Ischaemic stroke is the leading cause of death in women and the third in men in our setting.1,2 On occasion, diagnosis is hindered by the presence of atypical signs and symptoms, which may confuse the neurologist or clinician attending the patient for the first time.
We present the case of a patient with ischaemic stroke with atypical hallucinations as the sole manifestation.
Our patient is a 95-year-old woman who lives alone and is totally independent in the activities of daily living and does not present cognitive impairment; her medical history only reports hypercholesterolaemia, controlled with low doses of statins.
She consulted due to a one-month history of sudden-onset visual hallucinations limited to the left hemifield. She saw “people with tiny hands,” distorted images, “[her] relatives’ heads became huge when they approached [her] from the left”; she also saw animals approaching her from the left. The patient was aware at all times that these were hallucinations but found them highly disturbing. The examination also revealed left homonymous hemianopsia, with no further neurological deficits.
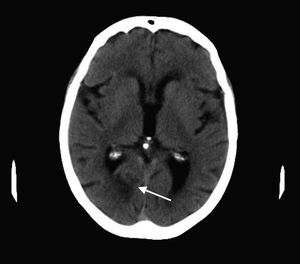
A brain CT scan showed a hypodensity in the right posterior cerebral artery (PCA) territory, affecting the calcarine sulcus (Fig. 1).
Aetiological studies included a Doppler ultrasound of the supra-aortic trunks, which obtained normal results; a transcranial duplex ultrasound, which showed a normal circle of Willis; Holter monitoring, which ruled out emboligenic arrhythmia; and a blood test, with normal results. An electroencephalography revealed slow activity in the right posterior area (coinciding with the area of the ischaemic lesion).
The patient was diagnosed with cryptogenic ischaemic stroke in the right PCA area, manifesting as Alice in Wonderland syndrome (AWS); treatment was started with low doses of levetiracetam in addition to antiplatelets for secondary prevention of vascular events; this achieved good outcomes.
AWS was first described in 1955 by the British psychiatrist John Todd3 and included a group of symptoms “intimately associated with migraine and epilepsy, although not confined to these disorders”. It owes its name to the similarity of symptoms with Lewis Carroll's story, in which Alice experiences changes in body size. As described in the book Alice's Adventures in Wonderland,4 the group of symptoms includes visual illusions which make the patient perceive alterations in the dimensions of objects (micropsia and macropsia), repeated images of stimuli after their disappearance (palinopsia), altered shapes (metamorphopsia), or animals (zoopsia).
This syndrome is occasionally accompanied by depersonalisation and altered perception of time. The most remarkable feature of this syndrome is that patients are aware that they are experiencing hallucinations.5
Symptoms of AWS are attributed to functional and structural abnormalities in the visual perception system in the occipital lobe6; the most frequent causes include space-occupying lesions, migraine episodes, seizures, or hallucinogenic substances.
In some series, cerebrovascular aetiology accounts for 3% of AWS cases, predominantly in patients older than 18.7
Most cases are benign, but if there is an underlying cause (as in our patient), symptomatic treatment may be necessary and useful, with antiepileptics being the most frequently used drugs.8
Our patient's progression with low doses of antiepileptics was optimal.
Please cite this article as: García-Cabo C, Fernández-Domínguez J, García-Rodríguez R, Mateos Marcos V. Síndrome de Alicia en el País de las Maravillas como primera y única manifestación de un ictus isquémico. Neurología. 2019;34:487–488.