The purpose of our study is to describe 4 cases of sexsomnia, a form of parasomnia characterised by sexual behaviour during sleep.
MethodsClinical history and video-polysomnography recordings from patients diagnosed with sexsomnia in the Multidisciplinary Sleep Unit at Hospital Clínic in Barcelona.
ResultsThree men and one woman between 28 and 43 years of age reported sexual behaviours during sleep with progression times ranging from 9 months to 7 years. Episodes consisted of masturbation without seeking the participation of a sleeping partner (2 cases) and attempts at sexual intercourse with inappropriate and uncharacteristic vocalisations and behaviours (3 cases). The frequency of the episodes ranged from 4 isolated episodes to 2-3 per week. Patients were amnestic of these events and surprised by their partners’ accounts of their behaviour. Medical histories revealed that 1 patient was a somnambulist, 2 had confusional arousals, and 1 experienced somniloquy. Video-polysomnography did not disclose sexual behaviours during sleep but revealed sleep apnoea in 2 cases and periodic leg movements in sleep in another. The only patient treated with clonazepam reported decreased frequency of both confusional arousals and sexsomnia episodes.
ConclusionsSexsomnia occurs in young adults and is characterised by masturbation and inappropriate attempts at achieving sexual intercourse followed by total amnesia of the events. It can be associated with other parasomnias such as sleepwalking and confusional arousals. Other sleep disorders, including sleep apnoea and periodic leg movement disorder, may trigger episodes of sexsomnia.
El objetivo de nuestro trabajo es describir 4 casos de sexsomnia, una parasomnia caracterizada por conductas sexuales durante el sueño.
MétodoHistoria clínica y registro videopolisomnográfico de pacientes identificados en la unidad multidisciplinaria del sueño del Hospital Clínic de Barcelona.
ResultadosTres varones y una mujer entre 28 y 43 años de edad referían conductas sexuales durante el sueño de entre 9 meses y 7 años de evolución. Consistían en la masturbación sin buscar la participación de la pareja, que dormía en la misma cama (2 casos), e intentar el coito con vigorosidad conductual y verbal inapropiada e inhabitual (3 casos). La frecuencia era variable entre 4 únicos episodios y 2-3 semanales. Los pacientes presentaban amnesia completa de los eventos y sorpresa cuando se les explicaba lo que habían hecho. Había antecedentes de sonambulismo (un caso), despertares confusos (2 casos) y somniloquia (un caso). Los registros polisomnográficos con vídeo no detectaron conductas sexuales pero registraron apneas (2 casos) y movimientos periódicos de las piernas (un caso). En el único paciente en que se probó clonacepam la frecuencia de la sexsomnia y los despertares confusos disminuyó.
ConclusiónLa sexsomnia aparece en el adulto joven, consiste en intentar consumar de forma inapropiada el coito o masturbarse durante el sueño, con amnesia posterior de lo ocurrido. Puede coexistir con otras parasomnias, como sonambulismo y despertares confusos. Otros trastornos del sueño, como las apneas y los movimientos periódicos de las piernas, podrían desencadenar los episodios de sexsomnia.
Parasomnias are abnormal sensory or motor phenomena that occur during sleep, while falling asleep, and upon waking.1 The International Classification of Sleep Disorders groups parasomnias as REM sleep parasomnias (REM sleep behaviour disorder, nightmares, and sleep paralysis), non-REM sleep parasomnias (sleepwalking, confusional arousals, and night terrors), and a third group of ‘other parasomnias’ that includes, for example, enuresis, sleep-related eating disorder, and sleep-related groaning.1
Recent studies have described sexsomnia or sleep sex, a new parasomnia in which specific motor activation produces inappropriate and involuntary sexual behaviour.2–7 After falling asleep, patients with sexsomnia engage or attempt to engage in sexual intercourse or sexual behaviour in inappropriate and inhabitual ways. They are not conscious of this behaviour and cannot recall what happened the next day. Behaviour may include masturbation, attempting sexual activity with a partner sleeping in the same bed, or even attempting sex with a non-partner with whom the patient does not share a bed or a room. Sexsomnia may lead to marital repercussions, or even legal repercussions in very serious cases or those involving minor children.2,3 Prevalence of the syndrome is unknown since it is rare and probably underdiagnosed due to patients’ and doctors’ lack of awareness and reluctance to describe it.7 Medical literature on sexsomnia is very scarce. Fewer than 50 cases had been described prior to October 2012,2–6 and clinical symptoms may be mistaken for those of other entities such as epilepsy. Here, we present 4 cases studied in our sleep disorders unit that may contribute to our understanding of this parasomnia.
Patients, methods, and resultsThe 4 cases we describe below were identified in the multidisciplinary sleep disorders unit in Hospital Clínic, Barcelona, between November 2007 and March 2012. None of these 4 patients had a history of psychiatric or sexual disorders. In these 4 cases, researchers completed a detailed medical history and a nocturnal polysomnography with synchronised audio-visual recording.
Case 1The first case was a 38-year-old man, accompanied by his wife, who consulted due to a 7-year history of abnormal behaviour during sleep. He had no family or personal history of relevant medical or surgical episodes except for nasal septoplasty performed 5 years earlier. The patient had no history of traumatic sexual experiences. He reported isolated incidents of sleep talking as a child. The patient presented no other abnormal sleep behaviours, such as confusional arousal, sleepwalking, night terrors, or other types of parasomnia.
He had been in a stable relationship for 17 years and the couple had a daughter. They engaged in conventional and satisfactory sexual intercourse with a frequency of 2-3 times weekly. The patient's wife reported that in the past 7 years, her husband would sleep for 2-3hours at night before presenting abrupt 10- to 30-minute episodes in which he would attempt to achieve coitus. He experienced such an episode approximately once a week. In contrast to his behaviour when awake, he used vigorous movements and lewd language while attempting to persuade and penetrate his partner. During one episode, he immobilised her by placing his arm around her neck like a yoke. The patient's wife reported that the patient's penis was erect during every episode. Although he attempted penetration, she never permitted it because she believed that the episodes were not normal sexual behaviour and that her husband's actions were involuntary. The patient had awakened in a confused state during some of these episodes and was surprised by his wife's account of his behaviour. The patient and his partner were unable to link these episodes to any trigger factors such as stress or prior sexual stimuli. He never recalled what had happened the following morning. Likewise, he could not recall having dreamed on the nights on which this behaviour occurred. The patient did not typically remember his dreams, but he did occasionally experience erotic dreams accompanied by spontaneous ejaculation (‘wet dream’). However, these dreams never coincided with the episodes he described in the consultation.
In addition to episodes of sexsomnia, he had a 20-year history of snoring, apnoeic episodes observed by his wife, and excessive daytime drowsiness while eating, reading, driving, and helping his daughter with her homework. Due to the possibility of obstructive sleep apnoea he had undergone nasal septoplasty 5 years before, without having had a prior polysomnography. This procedure did not improve snoring or drowsiness or modify his sexual behaviour during sleep. The patient presented an Epworth Sleepiness Scale score of 14 and a body mass index of 25.
Our hospital performed a daytime EEG, which yielded normal results, as well as nocturnal polysomnography with synchronised audio-visual recording. The latter was indicative of obstructive apnoea episodes associated with oxyhaemoglobin desaturation and micro-arousals causing broken sleep. The global apnoea/hypopnoea index for obstructive episodes was 13/hour, reaching 40/hour when the patient was supine. The study detected no other abnormalities, such as epileptiform activity or abnormal sleep behaviours such as those described during episodes of sexsomnia or other types of parasomnia. The patient refused treatment for sleep apnoea as well as clonazepam treatment for sexsomnia.
Case 2Case 2 was a 41-year-old woman who made an appointment due to a 1-year history of atypical sexual behaviour. She had presented childhood sleepwalking until the age of 14. The patient had a 1-year history of metrorrhagia of unknown origin which caused iron deficiency anaemia; she was periodically treated with oral iron supplements. The patient had no relevant sexual history.
Her husband explained that in the past year, she had been masturbating about 3 times per week without seeking to involve him although they slept in the same bed. She did not remember these episodes upon waking up the next morning. They occurred around 5.00 and sometimes resulted in orgasm, to the surprise of her husband, who never participated in his wife's episodes. When her husband described these episodes, she felt ashamed and stated that she was unable to remember them. She reported that they had regular, satisfactory, and pleasant sexual intercourse, with no sexual problems when awake.
In addition, her husband also indicated that she displayed repetitive and periodic non-sexual limb movements while sleeping, especially when in the lateral decubitus position. The patient explained that when she was awake she occasionally presented a sensation of restless legs when resting, especially at night, which did not interfere with her ability to fall asleep when she went to bed. She did not snore and no apnoeic episodes were detected during sleep. Likewise, she presented no excessive daytime drowsiness or insomnia.
A polysomnography study with audio-visual recording identified periodic leg movements during sleep. The study showed an index of 24 movements per hour, occurring throughout the night. An index of 7 periodic leg movements per hour was associated with microarousals resulting in partially broken sleep. Apart from affecting the patient's feet, the characteristic feature of these movements was their association with sudden abduction of the lower limbs. On 2 occasions, these movements were more prolonged, accompanied by repetitive arm movements. She also placed her hand on her genitals for a few seconds but did not masturbate. No apnoeic episodes, epileptiform activity or other abnormalities were recorded during sleep.
She began treatment with 0.18mg pramipexole administered at bedtime and oral iron therapy, which improved restless legs syndrome. However, her atypical sexual behaviour remained unchanged 90 days after treatment onset and the patient stopped attending follow-up visits.
Case 3The third case was a 43-year-old man examined due to abnormal behaviour during sleep. Since childhood, he presented frequent episodes of nocturnal talking and shouting. These episodes were occasionally associated with distressing nightmares (impossible tasks, fights with animals, failure to comply with family responsibilities, etc.). In the preceding year, he had been working rotating shifts (morning, afternoon, and night). The patient presented no sexual disorders and practices satisfactory conventional sexual intercourse.
He has been living with his partner for a year. The partner relates that the patient, 2hours after falling asleep, occasionally sits up abruptly and shows signs of confusion and fear. He may also be able to have a partially coherent conversation with her for a few minutes. During these episodes, his eyes are always open; he is able to move and may swat at the air. His partner believes him to be asleep at these times and the patient never recalls the episodes in the morning.
His partner also reported 4 similar episodes involving exclusively sexual behaviour. During each episode, the patient, after sleeping 2-4hours, attempted to initiate sex with his partner by touching her body and genitals. His partner rejected these advances due to finding them inappropriate and probably involuntary; each time, the patient showed no aggression or insistence, but merely moved to the other side of the bed, expressing his frustration and annoyance in such terms as ‘no fun’. Upon being informed of the episode the next morning, the patient was unable to remember it. These 4 sexual episodes were described as not posing problems for the couple and they always occurred on a day when the patient changed shifts. The patient also explained that similar sexual behaviour had also manifested with a former partner, who had on occasions permitted his advances resulting in both parties achieving orgasm. These episodes had been described to him by the previous partner; the patient only had a vague recall of the end of the sex act.
A nocturnal polysomnography study with audio-visual recording was performed during 2 nights without detecting any abnormal behaviour. Both recordings did show snoring and obstructive sleep apnoea. The apnoea–hypopnoea index during sleep was 16/hour and 7/hour on both nights. Apnoeic episodes were more common when the patient was supine, especially during REM sleep; the episode index was recorded at 37/hour and 40/hour for this sleep phase and the supine posture. No periodic leg movements, epileptiform activity, or other abnormalities were recorded during sleep. The polysomnogram showed muscle atony in REM phase, which was sufficient to rule out REM sleep behaviour disorder. The patient refused treatment for sexsomnia and sleep apnoea.
Case 4Case 4 was a 28-year-old man who made an appointment due to abnormal behaviour during sleep. Medical history revealed use of anodyne, with no history of drug abuse and no current medications. Regarding family history, he reported that his brother had experienced probable sleepwalking as a child: “he would get up at night and go to the balcony to urinate”.
His partner, with whom he had been living for 9 months, reported that between 3 and 6 nights per week, while the couple was sleeping, the patient would abruptly sit up in bed or turn towards her and shake her before uttering incoherent fragments like “look at that house” or “the devil”. According to his partner, they were even able to hold conversations. On some occasions, the patient would cry out or laugh. He also displayed abnormal movements and gestures that appeared to mime driving, holding a conversation, or searching for something in the bed. In doing so, he seemed to be acting out a dream. During these episodes, the patient's eyes remain open and he appears restless and worried. His partner is generally able to soothe him by telling him to go back to sleep. The patient has never managed to get out of bed during an episode.
The partner also reported that the patient suffers episodes that are similar, but exclusively sexual, some 2 or 3 times a month. During these episodes, the patient begins to masturbate or turns to his partner and touches her in an attempt to initiate sex. His partner reported that the patient is neither aggressive nor violent during these times, but states “it isn’t him”, describing the behaviour as more lewd and vulgar. During the episodes, the patient's penis is erect. His partner consistently refuses sex at these times, and the patient obediently stops the behaviour without insisting or complaining. His partner believes that if she allowed it, he would be able to engage in coitus.
All his episodes of abnormal sleeping behaviour, whether sexual or non-sexual, tend to occur only once per night, between 3.00 and 4.00, when the patient has been asleep for 2-3hours. The patient does not recall any abnormal behaviour, although he feels more tired on the days after an episode is reported. Likewise, the patient reports no nightmares or erotic dreams. The couple engage in regular sex during waking hours, and both consider it satisfactory.
As a child, the patient presented episodes of sleep talking and sleepwalking. In the past, the patient's former partners with whom he did not cohabitate had also mentioned occasions on which he talked in his sleep or displayed unusual behaviour, including sexual behaviour, resembling that described by his current partner.
A nocturnal polysomnography study with audio-visual recording did not register abnormal conduct. No apnoeic episodes, periodic leg movements, epileptiform activity, or other abnormalities were recorded during sleep. Following diagnosis of non-REM sleep parasomnia with confusional arousals and sexsomnia, we recommended improving sleeping habits (regular cycles and 8hours of sleep per night) and clonazepam 0.5mg before bed. Due to better sleeping habits and clonazepam, the patient's confusional arousal frequency dropped to 1 or 2 nights per week, and sexsomnia frequency decreased to 1 or 2 episodes every 3 months.
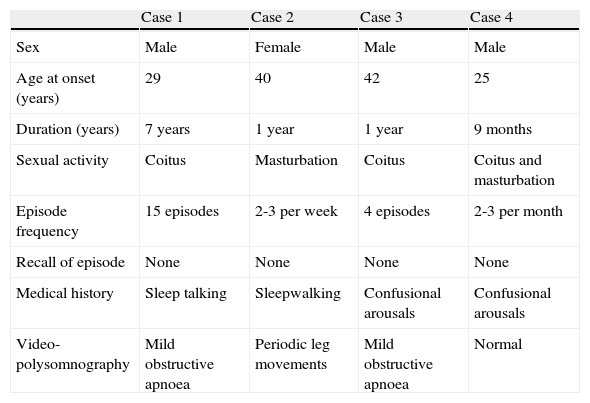
DiscussionIn 2005, the International Classification of Sleep Disorders defined and classified sexsomnia as a variant of the confusional arousals typical of non-REM sleep parasomnia.1 The clinical spectrum of sexsomnia is illustrated by the 4 cases we described here; a summary is also included below (Table 1).
Clinical characteristics and polysomnography findings.
| Case 1 | Case 2 | Case 3 | Case 4 | |
| Sex | Male | Female | Male | Male |
| Age at onset (years) | 29 | 40 | 42 | 25 |
| Duration (years) | 7 years | 1 year | 1 year | 9 months |
| Sexual activity | Coitus | Masturbation | Coitus | Coitus and masturbation |
| Episode frequency | 15 episodes | 2-3 per week | 4 episodes | 2-3 per month |
| Recall of episode | None | None | None | None |
| Medical history | Sleep talking | Sleepwalking | Confusional arousals | Confusional arousals |
| Video-polysomnography | Mild obstructive apnoea | Periodic leg movements | Mild obstructive apnoea | Normal |
- 1.
Predominant in males (3 men, 1 woman).
- 2.
Affects younger adults (patients’ ages at time of examination ranged from 28 to 43 years).
- 3.
History of isolated sleep talking (1 case) or non-REM sleep parasomnia (3 cases).
- 4.
No history of neurological diseases such as epilepsy.
- 5.
No psychiatric disorders and no history of sex-related diagnoses such as paraphilias. While our patients did not complete specific psychiatric or neuropsychological evaluations, our clinical opinion is that no such disorders were present.
- 6.
Sexual activity with intention to complete coitus (in all 3 men) or masturbate (the woman and one of the men).
- 7.
Inappropriate or atypical attitude to sex compared to waking sexual behaviour, characterised by lewdness and vulgarity, or more rarely, forcefulness or aggressiveness.
- 8.
Variable frequency (from 4 single episodes to 2-3 episodes weekly).
- 9.
Not associated with dreams.
- 10.
Total amnesia of the episodes.
- 11.
Polysomnography recordings do not typically detect episodes of sexsomnia, but they may identify other sleep disorders, including apnoea or periodic leg movements.
- 12.
Sexsomnia episodes may possibly be triggered by circumstances leading to broken sleep, such as apnoea (cases 1 and 3), periodic leg movements (case 2), or changes in the sleep-wake cycle (changing shifts in case 3). It is possible that treating these trigger factors may decrease the frequency and intensity of sexsomnia episodes. Two of our patients refused apnoea treatment. The patient with periodic leg movements (case 2) underwent short-term treatment with low doses of pramipexole, with no beneficial effects on sexsomnia. Research suggests that masturbation may be a strategy for treating restless legs syndrome8 and that it may also be a complication of pramipexole treatment.9 However, the patient in case 2 only engaged in masturbation when ‘asleep’, and sexsomnia symptoms began a year before she started treatment with pramipexole.
- 13.
Research shows that treatment with clonazepam may reduce the frequency of sexual behaviours during sleep.2 In the only patient in our series to accept treatment, clonazepam did decrease the frequency of sexsomnia and confusional arousals.
- 14.
Sexsomnia had not led to any significant marital or legal repercussions in these 4 cases.
As of October 2012, fewer than 50 cases of sexsomnia had been described in the literature.2–7 Most (80%) of the published cases are of men; average age at initial consultation is between 30 and 32 years, with about a 10-year history of symptoms. Average age at onset in women is 14 years, compared to 27 years in men. All patients experienced total amnesia of the episodes, which were described by the people who witnessed them masturbating or with whom they attempted intercourse. Sexsomnia is not associated with erotic dreams; this being the case, the subject does not seem to be acting out a dream, as we see in other types of parasomnia such as sleepwalking, confusional arousal, and REM sleep behaviour disorder. Masturbation and sexual vocalisations are the most typical sexsomnia behaviours in women, whereas men more commonly touch and fondle a bed partner's breasts and genitals or attempt to complete coitus. The latency between sexual arousal and sexual readiness is short; patients easily achieve erection or vaginal lubrication. Sexual interests during sexsomnia episodes do not reflect the patient's waking preferences. Cases of homosexual sexsomnia have been described in subjects who are heterosexual when awake; there are also cases of fathers touching the genitals of their daughters or daughters’ friends. Sexual behaviour during sexsomnia episodes also differs from waking behaviour. Some patients are more gentle and affectionate with their partners, whereas others are more direct and abrupt, or even aggressive and violent. They may strike or insult their partners or even attempt sex acts not contemplated in their normal practice, such as anal penetration. A few partners prefer the patient's sexual approach during sexsomnia episodes to the waking approach; the patient may be either more gentle or more direct than normal. However, most partners refuse to engage in sex play and coitus after realising that the patient's actions are not voluntary. In other cases, sexsomnia episodes have erroneously been considered rape due to being interpreted as non-consensual sex acts committed by a person in an alert and conscious state.2–6
Sexsomnia episodes are especially common during the first half of the night. Frequencies vary between patients, ranging from one-time occurrences to several episodes weekly. Trigger factors tend to be physical contact with the bed partner, sleep deprivation, periods of stress, fatigue, and abuse of such substances as alcohol and marijuana on the night of the episode. Sleep masturbation may be violent; the literature includes a case of vaginal tearing and a fractured digit. Typically, the bed partner is surprised upon waking up to find the patient masturbating and uttering moans and sexual vocalisations. Such vocalisations may present as moaning, provocative remarks intended to initiate sex, lewd and sexual remarks, or sexual insults. Sex play includes attempts at removing the partner's clothes, touching his or her genitals, and initiating fellatio or cunnilingus. Sexsomniacs may attempt vaginal, or more rarely anal, penetration; if coitus is completed, it may or may not be followed by ejaculation or orgasm. Various postures are possible if permitted by the patient's partner.2–6
Sexsomnia is often associated with a history of isolated sleepwalking and sleep talking incidents. It has also been described in 4 patients with REM sleep behaviour disorder. Patients with waking sexsomnia have a normal sex life with no history of sexual abuse, sexual trauma, paraphilia, or psychiatric alterations. Some cases have been associated with obstructive sleep apnoea syndrome and the use of zolpidem and selective serotonin reuptake inhibitor antidepressants.2,3
Sexsomnias must be distinguished from other involuntary sexual behaviours, which include wet dreams (a normal phenomenon consisting of spontaneous ejaculation during sleep, typically associated with erotic dreams) and pathological conditions such as painful erections. It must also be differentiated from the hypersexuality occurring in Kleine-Levin syndrome and cases of epileptic seizures with sexual behaviour.2
Very few episodes of sexsomnia have been described using polysomnography with audio-visual recording. Three patients were heard to utter sexual moans during deep N3 stage sleep.10 One patient with sexsomnia completed coitus with his partner (who provoked him sexually while they were sleeping together in the laboratory). He was between wakefulness and light N1 stage sleep, and was unable to recall the episode later.11 A video-polysomnography study of a 60-year-old woman revealed a masturbation episode lasting a few minutes and beginning in deep N3-stage sleep. During the episode, the EEG trace showed a mixture of alpha activity and persistent delta waves indicating deep N3 sleep. When the technicians roused the patient, she could not recall touching herself or having been dreaming.2
As with all other types of non-REM sleep parasomnia, the pathophysiology of sexsomnia is unknown, but it is likely related to disordered sleep-wake regulation mechanisms. We should also mention another type of parasomnia, sleep eating, in which motor activity consists of consuming foods in unusual ways instead of presenting as the sexual behaviour seen in sexsomnia.12
The potential consequences of sexsomnia are quite predictable. Patients are surprised and ashamed by their sexual behaviours, which they may consider anomalous and humiliating. They are unable to recall the behaviour, which is therefore involuntary. This is also a topic for legal medicine since several patients with sexsomnia have been tried for child molestation and rape.
Clonazepam is effective for reducing sexsomnia episode frequency and intensity in most patients.2 Antidepressants may be of use,6 although there is a published case in which citalopram caused sexsomnia episodes.13 The patient should achieve uninterrupted sleep with no arousals or microarousals. Shift changes, apnoea, and periodic leg movements may fragment sleep, and this can lead to episodes of sexsomnia in predisposed individuals.2 On this basis, fostering good sleeping habits and treating apnoea and periodic limb movements may reduce the frequency of sexsomnia episodes.
In summary, sexsomnia is a type of parasomnia that manifests in young adults and consists of masturbation or inappropriate attempts at coitus in a sleeping patient who cannot recall the event. It is important that the entity be recognised so that patients and their partners will receive the appropriate information on their doctor's visit; sexsomnia is potentially treatable, it may present with other parasomnias, and it can result in marital and legal problems in extreme cases.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Ariño H, Iranzo A, Gaig C, Santamaria J. Sexsomnia. Una forma de parasomnia con conductas sexuales durante el sueño. Neurología. 2014;29:146–152.
This study was presented as a poster in the sleep disorders section at the 2011 SEN Annual Meeting.