Acute hepatic encephalopathy (AHE) is typically characterised by a wide range of neuropsychiatric manifestations including behavioural, cognitive, or mood changes associated with asterixis and different degrees of alteration to the level of consciousness, which may progress to stupor or coma in some cases.1 This situation may be due to acute liver failure, cirrhosis, portal hypertension, or a transjugular intrahepatic portosystemic shunt.2,3 Brain magnetic resonance imaging (MRI) of patients with AHE may reveal signal alterations in different brain areas, caused by vasogenic and cytotoxic oedema related to the toxic effect of ammonia in the brain.4,5 These alterations may disappear after resolution of the encephalopathy,5 or may progress to cortical laminar necrosis in cases with poor outcomes.6 Presentations with focal manifestations are very infrequent in AHE, and may lead to diagnostic errors.
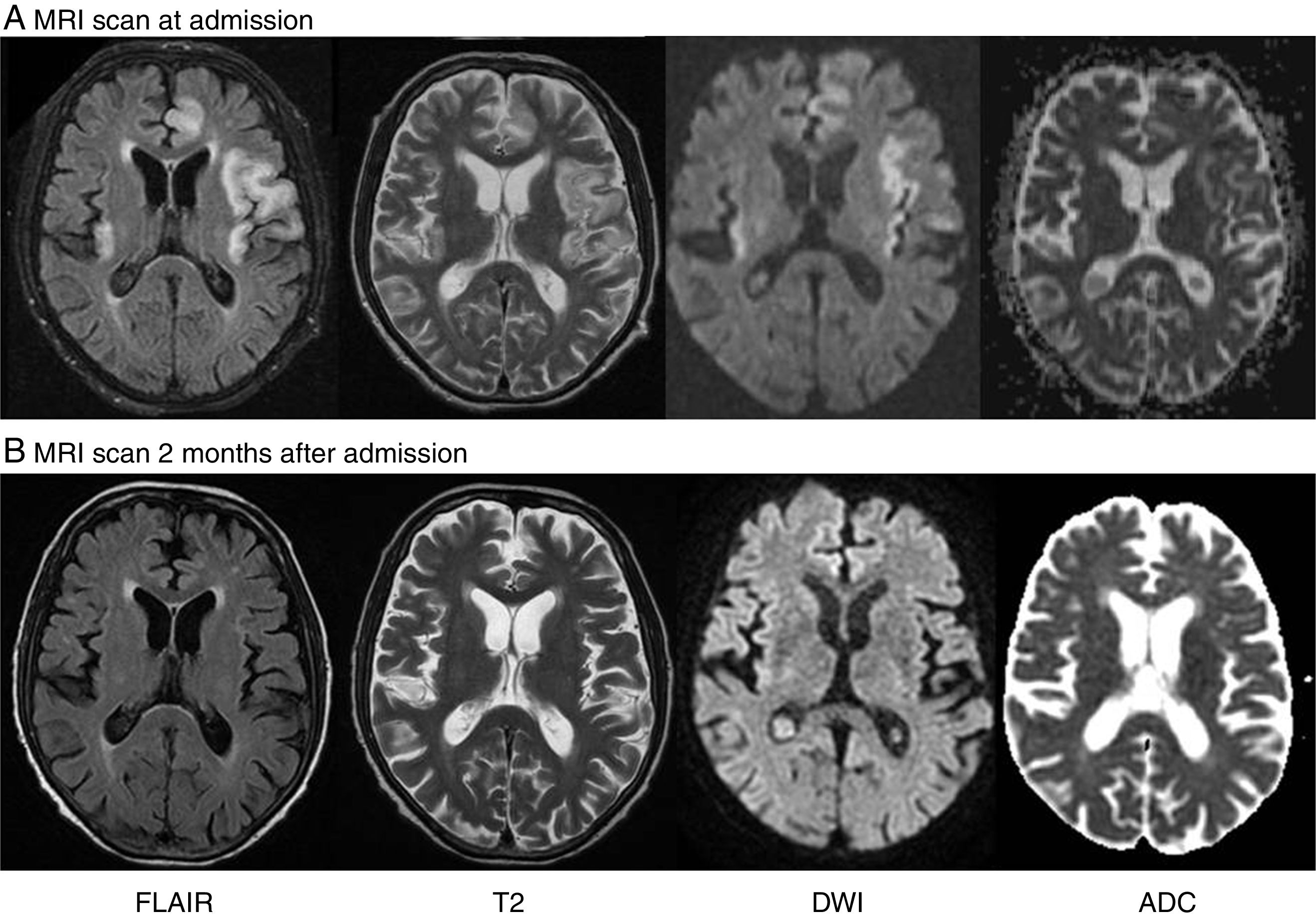
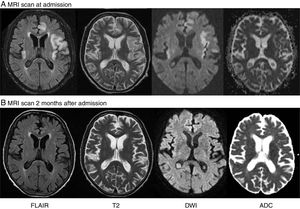
Clinical case. The patient was a 50-year-old man who was diagnosed in 2002 with portal vein thrombosis secondary to protein S deficiency, which was treated with a transjugular intrahepatic portosystemic shunt (TIPS) and oral anticoagulation. He was admitted to another hospital in May 2015 due to a sudden loss of consciousness which progressively and spontaneously improved over the following hours. The patient was transferred to our hospital to rule out the possibility of cerebrovascular accident, since he presented difficulties speaking after recovering a normal level of consciousness. During the neurological examination at admission, the patient was awake and presented mild asterixis in both hands; the most striking finding, however, was the presence of mixed aphasia characterised by hypofluent speech with presence of frequent phonological paraphasias in spontaneous language and difficulty understanding complex commands. Word repetition was preserved, although he showed difficulties repeating simple sentences. The neurological examination yielded otherwise normal results. The blood test revealed chronic anaemia, altered liver profile (ASAT 58IU/L, total bilirubin 3.3mg/dL) and moderately elevated levels of ammonia (91μmol/L). The peritoneal fluid analysis and a brain computed tomography showed no abnormalities. However, the brain MRI showed altered high intensity signal on the fast fluid-attenuated inversion recovery (FLAIR), T2-weighted, and diffusion-weighted imaging (DWI) sequences in the left frontal parasagittal, insular, temporal, and cingulate cortices, as well as the right insular cortex, with no abnormal diffusion restriction in the apparent diffusion coefficient (ADC) map (Fig. 1A). The MR-angiography showed permeability of the intra- and extracranial vessels. An EEG study revealed presence of a delta rhythm with bi- and triphasic waves suggestive of toxic-metabolic dysfunction, with no associated epileptiform activity. We finally diagnosed the patient with acute aphasia as a manifestation of AHE associated with multifocal cortical brain lesions, predominantly involving the left insular and temporal cortices, and in the context of a TIPS. The patient received cathartic therapy, with aphasia progressively improving and resolving several weeks later. An additional MRI scan performed 2 months later showed that the cortical lesions had completely disappeared (Fig. 1B).
(A) Brain MRI revealing cortical and subcortical hyperintensity in both insular areas, the left temporal lobe, and the parasagittal frontal lobe on T2-weighted and FLAIR sequences. DWI showed cortical signal alterations in all these areas, with no abnormal diffusion restriction in the ADC map. (B) A second MRI scan performed 2 months later revealed that lesions had disappeared.
Discussion. Few cases have been described of patients with TIPS who, in the context of AHE, developed focal neurological signs associated with presence of cortical lesions in neuroimaging.7–9 Two of the patients described in the literature presented sudden loss of consciousness with posterior aphasia, with brain MRI scans showing cortical lesions with a similar location to that described in our patient.
Correlation of the level of ammonia with the type of manifestation and the clinical severity of encephalopathy is a controversial issue.10 In our case, as in that reported by Babington et al.7, blood ammonia levels increased only moderately. This suggests that the pathophysiology of these pseudo-ictal discharges may involve factors other than ammonia, such as inflammatory mechanisms or other potential toxins,1,11 the individual susceptibility of the brain to the toxic effect of ammonia, or the rate of increase of ammonia levels in the brain, favoured by TIPS.
Diagnosis of AHE in case of acute focal symptoms in patients with liver disease or TIPS is important since it may have prognostic consequences. It is well known that patients undergoing early, aggressive treatment for AHE have a better prognosis for recovery of neurological deficits and resolution of brain lesions. However, results may not be favourable, with the condition even resulting in the death of the patient, if the aetiology of these lesions is uncertain and treatment is started late.4,8
Conflicts of interestNone.
Please cite this article as: Falgàs N, Alfaro I, Crespo G, Berenguer J, García-Pagán JC, Muñoz E. Afasia en paciente con encefalopatía hepática aguda asociada a lesiones corticales cerebrales multifocales. Neurología. 2018;33:410–412.