Oral anticoagulant therapy (ACO) is considered an independent predictor of mortality in patients with intracerebral haemorrhage (ICH), with the role of the international normalised ratio (INR) being unclear. The aim of this work is to evaluate the relationship between ACO and the INR value and the ICH volume, and to determine the relationship between both variables and mortality.
Patients and methodsPatients were retrospectively analysed using the Private Community Cerebrovascular Hospital Register (Registro Cerebrovascular del Hospital Privado de Comunidad), between December 2003 and May 2009. Volumes of the haematomas (dependent variable) were calculated from the first image performed, using the abc/2 method. Independent variables were age, gender, vascular risk factors, site of bleeding, intraventricular dump, clinical severity (Glasgow scale), time to image, antiplatelet drugs, and INR value on admission. An analysis of the relationship between all these variables and mortality was also performed.
ResultsA total of 327 patients with HIC were identified (35 with ACO). Median volume was higher in the anticoagulated patients (55ml vs 24ml P<.05), with no statistically significant relationship between volume and the other variables. In the multivariate analysis, a statistically significant higher mortality associated to volume was observed, but not with anticoagulation.
ConclusionsOral anticoagulation was associated with a higher initial volume of the haematoma, with no correlation between the INR value and volume. The HIC volume was directly related to mortality, however, like the volume, the INR was not associated with increased mortality.
El uso de anticoagulantes orales (ACO) es considerado predictor independiente de mortalidad en pacientes con hemorragias intracerebrales (HIC), siendo incierto el rol del cociente normalizado internacional (INR). El objetivo de este trabajo es evaluar la asociación entre la ACO y el valor del INR, y el volumen de los HIC, así como determinar la relación entre ambas variables y la mortalidad.
Pacientes y métodosSe analizaron retrospectivamente todos los pacientes con HIC incluidos en el registro cerebrovascular del Hospital Privado de Comunidad, entre diciembre de 2003 y mayo de 2009 inclusive. Los volúmenes de los hematomas (variable dependiente) se calcularon sobre la primera imagen realizada, utilizando el método abc/2. Las variables independientes fueron edad, sexo, factores de riesgo vascular, localización del sangrado, volcado intraventricular, gravedad clínica (escala de Glasgow), tiempo para la realización de la imagen, antiagregación y valor del RIN al ingreso. También se analizó la relación entre todas las variables mencionadas y la mortalidad.
ResultadosSe identificó a 327 pacientes con HIC (35 recibían ACO). Fue mayor la mediana de volumen de los anticoagulados (55ml vs 24ml p<0,05), no encontrándose asociación estadísticamente significativa entre el volumen y las demás variables. En el análisis multivariable se observó mayor mortalidad estadísticamente significativa asociada al volumen, no así a la anticoagulación.
ConclusionesLa ACO se asoció a un mayor volumen inicial del hematoma, no encontrándose correlación entre el valor de INR y dicho volumen. El volumen de la HIC se relacionó directamente a la mortalidad; sin embargo, a igualdad de volumen el valor de INR no se asoció a mayor mortalidad.
The use of oral anticoagulants (OAC) before an intracerebral haemorrhage (ICH) is an independent predictor of mortality.1–3 In turn, anticoagulation not only increases ICH risk, but also its severity when it occurs.3,4 During the past few decades, the number of anticoagulation-associated ICH (OAC-ICH) has increased, representing 20% of the total ICH.1–7
Among the factors that influence ICH prognosis, haematoma volume at the time of consultation and extension of the haematoma after its presentation are important variables that could be influenced by the use of anticoagulants.8,9
The international normalised ratio (INR) is a standard measurement to estimate the oral anticoagulant level, although its role as a prognostic factor is uncertain, with differing results in the series published. If there is a relationship between anticoagulation intensity and the clinical outcome of ICH, we must implement strategies to quickly revert the anticoagulant effect. Likewise, strict control of anti-coagulated patients is important, so as to maintain them within proper anticoagulation levels.3,6,8,10
The goal of this study was to assess the association between OAC and INR values and ICH volume, as well as to determine the relationship between both variables and mortality.
Material and methodsAll patients with an ICH diagnosis were consecutively included in the Private Community Cerebrovascular Hospital Register, between December 2003 and May 2009. Any ICH secondary to trauma, tumour, haemorrhagic transformation of infarction, ruptured aneurysm or vascular malformation was excluded. All patients were assessed by on-call neurologists in the emergency department and were admitted to the neurological care unit. All anti-coagulated patients had their treatment stopped immediately and were then treated intravenously immediately with 10mg of vitamin K and frozen fresh plasma according to their INR values and patient weight.
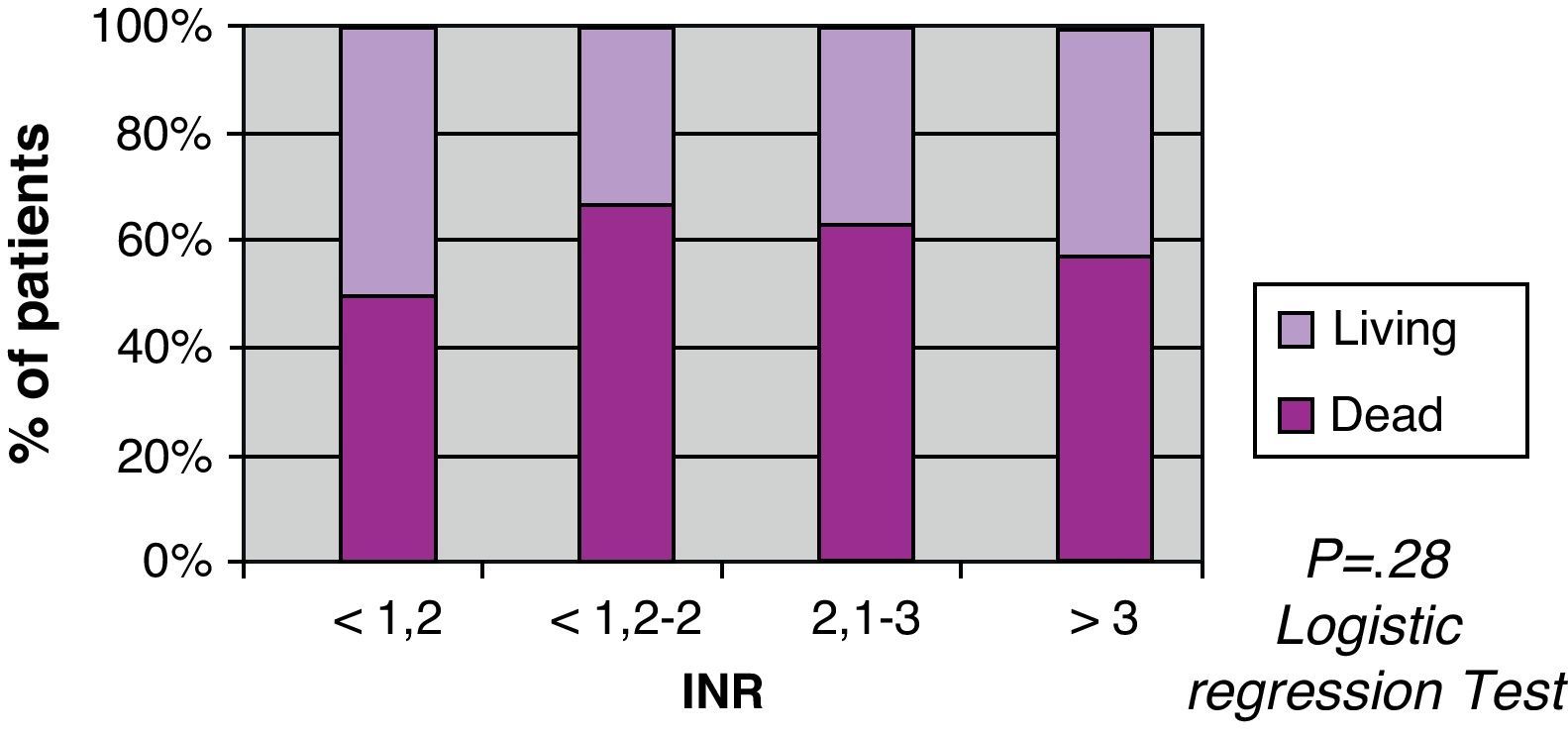
Haematoma volumes (dependent variable) were calculated with the first image taken after the event, by using the abc/2 method.11 The independent variables were age, gender, vascular risk factors (hypertension, diabetes mellitus, dyslipidemia, smoking), site of bleeding (supratentorial), intraventricular dump, clinical severity (measured using the Glasgow scale), time to image, antiplatelet drugs and INR value on admission. They were arbitrarily classified according to INR<1.2, between 1.2 and 2, between 2.1 and 3, and INR>3. All the variables had been defined previously in the Private Community Cerebrovascular Hospital Register manual (www.hpc.org.ar).
The outcome analysed was mortality at day 30 after the ICH in patients, with or without anticoagulation. For patients where there was no outcome information in the register, we obtained this at later consultations, through the internal hospital mortality register or through direct contact with the patients or their relatives.
Statistical analysisA significance level of α=0.05 was established for the statistical analysis. The Mann–Whitney test was used to analyse the relationship between the different independent variables and volume, which did not present a normal distribution. The Spearman correlation coefficient was used to assess the association between the INR variable and haemorrhage volume. The relationship between mortality and the haematoma volume was analysed with the Mann–Whitney test and its relationship with anticoagulation, antiplatelets and supratentorial location were tested using the Chi squared test. Statistically significant variables in the univariate analysis were included in the logistic regression test. The statistical programme used was SPSS version 11.0.
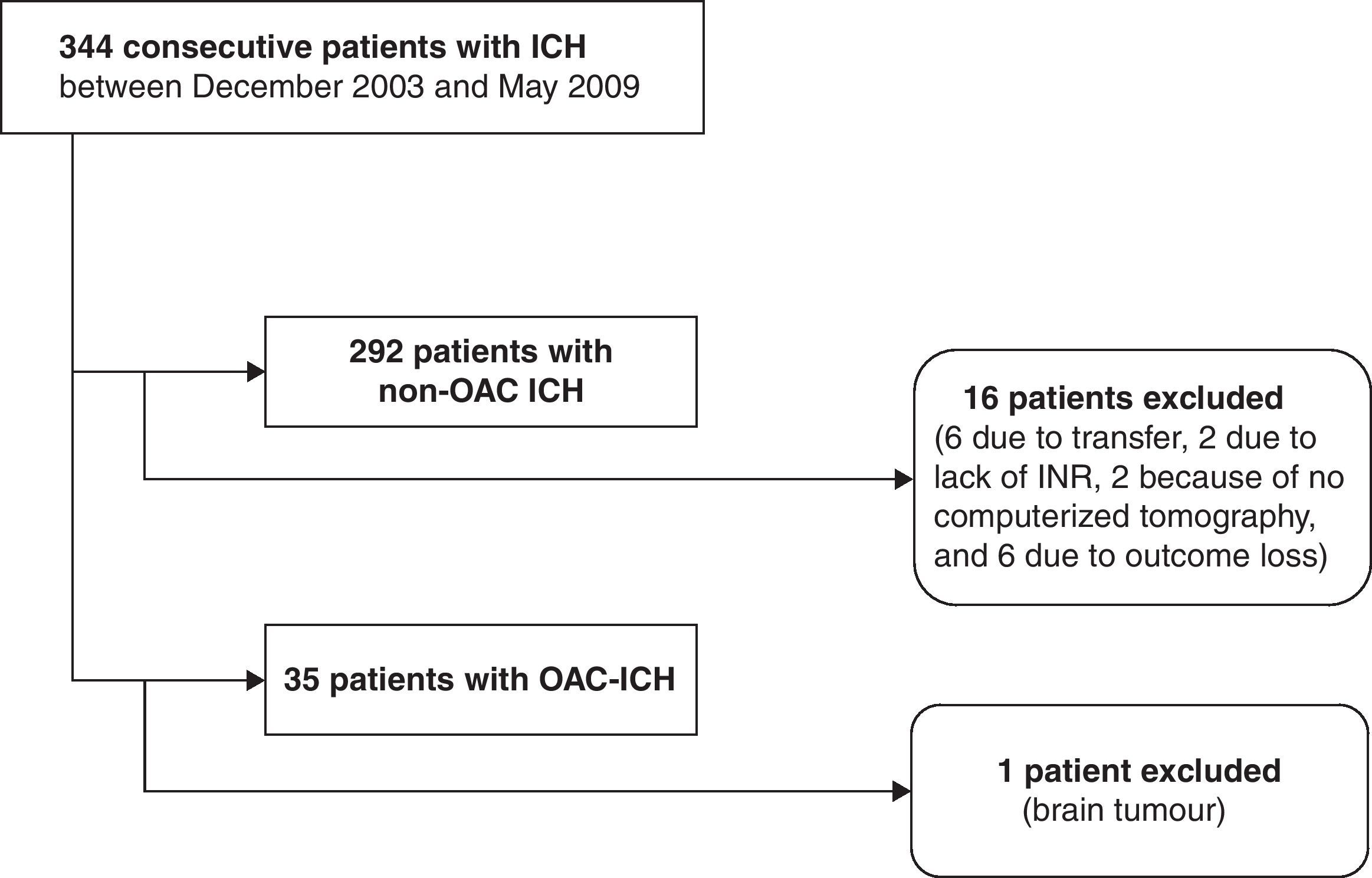
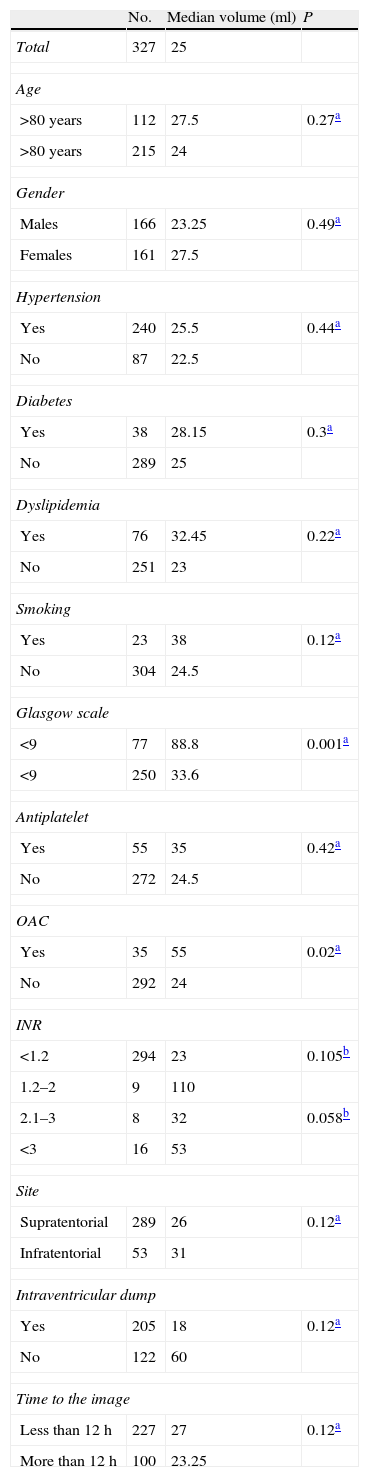
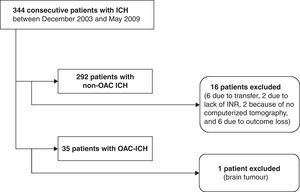
ResultsThere were 344 patients diagnosed with ICH that were identified. We excluded 16 patients from the non-OAC ICH group (6 due to transfer, 2 through lack of INR on admission, because there was no computerised tomography, and 6 due to outcome loss); in the OAC-ICH group, one was excluded due to a suspected secondary haemorrhage from a tumour. There were a total of 292 patients with ICH and 35 with OAC-ICH included in the analyses (Fig. 1). The distribution of patients according to the variables analysed is shown in Table 1.
Distribution of patients according to the variables assessed and their relationship with ICH volume.
| No. | Median volume (ml) | P | |
| Total | 327 | 25 | |
| Age | |||
| >80 years | 112 | 27.5 | 0.27a |
| >80 years | 215 | 24 | |
| Gender | |||
| Males | 166 | 23.25 | 0.49a |
| Females | 161 | 27.5 | |
| Hypertension | |||
| Yes | 240 | 25.5 | 0.44a |
| No | 87 | 22.5 | |
| Diabetes | |||
| Yes | 38 | 28.15 | 0.3a |
| No | 289 | 25 | |
| Dyslipidemia | |||
| Yes | 76 | 32.45 | 0.22a |
| No | 251 | 23 | |
| Smoking | |||
| Yes | 23 | 38 | 0.12a |
| No | 304 | 24.5 | |
| Glasgow scale | |||
| <9 | 77 | 88.8 | 0.001a |
| <9 | 250 | 33.6 | |
| Antiplatelet | |||
| Yes | 55 | 35 | 0.42a |
| No | 272 | 24.5 | |
| OAC | |||
| Yes | 35 | 55 | 0.02a |
| No | 292 | 24 | |
| INR | |||
| <1.2 | 294 | 23 | 0.105b |
| 1.2–2 | 9 | 110 | |
| 2.1–3 | 8 | 32 | 0.058b |
| <3 | 16 | 53 | |
| Site | |||
| Supratentorial | 289 | 26 | 0.12a |
| Infratentorial | 53 | 31 | |
| Intraventricular dump | |||
| Yes | 205 | 18 | 0.12a |
| No | 122 | 60 | |
| Time to the image | |||
| Less than 12h | 227 | 27 | 0.12a |
| More than 12h | 100 | 23.25 | |
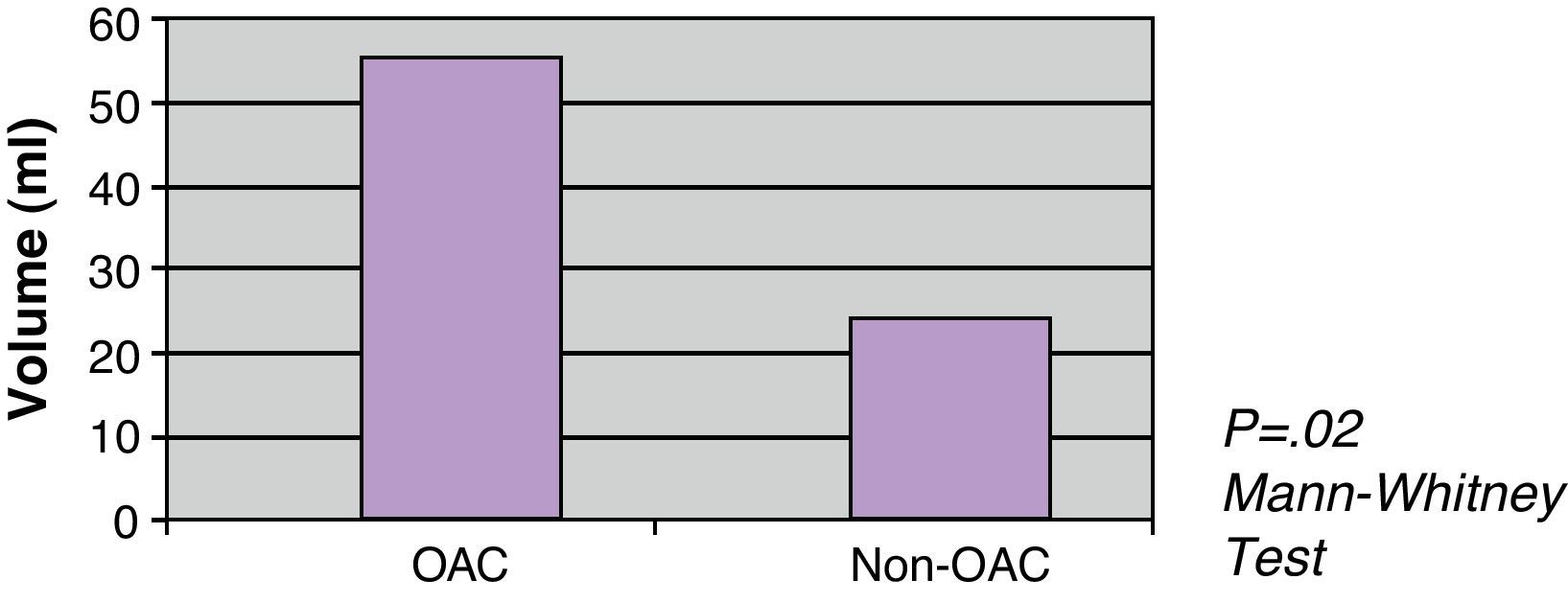
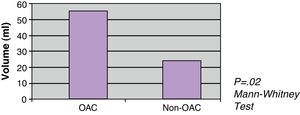
The OAC was correlated with the largest initial ICH volume, with the median volume between OAC patients being 55ml and non-OAC patients having a median of 24ml (P=.02) (Fig. 2). There was no statistically significant association between volume and INR (Spearman rho=0.105; P=.058).
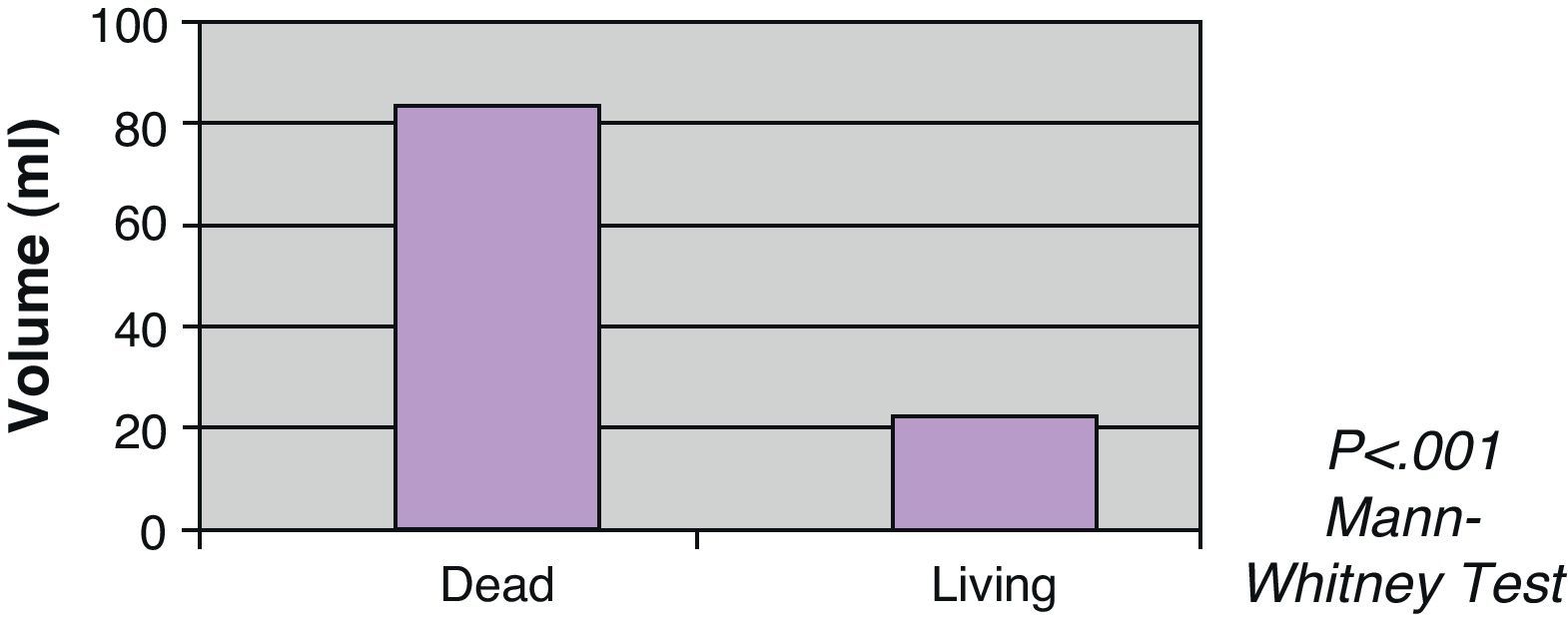
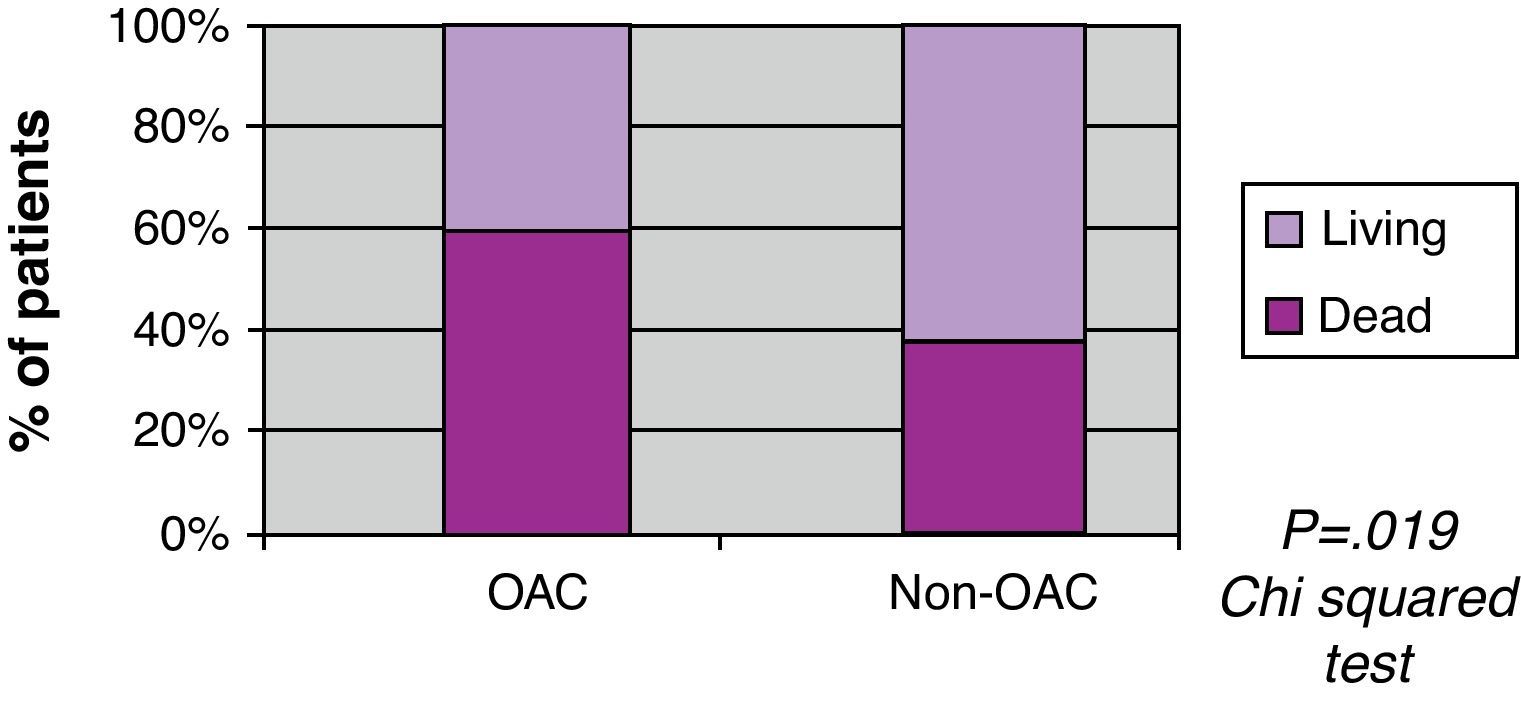
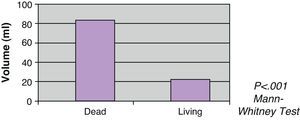
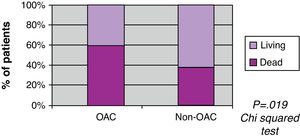
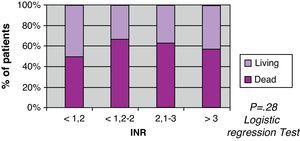
Greater mortality was seen with volume increase, with a median among living patients of 22ml, and of 86ml among the deceased (Fig. 3). A greater mortality was also seen in patients with OAC (60% vs 35%) in the univariate analysis (Fig. 4). When the INR was adjusted with the volume in the logistic regression test, there was no statistically significant association with mortality (Fig. 5).
DiscussionOur study shows that mortality from ICH in patients treated with oral anticoagulants is significantly greater than in those not treated, reaching 60% in the 30 days after the stroke occurred. This could be partially explained by the greater haematoma volume seen in this patient group, a variable that is widely accepted in literature as a poor outcome factor for this pathology.12,13 Similar figures for haematoma volume have been presented in previous studies.6,14–17
A limitation of the work was not being able to know the frequency, amplitude and duration of the increase in intracranial bleeding in the overall series or in the OAC, as no images were taken in a series. Haematoma expansion after the stroke could be the cause for the great mortality in this patient group, although it is not widely accepted, as progressive haematoma size increase not related to OAC has been reported.18 The interpretation could be overestimated by the greater speed with which cerebral images could be taken of OAC patients and by carrying out images in a series of these patients.6–9
There are few works studies on the relationship between anticoagulation level and initial ICH volume. A recent study shows that the significant increase in haematoma volume occurs with INR values that are greater than 3, suggesting that haematoma expansion causes this during the first few hours.8 Two previous studies do not show the relationship between the anti-coagulation level and volume, postulating a phenomenon of “all or nothing”.6,7 We have not found publications on mortality associated to INR values in any of the literature. In our work we did not find a significant association either between the INR value and volume or with mortality at 30 days.
ConclusionAnti-coagulated patients present greater mortality through ICH than patients not treated. This outcome is independent of the INR value at the time of presentation, which means that the sole fact of receiving anticoagulant treatment, despite proper controls, aggravates the prognosis.
However, the current recommendations for ICH steer towards correcting coagulation quickly, although which treatment is best to change the natural history of this pathology in this patient subgroup still has not been confirmed.19
Conflict of interestsThe authors have no conflict of interests to declare.
Presented as a poster at XLVI Congreso Argentino de Neurología. Sociedad Neurológica Argentina. Mar del Plata, 14th–17th October 2009.
Please cite this article as: Sousa LD, et al. ¿Es el cociente normalizado internacional un factor pronóstico de mortalidad en hemorragias intracerebrales? Neurología. 2011;26:528–32.