When secondary headache is suspected and the patient is referred to the emergency department or to the outpatient neurology clinic, it is important to know which are the appropriate complementary examinations to perform and the suitable referral pathway for patients to follow.
In order to establish recommendations on this matter, the Spanish Society of Neurology's Headache Study Group (GECSEN) has decided to issue a series of agreed recommendations constituting a referral protocol for patients with headache and/or craniofacial neuralgias.
DevelopmentYoung neurologists with an interest and experience in headache were invited to draft a series of practical guidelines in collaboration with GECSEN's Executive Committee. For practical reasons, the document was divided into 2 articles: the first focuses on primary headaches and craniofacial neuralgias and this second article on secondary headaches and other craniofacial pain. In order for the recommendations to be helpful for daily practice, they follow a practical approach, with tables summarising referral criteria, examinations to be performed, and referral to other specialists.
ConclusionsWe hope to offer a guide and tools to improve decision-making regarding patients with headache, identifying complementary tests to prioritise and referral pathways to be followed, in order to avoid duplicated consultations and delayed diagnosis and treatment.
Cuando se sospecha que estamos ante una cefalea secundaria y se deriva un paciente a Urgencias o a la consulta de Neurología es importante sabre qué exploraciones complementarias son oportunas hacer en cada caso, además de saber posteriormente cuál es el circuito adecuado que ha de seguir el paciente.
Por este motivo, el Grupo de Estudio de Cefaleas de la Sociedad Española de Neurología (GECSEN) ha decidido crear unas recomendaciones consensuadas que establezcan un protocolo de derivación de pacientes con cefalea y/o neuralgias craneofaciales.
DesarrolloSe ha contactado con neurólogos jóvenes con interés y experiencia en cefalea y con la Junta Directiva del GECSEN han desarrollado este documento que, por razones prácticas, se ha dividido en 2 artículos. El primero centrado en las cefaleas primarias y neuralgias craneofaciales, y este centrado en las cefaleas secundarias y otros dolores craneofaciales. El enfoque es práctico, con tablas que resumen los criterios de derivación con exploraciones complementarias y otros especialistas a los que derivar, para que sea útil y facilite su uso en nuestra práctica asistencial diaria.
ConclusionesEsperamos ofrecer una guía y herramientas para mejorar la toma de decisiones ante un paciente con cefalea valorando exploraciones a priorizar y qué circuitos seguir para así evitar la duplicación de consultas y retrasos en el diagnóstico y en el tratamiento.
The Spanish Society of Neurology's Headache Study Group (GECSEN) has detected that patients are attending consultation for headache without having undergone the necessary complementary tests or followed the appropriate care circuits, and are sometimes referred at an inopportune time or without the necessary level of urgency/priority.
We have therefore drafted a series of consensus recommendations based on published scientific evidence and our own experience, establishing referral protocols for patients with secondary headache and/or craniofacial pain from emergency or primary care (PC) departments. These are general recommendations and will require adaptation to the specific circumstances of each centre.
These guidelines were drafted with the collaboration of young neurologists with experience in treating headaches. For practical reasons, they are divided into 2 publications: the present work, focusing on secondary headache and craniofacial pain, and another discussing primary headache and neuralgias.
The types of secondary headache addressed in this article are associated with: head trauma, vascular disorders, medication overuse, cerebrospinal fluid (CSF) hyper-/hypotension, migraine with pleocytosis and other craniofacial pains, such as Tolosa–Hunt syndrome, Raeder (or paratrigeminal oculosympathetic) syndrome, burning mouth syndrome, and persistent idiopathic facial pain. We present each type of headache and briefly describe the diagnostic criteria according to the International Headache Society's International Classification of Headache Disorders (ICHD-3 beta),1 the most important differential diagnoses to be considered, and tables illustrating the protocols for action and referral from emergency departments and PC.
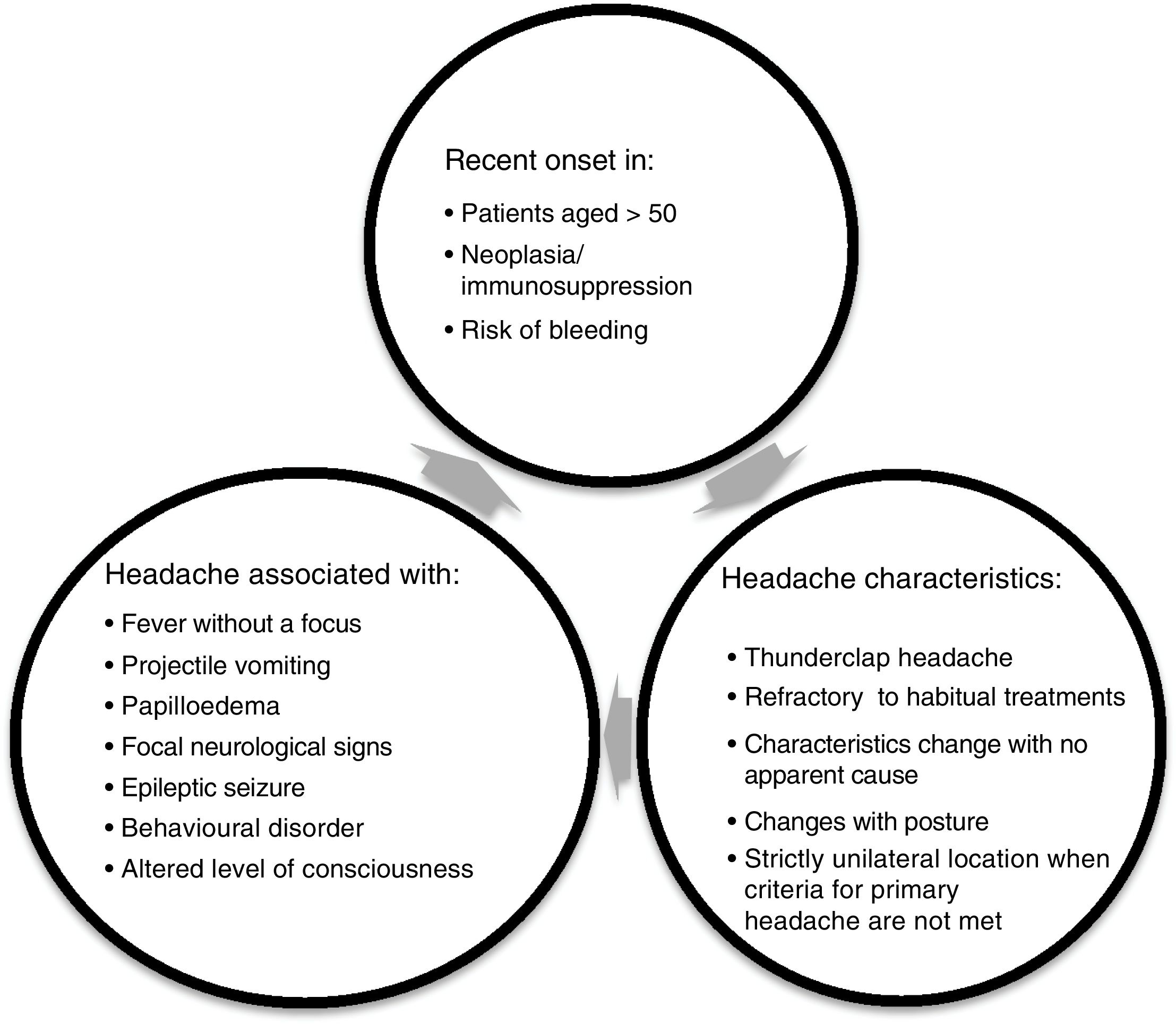
RecommendationsThe most important task when assessing patients with headache, whether in PC or at the emergency department, is to confirm the absence of alarm symptoms (Fig. 1), as these can indicate that the patient may have headache secondary to another condition.
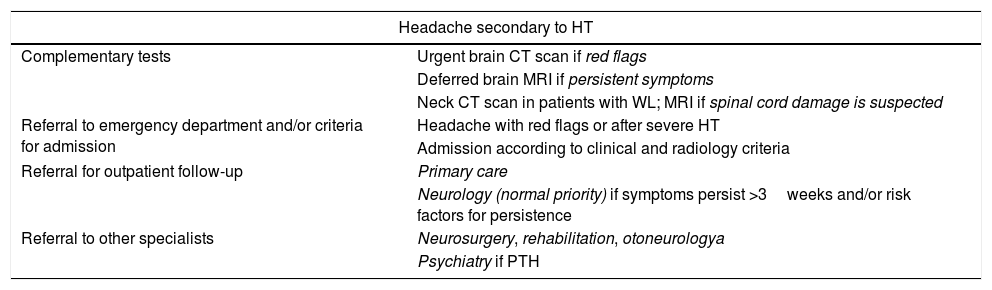
Headache attributed to traumatic injury to the headThis condition is defined as a headache occurring in the 7 days following head trauma or the 7 days after consciousness is regained. These are considered acute headaches in the first 3 months after onset, and persistent if they continue for longer periods. Whiplash (WL) is caused by acceleration/deceleration and flexion/extension of the neck. Post-traumatic headache (PTH) is associated with a wide variety of symptoms: headache, dizziness, impaired concentration, psychomotor retardation, insomnia, anxiety, and irritability.1 Neuroimaging studies are recommended if the patient has suffered moderate or severe trauma (loss of consciousness >30min, Glasgow coma scale >13, post-traumatic amnesia >24hours, altered level of consciousness >24hours, traumatic brain injury: cranial fracture, cerebral or subarachnoid haemorrhage or brain contusion),2 or shows focal neurological deficit or behavioural/personality alterations. In patients with WL, it is necessary to rule out fractures/joint dislocation and evaluate the possibility of spinal cord injury.3,4 Referral to other specialists will depend on the patient's pathology (subarachnoid or subdural haemorrhage, inner ear damage, etc.) and symptoms. Patients with PTH often also require psychological support.5,6 Headache usually improves at 3 weeks, although there is a range of predisposing factors for longer duration: age <60years, previous primary headache, psychiatric comorbidity, medication overuse, association with PTH, previous bleeding revealed by neuroimaging and/or post-traumatic epilepsy (Table 1).6–8
Protocol for action and referral from emergency departments and PC for headache secondary to HT.
| Headache secondary to HT | |
|---|---|
| Complementary tests | Urgent brain CT scan if red flags |
| Deferred brain MRI if persistent symptoms | |
| Neck CT scan in patients with WL; MRI if spinal cord damage is suspected | |
| Referral to emergency department and/or criteria for admission | Headache with red flags or after severe HT |
| Admission according to clinical and radiology criteria | |
| Referral for outpatient follow-up | Primary care |
| Neurology (normal priority) if symptoms persist >3weeks and/or risk factors for persistence | |
| Referral to other specialists | Neurosurgery, rehabilitation, otoneurologya |
| Psychiatry if PTH | |
CT, computed tomography; HT, head trauma; MRI, magnetic resonance imaging; PTH, post-traumatic headache; WL, whiplash.
a According to pathology and symptoms.
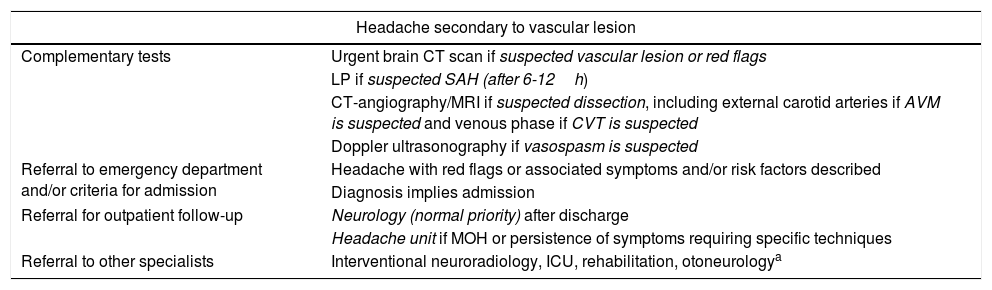
Described below are the main causes of headache attributed to vascular disorders (Table 2).
Protocol for action and referral from emergency departments and PC for headache secondary to vascular lesion.
| Headache secondary to vascular lesion | |
|---|---|
| Complementary tests | Urgent brain CT scan if suspected vascular lesion or red flags |
| LP if suspected SAH (after 6-12h) | |
| CT-angiography/MRI if suspected dissection, including external carotid arteries if AVM is suspected and venous phase if CVT is suspected | |
| Doppler ultrasonography if vasospasm is suspected | |
| Referral to emergency department and/or criteria for admission | Headache with red flags or associated symptoms and/or risk factors described |
| Diagnosis implies admission | |
| Referral for outpatient follow-up | Neurology (normal priority) after discharge |
| Headache unit if MOH or persistence of symptoms requiring specific techniques | |
| Referral to other specialists | Interventional neuroradiology, ICU, rehabilitation, otoneurologya |
AVM, arteriovenous malformation; CT, computed tomography; CVT, cerebral venous thrombosis; LP, lumbar puncture; MOH, medication-overuse headache; MRI, magnetic resonance imaging; SAH, subarachnoid haemorrhage.
This condition is usually more frequent in young adult patients. Headache is the first and most frequent symptom. It is generally unilateral, located in the occipital/nuchal region ipsilateral to the dissection, pulsatile, and with sudden onset; pain can be aggravated or alleviated with specific body positions. It is often accompanied by dizziness, neck pain, syncope, amaurosis fugax, Horner syndrome, tinnitus, facial swelling, and dysgeusia.2,9 It is important to enquire about neck trauma or manipulation at consultation. Headache persists beyond the first 3 months in 25% of patients.10
Headache attributed to non-traumatic intracranial haemorrhage (subarachnoid haemorrhage/arteriovenous malformation)It is essential to rule out subarachnoid haemorrhage in patients presenting intense, sudden onset headache which peaks quickly.11 The cerebellum and occipital lobe are the locations of lobar haemorrhage most frequently associated with thunderclap headache.12 Besides the alarm criteria, we must also take into account family history, age >40years, neck pain or stiffness, fundoscopic examination revealing subhyaloid haemorrhage, onset during exercise, and limited neck flexion.13 Risk factors for persistent headache are previous primary headache, stroke, vasospasm, and absence of endovascular therapy.14 It is important to note that non-steroidal anti-inflammatory drugs should be avoided, and that triptans are contraindicated.
Headache attributed to cerebral venous thrombosisHeadache is the most common symptom in 15%-40% of cases,2 but is typically accompanied by focal signs, subacute encephalopathy, or cavernous sinus syndrome.15 It may progress as insidious or thunderclap headache. Cerebral venous thrombosis should be considered in women using hormonal contraceptives and during pregnancy and the postpartum period, and patients with such risk factors as haematological alterations.16
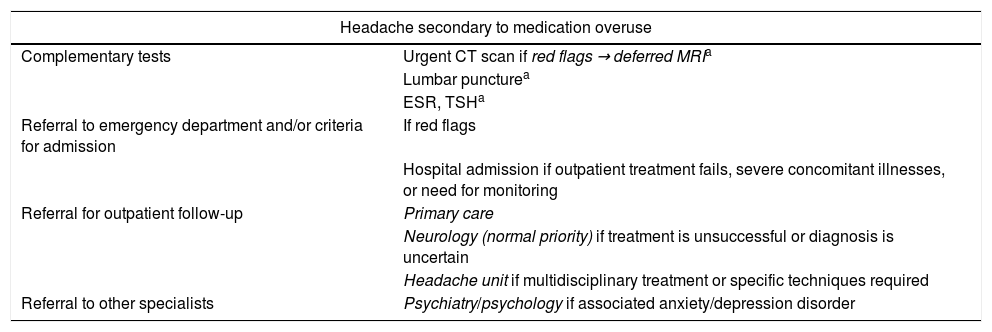
Medication-overuse headachesMedication-overuse headache (MOH) is a secondary headache caused by the overuse of symptomatic medication. It is a chronic condition and occurs if these drugs are consumed in excess (>10days per month for ergot derivatives, triptans, combined analgesics, and opioids, and >15days for simple analgesics) for longer than 3 months. The type and location of pain tend to be similar to those of the pre-existing headache, generally migraine or tension-type, but can vary, and even be accompanied by nausea, difficulty concentrating, memory problems, and irritability.17 These characteristics generally revert to their normal level when the patient stops using the drug or drugs responsible. MOH is more frequent at younger ages and in women.18
Physicians should take into account that many symptoms, including nausea, vomiting, sleep difficulties, and anxiety, may worsen during withdrawal from these medications, particularly in the first weeks.19 Outpatient treatment is recommended during patients’ withdrawal, as it has been observed to achieve better results and to involve lower risk of relapse. Furthermore, there is no difference in the reduction in the number of headache days, compared to hospitalised patients.20 Therapeutic decisions must take into account family support, patient motivation, psychiatric comorbidity, or the need for monitoring,21 in addition to the hospital resources available and the need for multidisciplinary therapy (Table 3).22
Protocol for action and referral from emergency departments and PC for medication-overuse headache.
| Headache secondary to medication overuse | |
|---|---|
| Complementary tests | Urgent CT scan if red flags → deferred MRIa |
| Lumbar puncturea | |
| ESR, TSHa | |
| Referral to emergency department and/or criteria for admission | If red flags |
| Hospital admission if outpatient treatment fails, severe concomitant illnesses, or need for monitoring | |
| Referral for outpatient follow-up | Primary care |
| Neurology (normal priority) if treatment is unsuccessful or diagnosis is uncertain | |
| Headache unit if multidisciplinary treatment or specific techniques required | |
| Referral to other specialists | Psychiatry/psychology if associated anxiety/depression disorder |
CT, computer tomography; ESR, erythrocyte sedimentation rate; MRI, magnetic resonance imaging; TSH, thyroid stimulating hormone.
Headache caused by high CSF pressure (>25cm H2O), usually accompanied by other clinical symptoms and/or signs of intracranial hypertension. It resolves after normalisation of CSF pressure. Attacks usually occur daily and are aggravated by the Valsalva manoeuvre, exercise, and supine position, but may also simulate migraine headaches.23 There are often associated symptoms, including pulse-synchronous tinnitus, temporary darkening of the vision linked to changes in posture, cervical pain, and back pain, with 25% of patients experiencing diplopia due to sixth cranial nerve involvement and reduced visual acuity. Intracranial hypertension is characterised by certain radiology findings, such as empty sella turcica, distension of the perioptic subarachnoid space, posterior scleral flattening, optic disc protrusion into the globe, and transverse cerebral venous sinus stenosis.
Intracranial hypertension can be idiopathic, a form which is typically seen in young women; however, other aetiologies are possible, for example metabolic disorders (liver failure, hypercapnia, acute hypertensive crisis, Reye syndrome, and heart failure), toxic or hormonal disorders, or intracranial pathologies (space-occupying lesions, sinus thrombosis, etc.) (Table 4).
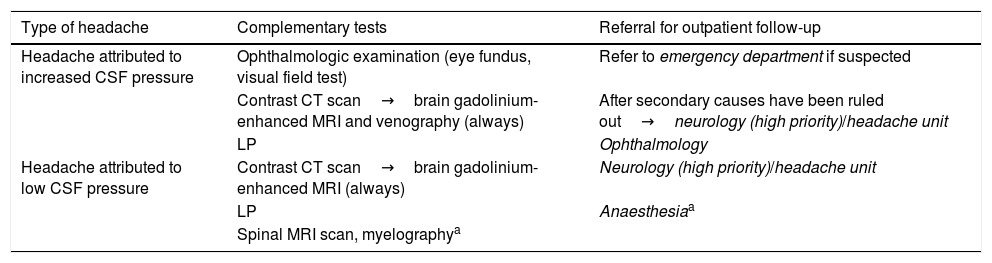
Protocol for action and referral from emergency departments and PC for headache attributed to cerebrospinal fluid alterations.
| Type of headache | Complementary tests | Referral for outpatient follow-up |
|---|---|---|
| Headache attributed to increased CSF pressure | Ophthalmologic examination (eye fundus, visual field test) | Refer to emergency department if suspected |
| Contrast CT scan→brain gadolinium-enhanced MRI and venography (always) | After secondary causes have been ruled out→neurology (high priority)/headache unit | |
| LP | Ophthalmology | |
| Headache attributed to low CSF pressure | Contrast CT scan→brain gadolinium-enhanced MRI (always) | Neurology (high priority)/headache unit |
| LP | Anaesthesiaa | |
| Spinal MRI scan, myelographya |
CT, computed tomography; LP, lumbar puncture; MRI, magnetic resonance imaging.
A predominantly occipital, bilateral orthostatic headache exacerbated by Valsalva manoeuvres, present in patients with low CSF pressure (<6cm H2O) and/or CSF leak even at normal pressure. It is generally accompanied by cervical pain, tinnitus, auditory alterations, photophobia and/or nausea. It often intensifies significantly when patients sit or stand, improving when they lie down (this is not a diagnostic criteria).1 The orthostatic nature of this type of headache may become less pronounced with time. It is most frequent in women in the fourth decade of life.24
Headache may occur due to lumbar puncture (for up to 5 days after the procedure), a CSF leak, or spontaneously. It should be noted that not all orthostatic headaches are caused by CSF alterations; differential diagnosis is necessary to rule out diabetes insipidus and cervicogenic headache, and after decompressive surgery for Chiari malformations without CSF leaks.25
Neuroimaging studies may show subdural collections, cerebellar tonsillar herniation, obliteration of subarachnoid cisterns, dilation of venous structures, collapsed ventricles, dural enhancement, or pituitary hyperaemia (Table 4).24–26
Syndrome of transient headache and neurological deficits with cerebrospinal fluid lymphocytosisSyndrome of transient headache and neurological deficits with CSF lymphocytosis (HaNDL) is also known as pseudomigraine with lymphocytic pleocytosis, and migraine with CSF pleocytosis.1,27 The condition is characterised by moderate-severe episodes of migraine-like headache accompanied by sensory symptoms (3 in 4 patients), aphasia (2 in 3, pure aphasia in 34%), and motor symptoms (<50%) lasting 4minutes to 72hours.1,28–30 Visual symptoms are rare (18%), but have been observed in migraine patients.29 HaNDL usually occurs in the third and fourth decades of life, although cases have been described in patients from 7 to 52 years of age.31 Young men are most frequently affected. Although they are usually focal, the associated symptoms may also be diffuse (e.g. acute confusional state). Fever is present in 22%-33% of cases. Papilloedema and sixth nerve palsy have also been observed.32 In 25%-40% of cases, patients report coughing, rhinitis, diarrhoea, and asthenia,31 and one in 4 patients have a viral prodrome in the preceding weeks (perhaps pointing to an autoimmune cause). Headache is usually pulsatile, bilateral, lasts from one hour to one week, and generally occurs after other symptoms (15-60min), although it may also be the first. Patients experience no meningeal symptoms and are asymptomatic between episodes.31 Lymphocytic pleocytosis (<760cells/mm3) is present in the CSF; a majority also show high CSF protein levels, and approximately 50% have raised CSF pressure. Cases generally resolve quickly, although this may take months.33
As HaNDL is mainly diagnosed by exclusion, the following conditions must be ruled out: stroke,34–36 meningoencephalitis caused by herpes simplex virus type 1,1 Mollaret meningitis (recurrent benign lymphocytic meningitis; in this case, HaNDL is differentiated by the presence of neurological deficits, the absence of meningitis and the absence of Mollaret cells in the CSF), and familial or sporadic hemiplegic migraine (which do not feature CSF lymphocytic pleocytosis). It is also important to consider treatable conditions such as Lyme disease, neurosyphilis, meningitis due to human immunodeficiency virus, encephalitis, and central nervous system vasculitis.
MRI and CT scans usually reveal normal results. For HaNDL, multimodal neuroimaging has revealed extensive hemispheric hypoperfusion in perfusion-weighted sequences, with no acute lesions in diffusion-weighted sequences or evidence of arterial occlusion in angiography sequences.34 Additional tests, such as for neuronal antibodies, are justified only when it is suspected that HaNDL is associated with acute confusional state or a behavioural disorder. For recurrent attacks, brain MRI and lumbar puncture are recommended following each episode (taking into account the time since the last lumbar puncture: a period of at least one week between punctures is recommended) (Table 5).
Protocol for action and referral from emergency departments and PC for migraine with pleocytosis (HaNDL).
| HaNDL | |
|---|---|
| Complementary tests1 | CT scan and CT-angiography→brain MRI (with angiography) |
| LP | |
| SPECTa | |
| Angiographyb | |
| Referral to emergency department | If headache is associated with fever+neurological focal signs, always refer to emergency department |
| Admission if necessary to complete study or if symptoms persist | |
| Referral for outpatient follow-up | Neurology/headache unit (high priority) |
CT, computed tomography; HanDL, syndrome of transient headache and neurological deficits with cerebrospinal fluid lymphocytosis; LP, lumbar puncture; MRI, magnetic resonance imaging; SPECT, single-photon emission computed tomography.
Unilateral orbital pain associated with paresis of one or more of the third, fourth and sixth cranial nerves, caused by granulomatous inflammation of the cavernous sinus, superior orbital fissure, or orbit. The optic nerve is occasionally also affected.1,37 The syndrome is a curable, though potentially recurrent, cause of painful ophthalmoplegia, requiring early identification and treatment. Tolosa–Hunt syndrome is diagnosed by exclusion; conditions to be ruled out are: vascular diseases (thrombosis of the sinuses, dural arteriovenous fistulas), neoplastic diseases (meningiomas, nasopharyngeal carcinomas, lymphoma, metastasis, etc.), infectious diseases (fungal infections, tuberculosis, syphilis, actinomycosis), specific granulomatous diseases (Wegener granulomatosis, sarcoidosis, giant-cell arteritis, systemic lupus erythematosus, etc.) and such other pathologies as diabetes mellitus.38–44 The purpose of the brain MRI is to detect granulomatous infiltrates in the cavernous sinus, the parasellar region, the orbital apex, the superior orbital fissure, or the orbit, according to ICHD-3 beta (Table 6).45,46
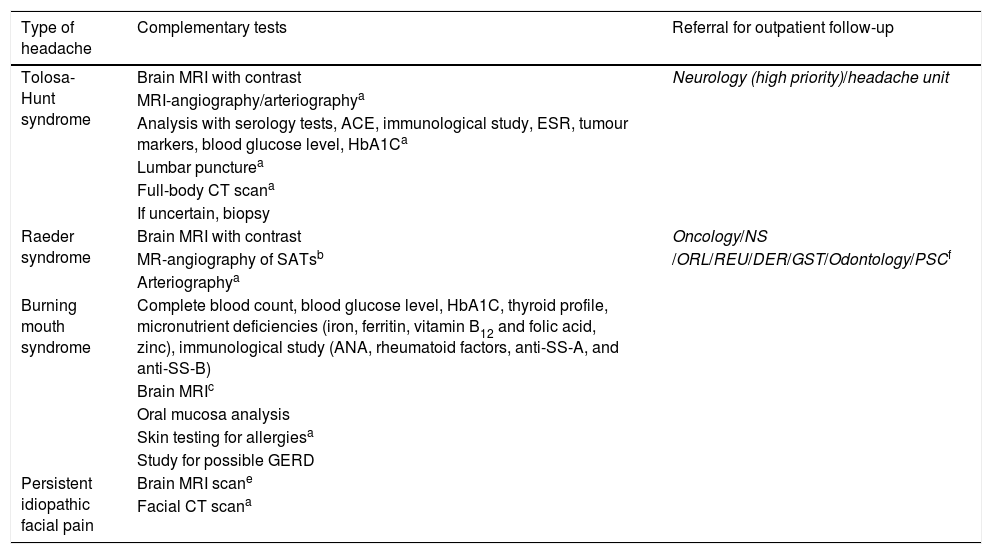
Protocol for action and referral from emergency departments and PC for other craniofacial pains.
| Type of headache | Complementary tests | Referral for outpatient follow-up |
|---|---|---|
| Tolosa-Hunt syndrome | Brain MRI with contrast | Neurology (high priority)/headache unit |
| MRI-angiography/arteriographya | ||
| Analysis with serology tests, ACE, immunological study, ESR, tumour markers, blood glucose level, HbA1Ca | ||
| Lumbar puncturea | ||
| Full-body CT scana | ||
| If uncertain, biopsy | ||
| Raeder syndrome | Brain MRI with contrast | Oncology/NS |
| MR-angiography of SATsb | /ORL/REU/DER/GST/Odontology/PSCf | |
| Arteriographya | ||
| Burning mouth syndrome | Complete blood count, blood glucose level, HbA1C, thyroid profile, micronutrient deficiencies (iron, ferritin, vitamin B12 and folic acid, zinc), immunological study (ANA, rheumatoid factors, anti-SS-A, and anti-SS-B) | |
| Brain MRIc | ||
| Oral mucosa analysis | ||
| Skin testing for allergiesa | ||
| Study for possible GERD | ||
| Persistent idiopathic facial pain | Brain MRI scane | |
| Facial CT scana |
ACE, angiotensin converting enzyme; ANA, antinuclear antibodies; CT, computed tomography; DER, dermatology; ESR, erythrocyte sedimentation rate; GST, gastroenterology; GERD, gastro-oesophageal reflux disease; HbA1C, glycated haemoglobin; MRI, magnetic resonance imaging; NS, neurosurgery; ORL, otorhinolaryngology; PSC, psychiatry; REU, rheumatology; SAT, supra-aortic trunk; SS, Sjögren syndrome.
A constant, unilateral pain in the ophthalmic branch of the trigeminal nerve, sometimes extending to the maxillary branch, accompanied by Horner syndrome with miosis and ptosis. Anhydrosis is rare. The cause is a lesion in the middle cranial fossa or the ipsilateral carotid artery.1,47–49
Given the multiple potential causes of these symptoms, it is necessary to rule out such vascular processes as aneurysm,50 dissection,51,52 or stenosis of the internal carotid artery, parasellar tumours, pituitary adenoma, meningioma, chordoma, nasopharyngeal tumours, infectious processes such as herpes zoster, maxillary sinusitis, chronic otitis media,53 and primary headaches such as ophthalmoplegic migraine or cluster headache (Table 6).
Burning mouth syndromeBurning mouth syndrome is characterised by a burning sensation or dysaesthesia in the oral mucosa, for at least 2hours per day and for at least 3 months, with no identifiable cause.1 Some patients also report dysgeusia or hypoesthesia.54,55
Diagnosis should begin by excluding secondary causes, principally: local causes (dental alterations, mechanical [prostheses] or chemical oral irritants, allergic stomatitis, infectious stomatitis [oral candidiasis is one of the most frequent secondary causes], xerostomia [mainly induced by local radiotherapy]); systemic causes (iron deficiency [with or without anaemia], or vitamin B6 or B12, folic acid, or zinc deficiency); endocrine diseases (diabetes mellitus, hypothyroidism); connective tissue diseases (Sjögren syndrome is one of the most important conditions to rule out); drugs (ACE inhibitors, oral antidiabetic drugs, chemotherapy [temporal association]); gastro-oesophageal reflux disease; and psychological causes (depression, anxiety) (Table 6).56
Persistent idiopathic facial painPersistent idiopathic facial pain is a persistent facial and/or oral pain which does not follow the distribution of any peripheral nerve, and is present for at least 2hours per day, for 3 months, without any neurological deficit.1,57 One subtype is atypical toothache, defined as pain in one or several teeth or in a tooth socket following extraction, with no objective underlying local cause. More circumscribed forms (idiopathic rhinalgia and idiopathic ophthalmodynia) have also been described.58 Diagnosis is by exclusion, after clinical criteria and the progression of the condition over time have allowed other causes of facial pain or the facial expression of other primary headaches to be ruled out. There are no guidelines or consensus on which complementary tests should be performed (Table 6).59,60
Differential diagnosis should take into account:
- (1)
Headache or facial pain attributed to pathologies of the cranium, neck, eyes, ears, nose, paranasal sinuses, teeth, and mouth (ICHD-3 beta, section 11). Among other conditions, this includes temporomandibular disorder.1,6
- (2)
Painful cranial neuropathies and other facial pains (ICHD-3 beta, section 13). The most important types to consider, due to their frequency or clinical similarity, are:
- a.
Trigeminal neuralgia.
- b.
Post-traumatic trigeminal neuropathy (trauma or iatrogenesis).
- c.
Other neuralgias of pericranial nerves.
- a.
- (3)
Facial expression of primary headaches such as migraine or certain trigeminal autonomic cephalalgias.
While a good clinical history is always important, it is essential in diagnosing secondary headaches, and may lead us down diagnostic pathways we may otherwise not have explored.
The aim of these protocols is to achieve better understanding of complementary tests, of criteria for referral to emergency departments and for admission, of which specialists should evaluate patients, and of how referral should be sought, with a view to enabling better treatment of patients with headache, both from PC physicians and emergency departments.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Gago-Veiga AB, Díaz de Terán J, González-García N, González-Oria C, González-Quintanilla V, Minguez-Olaondo A, et al. Cómo y cuándo derivar un paciente con cefalea secundaria y otros tipos de dolores craneofaciales desde Urgencias y Atención Primaria: recomendaciones del Grupo de Estudio de Cefaleas de la Sociedad Española de Neurología. Neurología. 2020;35:323–331.