In recent decades, many stroke rehabilitation methods have been developed. Mental practice (MP) is a dynamic state in which the subject evokes an imaginary representation of a motor action or skill in order to learn or perfect that action. Although functional imaging has shown that MP produces similar cortical activation patterns to those of movement, the clinical effectiveness of such methods in rehabilitation and functional recovery has yet to be demonstrated.
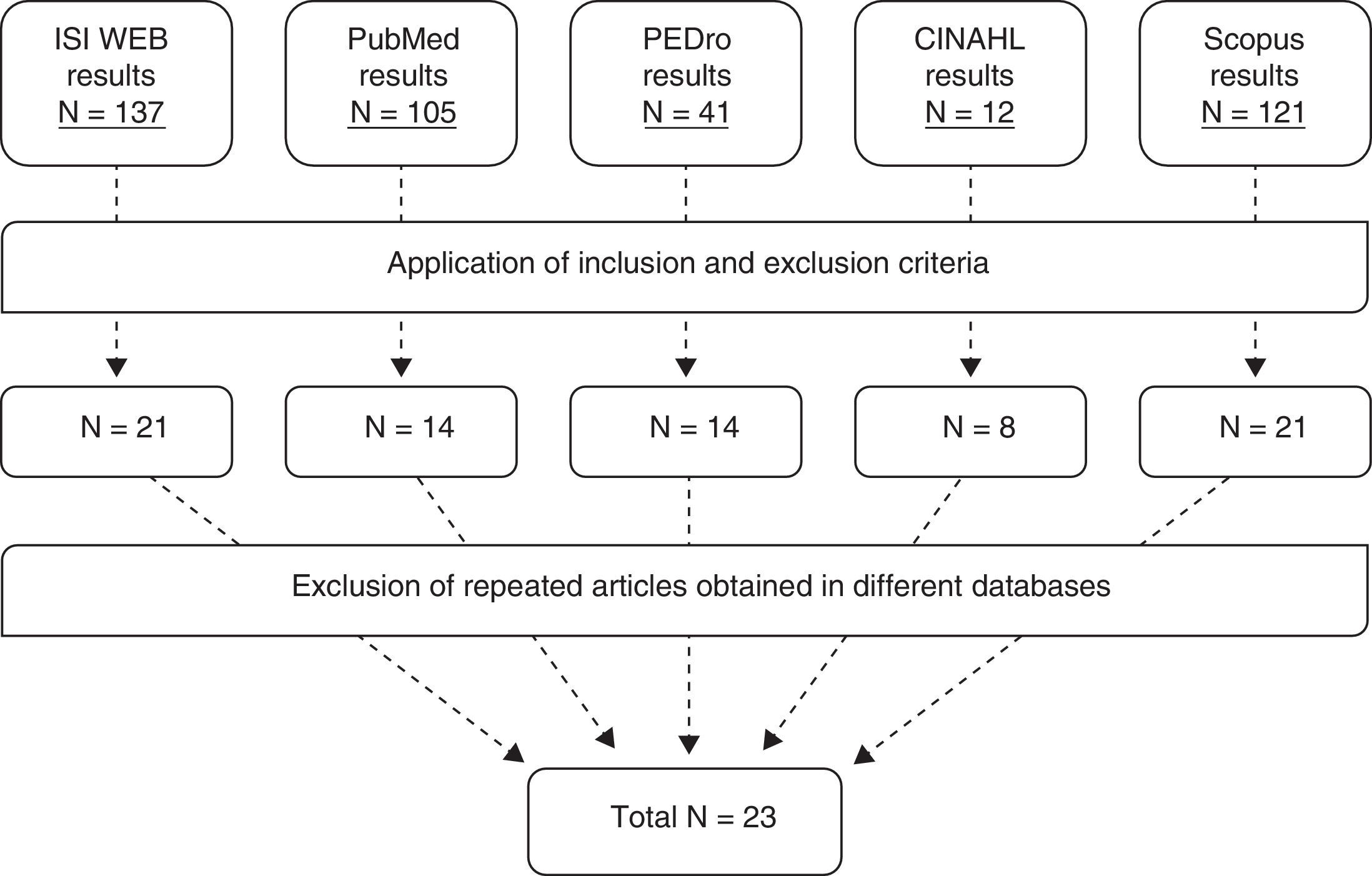
DevelopmentSystematic search of all clinical studies published in the main scientific databases between December 2011 and October 2012 concerning MP in stroke rehabilitation. We selected 23 clinical trials testing different MP protocols in patients with hemiparesis.
ConclusionsMP is effective when used in conjunction with conventional physical therapy for functional rehabilitation of both upper and lower limbs, as well as for the recovery of daily activities and skills. Owing to the heterogeneity of the studies with regard to the intervention protocol, specific imagery technique, time spent practicing, patient characteristics, etc., more studies are needed in order to determine the optimal treatment protocol and patient profile.
En las últimas décadas han surgido diferentes métodos de tratamiento rehabilitador para pacientes con hemiparesia. Uno de ellos es la práctica mental (PM) del movimiento, consistente en la evocación de un movimiento o gesto por parte del sujeto con el fin de aprender o mejorar su ejecución. A pesar de que las técnicas de neuroimagen han demostrado que durante la PM se ejecutan patrones de activación neuronal similares a los que aparecen durante el movimiento, es necesario demostrar su efectividad clínica en la rehabilitación y recuperación funcional de pacientes.
DesarrolloPara ello, entre diciembre de 2011 y octubre de 2012 se realizó una búsqueda sistemática en las principales plataformas bibliográficas y bases, seleccionándose 23 ensayos clínicos referentes a distintos protocolos de PM en pacientes con hemiparesia.
ConclusionesLa PM es efectiva cuando se combina con terapia convencional en la recuperación funcional del miembro tanto inferior como superior, así como para el entrenamiento de actividades y gestos cotidianos. Dada la heterogeneidad de los estudios en cuanto a la técnica de evocación mental, el volumen de entrenamiento, los sujetos incluidos…, se necesitan más estudios para determinar el tipo de paciente y el protocolo ideal de tratamiento.
Cerebrovascular accident (CVA) has become one of the leading causes of mortality among adult populations in developed countries.1–3 In fact, stroke incidence is approximately one million yearly in the European Union.4 Care and management of patients have improved greatly over the last few years, which has in turn increased survival rates. However, stroke sequelae are still dramatic for patients. One of the most frequent is hemiplegia or hemiparesis. Hemiplegic patients present impaired mobility on one side of the body, and therefore their function and independence are severely limited, as well as their quality of life.5 The financial costs resulting from stroke, including disability payments, medical and drug expenses, and assistance for dependent persons, are enormous.
Various strategies and treatment approaches aiming to improve patient function and independence have been developed over the years.6,7 In the last 20 years, neuroimaging techniques and the discovery of mirror neurons have brought about a deeper understanding of brain function. This in turn has led to the design of new treatment approaches such as action observation,8 constraint-induced movement therapy,9 bilateral rehabilitation,10 mirror symmetric bimanual movement priming,11 use of virtual reality,12 robotics,13 or mental representation of a motor action. This article focuses on the latter.
Mental practice or motor imagery training is a type of therapy in which the patient evokes a gesture or a movement so as to learn, reinforce, or improve performance of that movement. This activity has traditionally been used in athletics14,15 in an intuitive manner, with the aim of reviewing or reinforcing the sequence of movements that make up the action to be performed. There are 2 types of imagery techniques: external or visual, in which subjects imagine seeing themselves from the viewpoint of an external observer, and internal or kinaesthetic, in which subjects imagine the sensations of motion in their own bodies.
Using new imaging techniques, research in the past few years has shown that the activation sequences in the motor cortex during mental imagery of a movement are similar to those occurring during performance of that movement.16,17 This finding serves as a scientific basis for developing a methodology for motor imagery training in both healthy and impaired subjects. Treatment strategies have recently been developed for patients with neurological disorders,18,19 but their effectiveness has yet to be proved. We need to identify the most effective procedure and the target patient, since certain lesions in some cases render the patient unable to visualise movement.20,21
Therefore, the aims of this study are to examine scientific evidence on the effectiveness of motor imagery as a post-stroke therapeutic option for hemiparetic patients (with impairment of both the upper and lower limb), check the viability of establishing a mental imagery protocol, and assess the best way to do so.
DevelopmentMaterial and methodsBetween December 2011 and October 2012, we performed a systematic literature review of the following databases: ISI Web of Knowledge, PubMed, Physiotherapy Evidence Database (PEDro), Cumulative Index to Nursing and Allied Health Literature (CINAHL), and Scopus.
For searches in the ISI Web of Knowledge, we entered the combination of keywords ‘mental practice’ OR ‘mental imagery’ OR ‘motor imagery’ OR ‘locomotor imagery training’ in the ‘Title’ field. Subsequently, we selected ‘rehabilitation’ as the subject matter and ‘article’ and ‘clinical trial’ as the type of document.
We searched PubMed using the keywords ‘mental practice stroke’ OR ‘mental imagery’ OR ‘motor imagery stroke’ OR ‘locomotor imagery training’, and limited results to ‘randomised controlled trial’.
For the PEDro database, we performed 3 simple searches of the following keywords separately: ‘mental imagery’, ‘mental practice’, and ‘motor imagery’.
Using the advanced search option offered by the CINAHL database, we entered the following combination of keywords: ‘mental practice’ OR ‘mental imagery’ OR ‘motor imagery’ OR ‘locomotor imagery training’ for the ‘Title’ field and limited results to ‘randomised controlled trial’.
In Scopus, we entered the following keywords in the field ‘Article title, abstract, keywords’: [‘mental imagery’ OR ‘mental practice’ OR ‘motor imagery’ OR ‘locomotor imagery training’] AND ‘stroke’. We limited our search to the subject areas of ‘medicine’ and ‘health professions’, with ‘article’ as the type of document.
Inclusion criteriaWe included all controlled clinical trials or similarly designed pilot studies that examined patients with ischaemic or haemorrhagic CVA treated with mental practice or motor imagery and written in English or Spanish. Inclusion dates for these studies were January 2001 through September 2012.
Exclusion criteriaWe excluded those studies in which mental imagery was not used in patients with CVA. Studies of imagery for purposes other than motor relearning or recovery of motor function in stroke patients were also excluded. Articles focusing on the use of sophisticated new devices for applying the technique were excluded, as well as those studies including fewer than 10 patients or not designed as randomised clinical trials. We also eliminated articles for which full text versions were not available.
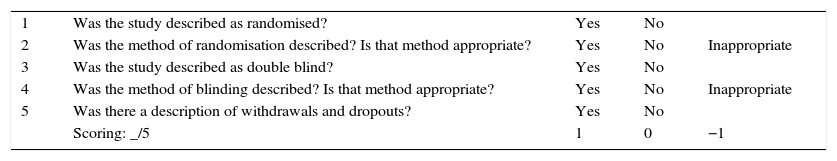
Assessment of study methodology qualityWe used the Jadad scale (Table 1) to assess the methodological quality of every article. This scale has been validated and its simplicity, effectiveness, and ease of use are widely recognised. It includes 5 items which assess whether patients have been randomised and if the randomisation method is adequate. It also assesses if the study is double-blinded and the blinding method is appropriate, and if dropout data are given.22,23
Jadad scale.
| 1 | Was the study described as randomised? | Yes | No | |
| 2 | Was the method of randomisation described? Is that method appropriate? | Yes | No | Inappropriate |
| 3 | Was the study described as double blind? | Yes | No | |
| 4 | Was the method of blinding described? Is that method appropriate? | Yes | No | Inappropriate |
| 5 | Was there a description of withdrawals and dropouts? | Yes | No | |
| Scoring: _/5 | 1 | 0 | −1 |
Results:
5/5=Excellent methodological quality
4/5=Good methodological quality
3/5=Acceptable methodological quality
2/5=Poor methodological quality
1/5=Bad methodological quality
After searching the different databases and applying inclusion and exclusion criteria, a total of 78 articles were considered valid. Excluding studies repeated in different databases yielded a total of 23 articles for inclusion in our study (Fig. 1).
Methodological quality of the studiesWe used the Jadad scale to assess the methodological quality of selected clinical trials. Double-blinding is always a challenge in a physiotherapy study. For this reason, we also specified when only the rater was blinded. Table 2 describes the methodological quality, among other characteristics, of every study included in this review.
Overview of the characteristics of reviewed studies.
| Jadad | Study and characteristics | Procedure | Studied variables |
|---|---|---|---|
| 5/5 | Author: Page et al.41Type: RCTDuration: 6 weeksParticipants: 13Diagnosis: hemiplegia in the subacute phase | SG: MI and conventional PT MI training was provided in audio tape format. Also home-based.CG: Only conventional PT | - Fugl-Meyer- ARAT |
| Author: Page et al.33Type: RCTDuration: 6 weeksParticipants: 11Diagnosis: chronic hemiplegia | SG: Conventional RHB of the paretic upper limb+30min of MP guided by audio recordingCG: Conventional RHB of the paretic upper limb+30min of relaxation therapy guided by audio recording | - Motor Activity Log- ARAT | |
| Author: Page et al.28Type: RCTDuration: 6 weeksParticipants: 32Diagnosis: chronic hemiplegia | SG: Functional RHB+30min of MP of the same activities as in PT guided by audio recordingCG: Functional RHB+30min of relaxation therapy guided by audio recording | - Fugl-Meyer- ARAT | |
| Author: Page et al.35Type: RCTDuration: 10 weeksParticipants: 10Diagnosis: chronic hemiplegia | SG: Constraint-induced movement therapy+MPCG: Constraint-induced movement therapy only | - Fugl-Meyer- ARAT | |
| Author: Page et al.34Type: prospective longitudinal studies based on a RCTDuration: 10 weeksParticipants: 21Diagnosis: chronic hemiplegia | Subjects in the SG followed a protocol combining MP with repetitive performance of a specific task. Subjects were assessed immediately after the intervention and at 3 months. | - Fugl-Meyer- ARAT- AMAT- Box and Block test | |
| Author: Page et al.24Type: RCTDuration: 10 weeksParticipants: 29Disease: mild chronic hemiplegia | 3 SG: MI (20–30–40min)+task-oriented functional therapyCG: Task-oriented therapy | - Fugl-Meyer- ARAT | |
| 3/5+blinded rater | Author: Liu et al.26Type: RCTDuration: 3 weeksParticipants: 46Disease: hemiplegia in the acute phase | SG: Functional training+MICG: Functional training | - Fugl-Meyer- Colour trails test- Ability to perform 15 trained tasks and 5 untrained tasks correctly |
| Author: Liu et al.29Type: RCTDuration: 3 weeksParticipants: 34Diagnosis: chronic hemiplegia | SG: Conventional PT+physiotherapy+MICG: Physiotherapy+conventional occupational therapy | - Fugl-Meyer- Likert-type scale- Cognistat | |
| Author: Malouin et al.31Type: RCTDuration: 4 weeksParticipants: 12Disease: chronic hemiplegia | SG: Conventional PT+MP2 CG: Conventional PT+cognitive therapyNo therapy | Analysis of vertical forces and impulses. | |
| Author: Bovend’Eerdt et al42Type: RCTDuration: 6 weeksParticipants: 30Disease: chronic hemiplegia | SG: Conventional PT and OT+MP (the technique is taught with 2 videos)CG: Conventional PT and OT+watching 2 videos on PT | - The Short-Orientation Memory concentration- Motricity Index- Barthel index- RiverMead Mobility Index- Timed Up and Go- Nottingham extended activities of daily living scale- Questionnaire on perceived effort in imagining a task | |
| Author: Riccio et al.36Type: RCTDuration: 6 weeksParticipants: 36Disease: chronic hemiplegia | Same intervention in both groups; however, while group A only received neurorehabilitation in the first 3 weeks, group B also received MP, and at 3 weeks the groups exchanged protocols. | - Motricity index subtest for the upper limb- Arm Functional Test | |
| Author: Ietswaart et al.43Type: RCTDuration: 4 weeksParticipants: 121Disease: hemiplegia in the subacute phase | SG: MI onlyCG:- Placebo intervention- Conventional rehabilitation | - ARAT- Barthel index- Functional Limitation Profile | |
| Author: Verma et al.27Type: RCTDuration: 2 weeksParticipants: 30Diagnosis: hemiplegia in the subacute phase | SG: 15min of MI+40min of task-oriented training circuit.CG: Conventional RHB using Bobath therapy | - Functional ambulation classification- RiverMead Visual Gait Assessment- Gait parameters- 10m walk test- 6min gait test- Barthel index | |
| Author: Braun et al.44Type: RCTDuration: 6 weeksParticipants: 36Diagnosis: hemiplegia in the subacute phase | SG: Conventional RHB+10 supervised MP sessions+MP without supervision (MP takes time from conventional RHB)CG: Traditional RHB+FT without supervision | - Barthel index- Motricity index- Nine Hole Peg Test- Berg Balance Scale- RiverMead Mobility Index- 10 metre walk test | |
| 3/5 | Author: Müller et al.25Type: RCTDuration: 4 weeksParticipants: 17Disease: severe hemiparesis with total paresis of the arm in a patient with CVA during the acute phase | SG: MP (train and imagine performing a sequence of movements with the affected hand)CG:- PT: Execute movements with the affected hand- Conventional PT+occupational therapy | - Neurological Motricity Index- Barthel index- Jebsen hand function test- Maximum finger-thumb opposition strength |
| Author: Liu et al.30Type: RCTDuration: 3 weeksParticipants: 35Disease: hemiplegia in the acute phase | SG: MI onlyCG: Functional RHB | Number of functional actions achieved | |
| Author: Braun et al.45Type: RCTDuration: 6 weeksParticipants: 16Disease: hemiplegia in the subacute phase | SG: Conventional RHB+MP instructionsCG: Conventional RHB | Questionnaire gathering patients’ and therapists’ opinions on the applicability of the intervention and on experiences while following the MP protocol | |
| Author: Kim et al.38Type: RCTDuration: 4 days per interventionParticipants: 15Diagnosis: chronic hemiplegia | Four interventions: visual locomotor imagery training, kinaesthetic locomotor imagery training, visual locomotor imagery with auditory step rhythm, and kinaesthetic locomotor imagery with auditory step rhythm. The order of interventions was randomised, but all subjects experienced all of the interventions. | - Timed Up and Go- EMG of quadriceps, hamstring, tibialis anterior muscle, and calf muscle on the affected side- Kinematic data in sagittal plane | |
| Author: Lee et al.37Type: RCTDuration: 6 weeksParticipants: 24Disease: chronic hemiplegia | SG: MI+treadmill gait trainingCG: Treadmill gait training | Computed analysis:- Speed- Rhythm- Cadence- Step length- Time on single limb support and double limb support | |
| 1/5 | Author: Dijkerman et al.46Type: Controlled trialDuration: 4 weeksParticipants: 20Diagnosis: chronic hemiplegia | SG: PT+MP of a non-functional specific task2 CG:- PT+visual imagery of previously seen pictures- PT exclusively | - Motor training task, Pegboard, dynamometer, position sensitivity, two-point discrimination, Recovery Locus of Control Scale, Elevator Counting of the Test of Every Day Attention, Barthel Index, and modified functional limitation profile |
| Author: Dunsky et al.40Type: Controlled trialDuration: 6 weeksParticipants: 17Disease: subacute hemiparesis | Mental imagery programme for home-based gait training | - Spatial-temporal parameters- Kinematic parameters- Tinetti- Modified Functional Walking Categories Index | |
| Author: Hwang et al.39Type: Controlled trialDuration: 4 weeksParticipants: 24Disease: chronic hemiplegia | SG: MI of locomotion+conventional PTCG: Conventional PT+watching documentary on health | - Spatio-temporal parameters- Activities-Specific Balance Confidence Scale- Berg Balance Test- Dynamic Gait Index- Modified Emory Functional Ambulation Profile | |
| Author: Guttman et al.32Duration: 8 weeksParticipants: 13Disease: chronic hemiplegia | Two interventions: mental practice of transition from sitting to rising and reaching and grasping. 4 weeks later, type of intervention was changed so that all subjects practised both techniques. | - Fugl-Meyer- Timed Up and Go- Posture grid- Reaching Performance Scale- Virtual reality glove |
AMAT: Arm Motor Ability Test; ARAT: Action Research Arm Test; PT: physiotherapy; Fugl-Meyer: Fugl-Meyer Assessment of Motor Recovery; CG: control group; SG: study group; MI: mental imagery; PP: physical practice; MP: mental practice; RHB: rehabilitation; OT: occupational therapy.
We obtained a total of 23 studies which analyse the effectiveness of mental practice or imagery.
Regarding the homogeneity of action protocols, trial durations ranged from 2 weeks to 10 weeks, with most studies lasting 6 weeks. Sample sizes ranged from a minimum of 10 to a maximum of 121 patients, although the most common sample sizes were 10 to 20 and 30 to 40. The type of intervention that combines mental imagery or practice with conventional rehabilitation (physiotherapy or occupational therapy) is predominant. In specific cases, mental imagery is combined with such other specific techniques as constraint-induced movement therapy, task-oriented circuit, or treadmill gait training. However, it is rarely used as therapy alone, since its effectiveness is usually studied as an adjuvant to conventional training. There is no universally accepted protocol although most studies analysed in our review include an initial relaxation time in which the patient can concentrate and focus his or her attention on the next task. Once this phase is completed, the patient is requested to perform a task mentally (generally using first-person imagery). This may be one of the activities performed physically during the preceding rehabilitation session, or another one to be practised later. Mental practice sessions generally last a mean of 30min. Some studies use videos to explain the technique to the patients. On some occasions, only an audio tape is used to guide the patient through the mental practice session.
All patients in each of these studies had hemiparesis or hemiplegia, although impairment was mild in some cases24 and far more severe in others.25 Likewise, articles also addressed the study of hemiplegia after acute stroke,26 during the subacute phase,27 and after chronic stroke,28 which is the most frequent.
Different questionnaires, such as ‘The movement imagery questionnaire’ and ‘The kinesthetic and visual imagery questionnaire’, have been described as tools assessing the capacity of each subject to mentally evoke a movement. Once mental practice had been completed, verification methods were used to record the time needed for each evoked gesture and compare it with the actual time to perform it. Alternatively, some patients were asked to describe the sequence of movements necessary to perform the task.
The variables used in the studies are very diverse, and the use of the Fugl-Meyer Assessment and the ARAT scales predominates among those studies analysing the effectiveness on the upper limb. Furthermore, the Barthel index, Timed Up and Go test, and the analysis of spatial-temporal parameters are used frequently in those studies analysing gait rehabilitation.
DiscussionRelearning tasks and performing them in new environmentsSome of the studies analysed in this review aim to determine the potential of mental practice to contribute to task relearning, as well as the possibility of transferring positive outcomes to new environments. For example, the study by Page et al.28 included patients with chronic hemiplegia who significantly improved the function and mobility of their impaired arms using mental practice. Furthermore, these motor changes translated to a new ability to perform a task that had not been possible for months. Authors cite 2 bases to explain this effect: firstly, mental practice is able to increase use of the affected arm, and secondly, mental practice causes brain reorganisation: new cortical areas are recruited to assist in moving the affected arm. Studies by Liu et al.26,29,30 support these findings. In these studies, patients engaging in mental practice showed statistically significant improvements in function and were more able to transfer these skills to other tasks in new environments. This happens even when patients receive potentially distracting stimuli from a different context, especially in a real environment, which is constantly changing and unpredictable.
Studies by Malouin et al.31 and Guttman et al.32 focus on a specific task: retraining the transition from sitting to standing and vice versa. Only the patients who combined both techniques showed a statistically significant increase in affected limb loading, as well as a reduction of the time necessary to perform the task. Authors observed that mental practice serves as pretraining, which increases the effectiveness of subsequent physical training. Furthermore, more benefits were observed in those subjects treated soon after the CVA, since they had less time to adopt negative habits.
Can mental practice improve function of the upper limb?Several studies25,33–36 have assessed the effectiveness of mental practice for arm rehabilitation. Studies by Page et al.33–35 find that mental practice helps improve function in the impaired upper limb by developing new motor schemes when it is combined with conventional physiotherapy,33 task oriented training,34 or constraint-induced movement therapy.35 These increases in ability were confirmed by the patients themselves, who reported being able to perform activities of daily living that they had not completed since the stroke. Authors also observed that these changes remain over time, up to 3 months after finishing the therapy.
Riccio et al.36 detected positive results in patients in the subacute phase. Mental practice achieved improvements in strength, gesture quality, and performance speed. These authors highlight the vast potential of this technique in patients able to evoke movement, since it is both discomfort- and cost-free, and can be repeated without any physical stress. Müller et al.25 also state that mental practice alone is just as effective as repetitive physical practice in the case of the pinch grip sequence.
In light of the findings described above, we can state that mental imagery, always as an adjuvant to conventional rehabilitation, leads to changes in the quality and degree of movement of the impaired arm. These improvements remain for at least 3 months after the therapy has been completed. Furthermore, engaging in mental practice means that the patient has more opportunities to train without any physical strain.
Can mental practice improve lower limb function?Most studies on metal practice published to date have assessed its effectiveness in relearning tasks performed with the arms. However, its utility in gait relearning has also been studied although to a lesser extent. Verma et al.27 assessed the effectiveness of a training programme which included a task-oriented circuit for gait rehabilitation combined with mental imagery. They found statistically significant improvements in most of the outcome measures, and independent functional gait also improved earlier than in the control group. Improvements remained until at least 6 weeks after therapy.
Furthermore, Lee et al.37 examined the effectiveness of mental imagery as a way of enhancing improvements achieved with treadmill training in cases of chronic hemiplegia. The authors detected improvements such as reduced double stance time in both the study and control groups, but they were more significant in the first group. They mentioned that motor imagery training is a low-risk and low-cost intervention.
However, Kim et al.38 compared the effect on gait performance of locomotor imagery (mental self-visualisation) and kinaesthetic imagery (imagining the sensation of performing a task) when combined with an auditory step rhythm. After the assessments, authors concluded that kinaesthetic imagery may have greater therapeutic benefits for gait performance than visual imagery, and that adding an auditory step rhythm may accentuate these benefits.
Furthermore, the study by Hwang et al.39 also showed statistically significant improvements in gait speed, length of stride, hip flexion torque, and dynamic balance in the experimental group. The authors concluded that these improvements may be explained by the transfer of skills, as well as by the psychological components of mental imagery, which reduce fear of falling.
Lastly, Dunsky et al.40 assessed the feasibility and efficacy of a home-based motor imagery gait training programme. They observed significant gains in walking speed after training (40%), and these gains were largely maintained at the 3-week follow-up evaluation. There were significant increases in stride length, cadence, and single-support time for the affected leg. Patients also improved on the gait scale of the Tinetti Performance-Oriented Mobility Assessment.
All these studies attest that mental imagery training is able to improve spatio-temporal gait parameters, especially when combined with other therapies such as task-oriented circuit training or auditory step rhythm signals. Motor imagery also seems to reduce the psychological component of fear of falling, thereby promoting walking at an earlier moment and increasing the patient's functional independence. Lastly, authors observe that mental imagery is a safe and low-cost technique that can be performed even without supervision once the patient has completed appropriate training.
Feasibility of incorporating a mental imagery protocolThe analysis of the studies mentioned above confirms that mental practice is effective as an adjuvant technique for increasing the effects of conventional therapy. However, doctors should assess the feasibility of establishing a mental imagery protocol, and determine the most effective way of conducting training. Page et al.,41 the authors of one of the studies examined here, aimed to test the feasibility of a mental imagery protocol. Results showed excellent adherence to the programme, and patients were satisfied with the outcomes. Participants in the study group showed significant improvements in their ability to use the affected hand and wrist, as well as some improvements in gross motor skills of the arm. Based on this evidence, the authors concluded that this technique is a promising cost-effective and non-invasive adjuvant to traditional therapy, which substantially reduces decline and improves functional results. The study by Guttman et al.32 also showed good adhesion among patients who even used this technique to retrain tasks they proposed themselves and that were outside the scope of the study. The Page et al.24 study also assessed the most effective session times for mental practice by comparing sessions of 20, 40, and 60minutes. The groups engaging in mental practice showed greater benefits and higher scores, but no differences were observed between groups with different session lengths. These authors conclude that task-oriented therapies are more effective when total mental imagery practice times are longer. Furthermore, patients can perform the technique at home and without supervision.
Not all studies identify positive results. Bovend’Eerdt et al.,42 for example, found that therapists used the technique during less time than required and patients trained to use it did not practice as much as they should have. These authors state that their findings probably reflect insufficient training among therapists, poor selection of patients having sufficient cognitive ability to engage in this practice, or situations in which it was impossible to take time away from conventional therapy. Ietswaart et al.43 found no evidence of the benefits of mental practice alone, but they do consider that physical practice combined with mental practice may be an effective approach. However, it is still not clear whether the benefits of combination treatment are due to improvements in the cognitive models of the movements being performed, motivation mechanisms, or to the indirect effect of mental practice on neuroplasticity. Furthermore, Braun et al.44 analysed the effectiveness of including mental practice within conventional therapy without adding time to the prescheduled daily session, compared to conventional therapy alone. No differences were found between groups. The authors indicate that introducing this therapy in an institution for the elderly is possible but difficult due to the complexity of the intervention. Likewise, a previous study by Braun et al.45 showed that the mental practice protocol was less applicable than was expected, and that this could have been due to lack of experience among therapists. Lastly, Dijkerman et al.46 assessed whether motor imagery training without daily supervision, conducted at the patient's home, could improve motor function of the hand. As a result, the group with motor imagery training showed greater improvement when performing the trained task than was the case for other tasks.
In summary, we can conclude that motor imagery or mental practice is effective when combined with conventional therapy. Rather than taking time away from conventional therapy, it should be supplementary, meaning that total training time should be increased. Likewise, therapists should receive adequate training in this technique and encourage patients to practice it at home without supervision. Furthermore, patients seem to have a positive attitude towards this type of training, which results in good treatment adherence. Regarding dosage, session length should be increased gradually since high levels of attention and concentration are needed. For this reason, patients with CVA should be thoroughly assessed in order to identify those whose mental imagery skills and cognitive level would allow them to benefit from this type of training. Finally, this last requirement may have been responsible for ineffective implementation of this technique in institutions for the elderly, since institutionalised patients are mostly not able to benefit from mental imagery training.
ConclusionsBased on our review, we conclude that motor imagery or mental practice combined with conventional therapy helps patients relearn tasks and transfer the improvements they gain to new environments. It also changes the quality and range of movement of the paretic arm by increasing its functionality and use in activities of daily life. Mental practice also improves spatio-temporal gait parameters, especially when combined with specific techniques, since it reduces fear of falling and promotes earlier retraining of gait. Lastly, applying a mental practice protocol is viable when practice is used as an adjuvant to conventional therapy in patients with preserved imagery skills. Session length should be increased gradually. Mental practice is a safe and low-cost technique which can increase function in patients presenting hemiplegia secondary to stroke. Further studies are needed to identify the type of intervention, the volume of training, and optimal candidates for this therapy.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: García Carrasco D, Aboitiz Cantalapiedra J. Efectividad de la imaginería o práctica mental en la recuperación funcional tras el ictus: revisión sistemática. Neurología. 2016;31:43–52.