Askin tumour is a rare and highly malignant neoplasm.1,2 Clivus metastasis is infrequent in these patients. To our knowledge, this is the first reported case of Askin tumour with clivus metastasis.
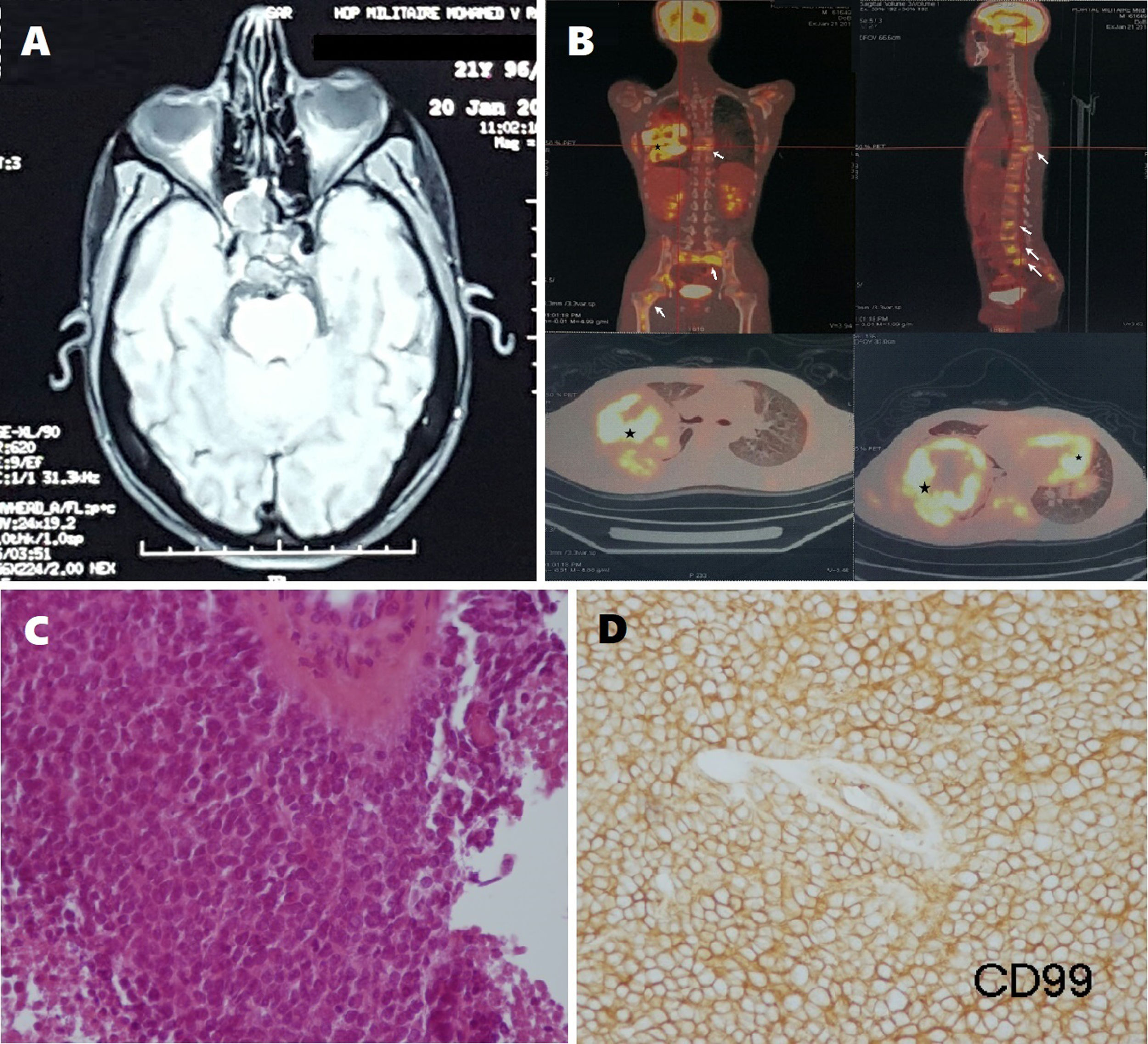
Our patient is a 21-year-old man with no relevant medical history, who visited the ophthalmology department due to 7-month history of diplopia, without decreased visual acuity or eye pain. The neurological examination revealed oculomotor palsy of the ipsilateral third, fourth, and sixth cranial nerves, associated with impairment of sensory branches V1 and V2. Brain MRI revealed a tumour in the clivus that extended laterally to the right cavernous sinus, compressing both temporal lobes; the posterior part occupied the sphenoid sinus and the anterior part infiltrated the posterior wall of the cavum (Fig. 1A).
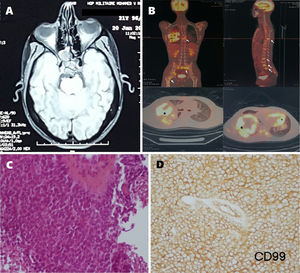
A) Axial T1-weighted brain MRI scan showing a tumour in the clivus. B) 18F-FDG PET study revealing a hypermetabolic mass in the right lung, with nodules in the left lower lobe (stars) and diffuse bone metastases (arrows). C) Round cell tumour proliferation. The histological study revealed cells with ill-defined cytoplasm and hyperchromatic nuclei (although most cells were non-nucleated), and abnormal mitosis. D) The immunohistochemical study revealed positivity for anti-CD99 antibodies.
Laboratory analysis showed a lactate dehydrogenase level of 1000 IU/L, a C-reactive protein level of 115 mg/L, and an erythrocyte sedimentation rate of 83 mm/h.
A full-body CT scan performed to locate the primary tumour revealed a mass in the right lung, with areas of necrosis in the middle and lower lobes. 18F-FDG PET revealed a hypermetabolic mass in the right lung, nodules in the left lower lobe, and several bone lesions affecting the humeral heads, scapulae, sternum, rib cage, thoracic and lumbar vertebral column, pelvis, and femurs (Fig. 1B).
The histological study of a specimen collected with a CT-guided lung biopsy showed compact cell walls separated by large areas of necrosis, sometimes presenting vessels with thickened walls surrounded by small elements with scarce, ill-defined cytoplasm. These cells were rarely nucleated, with rounded or oval-shaped hyperchromatic nuclei (Fig. 1C). The immunohistochemical study revealed positivity for anti-CD99 antibodies (Fig. 1D). The patient tested negative for anti-cytokeratin AE1/AE3, anti-P40, and anti-neurofilament antibodies. These morphological and immunohistochemical characteristics are compatible with primitive neuroectodermal tumour.
The patient received 2 cycles of chemotherapy with vincristine, doxorubicin, cyclophosphamide, etoposide, and ifosfamide. The third cycle could not be administered due to worsening clinical status. He died 15 days later.
Askin tumour is encompassed within the family of Ewing sarcoma tumours. It has an incidence of 2.9 cases per million children and adolescents, and rarely affects adults older than 30 years.1,2 It was first described in 1979 as a malignant small-cell tumour of the thoracopulmonary region.3 Askin tumours present similar histological characteristics to primitive neuroectodermal tumours, and a unique clinicopathological profile (onset at young ages, location in the chest, and poor prognosis).2
By order of frequency, the most common sites of metastasis include the contralateral lung, lymph nodes, and bones; metastases are rarely observed in the liver, adrenal glands, brain, retroperitoneal space, or sympathetic nervous system.2 Cases have been reported of Askin tumour metastasis to the spinal cord and the retro-orbital, retrocrural, and oropharyngeal spaces.2 To our knowledge, this is the first reported case of Askin tumour metastasis to the clivus.
In a literature review of clivus metastases, we identified a total of 66 patients, of whom 27% were women and 73% were men. Mean age was 59 years. The most common locations for primary tumours were the prostate (21%), kidney (11%), liver (9%), stomach (9%), lung (8%), and thyroid gland (6%).
Twenty-three patients presented symptoms associated with clivus metastasis prior to diagnosis of the primary tumour. Most patients presented sixth nerve palsy (43%) or diplopia (29%). Radiological study of the skull base frequently includes brain CT, MRI, and PET scans. Dekker et al.4 report a mean survival time of 11 months; survival times decrease to a mean of 5 months for patients with clivus metastasis associated with cranial nerve palsy.5
Askin tumours are frequently associated with short survival times. Factors of poor prognosis include presence of metastasis at the time of diagnosis, large tumour size, presence of pleural effusion, and poor response to neoadjuvant chemotherapy.7 The ideal treatment for Askin tumours is a combination of neoadjuvant chemotherapy, radical surgical resection, and adjuvant radiochemotherapy.6,7 However, metastases are frequently detected at the time of diagnosis, hindering optimal treatment.
In conclusion, this report describes a rare case of Askin tumour with clivus metastasis. Clinical and radiological signs suggestive of clivus metastasis should prompt suspicion of this type of tumour; these symptoms enable early diagnosis.
We would like to thank Ahmed Zahir Lakhal for his participation in the French to Spanish translation of this study.
Please cite this article as: Zegmout A, Asri H, Rhorfi I, Abid A. Tumor de Askin con metástasis en clivus: una localización infrecuente. Neurología. 2021;36:633–634.