/dL, ESR 62, CRP 105.78mg/dL), high titres of rheumatoid factor (RF 2770), and elevated serum immunoglobulins (IgG 602, IgM 230). Tumour markers were normal and serological tests for HBV, HCV, CMV, and HIV were negative. Lumbar puncture revealed intrathecal synthesis of IgM with biochemical analyses, cytology, and CSF culture all being normal. Brain MRI was indicative of leptomeningeal impairment (Fig. 1) with a predominantly left posterior and parietal subcortical oedema (Fig. 1B) suggesting meningoencephalitis. There were no signs on the PET-CT suggesting viable tumour tissue at any level.
The most likely aetiology based on these findings is autoimmune focal encephalitis related to the patient's underlying disease. Doctors suggested performing a brain biopsy, but the patient and his family refused the procedure. Doctors therefore began treatment with prednisone (1mg/kg/day). At 15 days after the onset of intravenous corticosteroid treatment, the patient presented no neurological symptoms. He was then started on immunosuppressants to specifically treat his disorder.
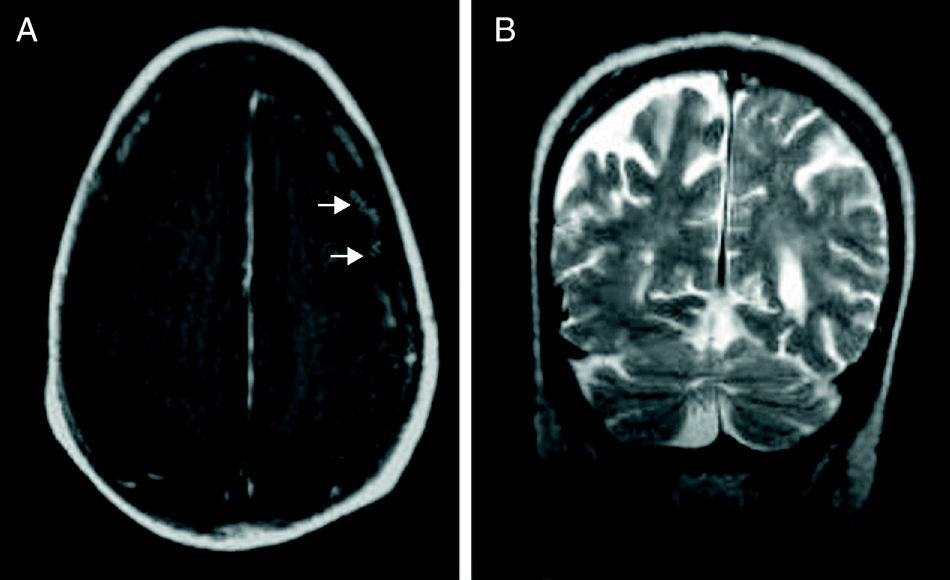
A routine brain MRI performed 5 months later showed a decreased level of leptomeningeal impairment (Fig. 2A) and no subcortical oedema.
In view of the patient's medical history, complementary test results, and his clinical and radiological improvement after steroid and immunosuppressant treatment, he was diagnosed with autoimmune focal leptomeningeal encephalitis due to rheumatoid arthritis.
As mentioned above, the most frequent neurological manifestations of rheumatoid arthritis, including sensory nerve entrapment, occur in the peripheral nervous system. Effects of rheumatoid arthritis on the central nervous system may include meningeal nodules, pachymeningitis, and cerebral vasculitis.
Meningeal nodules are usually asymptomatic and typically do not invade brain parenchyma.
Rheumatoid pachymeningitis is a rare complication that may appear in late stages of the disease. It is caused by the diffuse infiltration of inflammatory cells and may present with epileptic seizures or cranial nerve compression.2
Central nervous system vasculitis is a rare extra-articular manifestation which usually appears in advanced stages of the disease. In some cases, however, it presents as the first symptom. In cerebral vasculitis, tissue damage may arise as a result of occlusion of the inflamed blood vessels or due to a direct autoimmune mechanism.1,3 Few cases of rheumatoid meningoencephalitis due to vasculitis have been described, but all of them report an underlying autoimmune pathogenic mechanism. Such cases are generally treated with high doses of intravenous corticosteroids, and the treatment is usually effective.4–6
Due to the aggressive manifestations of rheumatoid meningoencephalitis, patients with a suspected diagnosis should begin treatment with high doses of intravenous steroids so as to reduce subsequent sequelae.
Please cite this article as: Rodríguez Sanz A, et al. Meningoencefalitis focal de causa autoinmune. Neurología. 2013;28:63–4.