Spinal cord infarction is a rare condition accounting for less than 1% of all ischaemic vascular processes of the central nervous system.1 It is characterised by rapid progression of symptoms, a specific deficit pattern, and pain in some cases. Rostrocaudal location and transverse propagation are key features of this condition. Symptoms are usually subacute and develop in a few hours.2 The spinal cord's blood supply is provided by the anterior spinal artery that irrigates the 2 anterior thirds of the medulla, as well as the 2 posterior spinal arteries.3 Magnetic resonance imaging (MRI) is the diagnostic tool of choice for spinal cord infarction. T2-weighted sequences show hyperintense lesions within the first 8hours to several days from symptom onset4; results from spinal cord arteriography are usually normal. There are several aetiologies for spinal cord infarction. The most frequent causes are haemodynamic compromise secondary to aortic dissection or aortic manipulation and atheromatous plaque blocking the ostia of the arteries that supply the spinal cord. Other aetiological mechanisms include embolism, vasculitis in autoimmune diseases, radiotherapy, and vascular malformations.
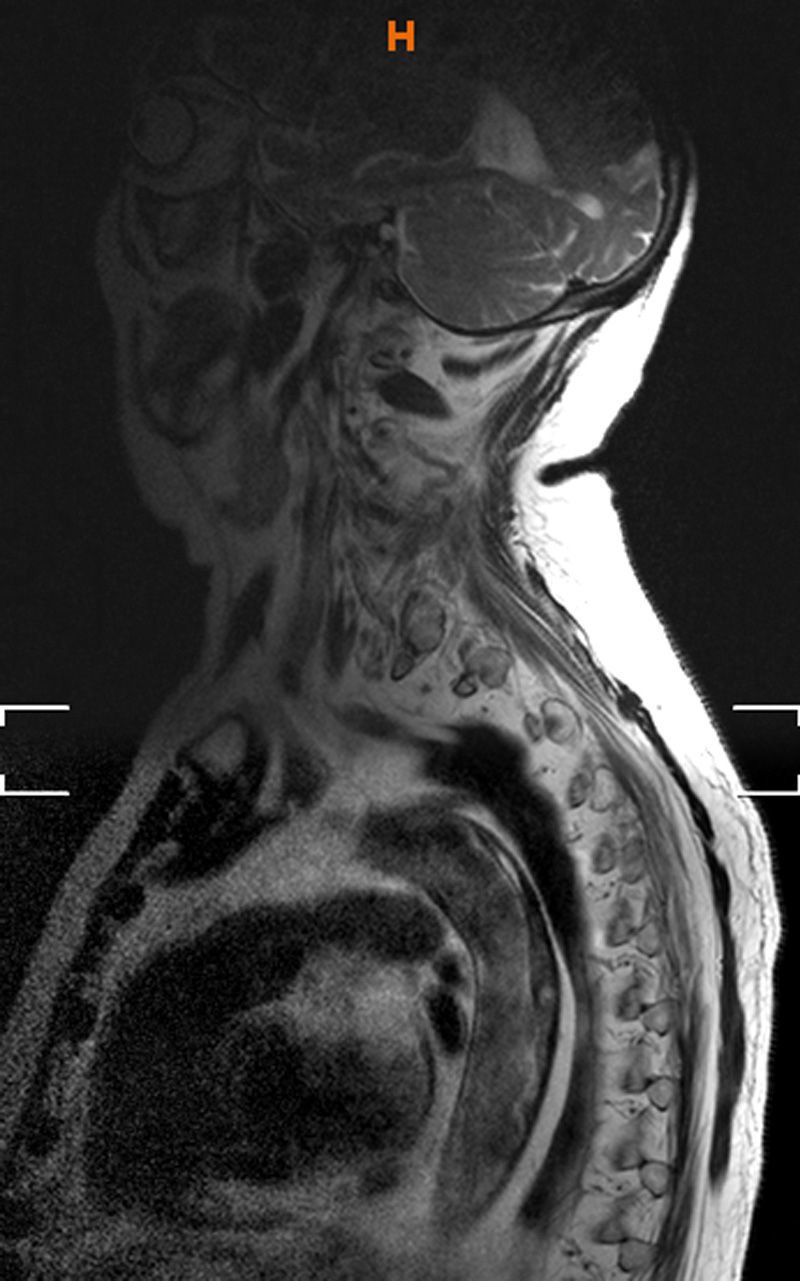
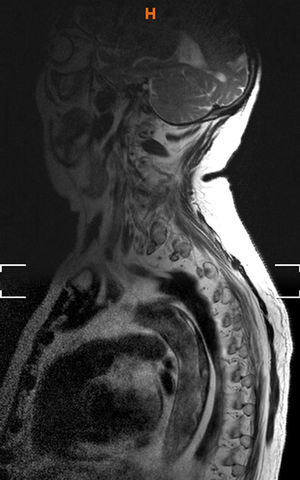
We present a case of fulminant myopathy of ischaemic origin. Our patient, a 79-year-old man, was an obese, hypertensive former smoker with a history of ischaemic heart disease, atrial fibrillation, peripheral artery disease, hyperlipidaemia, and polymyalgia rheumatica. He was treated with dabigatran, pentoxifylline, prednisone, lisinopril, bisoprolol, spironolactone, furosemide, and simvastatin. The patient reported good adherence to his medications. He came to the emergency department due to sudden paraplegia preceded by pain in the lumbar region with ascending radiation along the vertebral column to the interscapular region. He reported no prior trauma or considerable physical exertion. The initial neurological examination revealed flaccid paraplegia with a sensory level of T3 and impaired sensitivity of the posterior column. He was admitted with a diagnosis of medullary syndrome of possible vascular aetiology. Despite treatment with steroids, antiplatelets, and anticoagulants, his symptoms had exacerbated 24hours later: paresis had progressed to affect the upper limbs, and the sensory level rose to C7. Spinal MRI scan revealed an extensive spinal cord infarction from C4 to the conus medullaris (the T8-11 segment was preserved) due to a lesion in the anterior spinal arteries, and signal alterations at the T9 vertebral body, suggesting spinal cord ischaemia caused by obstruction of the radicular arteries (Fig. 1). The MRI image also showed the incidental finding of a lesion in the lumen of the thoracic aorta; this finding was interpreted as indicative of thrombus and dissection at the posterior wall of the aorta (Fig. 2). A CT angiography study showed abundant calcified and non-calcified atheromatous plaque. Hypodensities compatible with thrombus were observed in the posterior inner area of the lumen of the aorta towards the cranium and up to the aortic arch. The vascular surgery department confirmed the presence of 3 thrombi: a semilunar thrombus on the posterior wall of the thoracic aorta originating at the ostium of the left subclavian artery; a floating thrombus at T8-T10; and a mural thrombus above the bifurcation of the iliac arteries. Aortic dissection was ruled out. A thoracic endoprosthesis (Valiant, Medtronic) was placed from the left subclavian artery to the celiac artery to exclude the aortic floating thrombus. Surgery was performed without incident and CT angiography confirmed that the endoprosthesis had been placed correctly. The patient started rehabilitation therapy but showed no improvements and died 2 months later of respiratory failure.
This case of extensive spinal cord infarction was secondary to progressive thrombosis of the aorta. We first considered aortic dissection to be the most likely cause. However, a CT angiography of the aorta revealed a thrombus on the posterior wall of the thoracic aorta, which blocked the ostia of the spinal arteries, leading to thrombosis of the aorta progressing proximally and progressive extension of the affected area of the spinal cord.
Thrombosis of the aorta is an infrequent condition with disabling and devastating effects; very few cases have been described in the literature.5 It has different aetiologies, including prothrombotic states, inflammatory processes, and atherosclerotic changes involving large ulcerated and/or calcified plaques. Several predisposing factors linked to platelet aggregation and coagulation may be involved in aortic thrombus formation. Although oral anticoagulants have no impact on platelet aggregation, they can in theory prevent or reduce formation of red clots on complicated plaque. Using oral anticoagulants to treat critical carotid artery stenosis with ulcerated plaque or moving thrombi is based on this assumption.6 Oral anticoagulants, whether traditional vitamin K antagonists or the new thrombin and factor Xa inhibitors, have been shown to reduce risk of recurrent embolism in patients with non-valvular and valvular atrial fibrillation (vitamin K antagonists only); however, evidence is not sufficient to support oral anticoagulants as preventive treatment for local arterial thrombosis, especially in the case of new anticoagulants.
In our case, the infarcted area of the spinal cord was unusually large (from C4 to the conus medullaris) as a result of the aortic thrombosis secondary to a severe atherothrombotic disease. We should highlight that previous anticoagulant therapy with dabigatran failed to prevent thrombus formation and limit its development.
Please cite this article as: Gutiérrez-Alvarez AM, Sagarra-Mur D, del Valle-Sanchez M, Jimenez-Corral C. Devastadora mielopatía por trombo aórtico en paciente anticoagulado. Neurología. 2015;30:317–319.