Coronavirus disease 2019 (COVID-19), which is caused by infection with the SARS-CoV-2 coronavirus and has caused a global pandemic, presents a wide spectrum of manifestations ranging from asymptomaticity to severe infection causing systemic failure and death. The disease can involve a disproportionate, severe immune response. Immune dysregulation is one of the most widely studied and relevant phenomena in this disease; its effect on the nervous system is currently the main hypothesis proposed to explain neurological damage.
We present the case of a patient with anti–N-methyl-d-aspartate receptor (anti-NMDAR) encephalitis secondary to SARS-CoV-2 infection. Despite the rarity of this case (to our knowledge, it is the first case of this type to be reported), production of anti-NMDAR antibodies may be explained by the antigenic stimulus of the virus, which would trigger the disease.
Our patient was a 30-year-old woman who was admitted to the psychiatry department on 17 March 2020 due to a 3-day history of behaviour disorder characterised by psychomotor agitation, paranoid ideation, dysarthria with dysprosody, and visual hallucinations. A brain CT scan and conventional laboratory tests performed at admission yielded normal results.
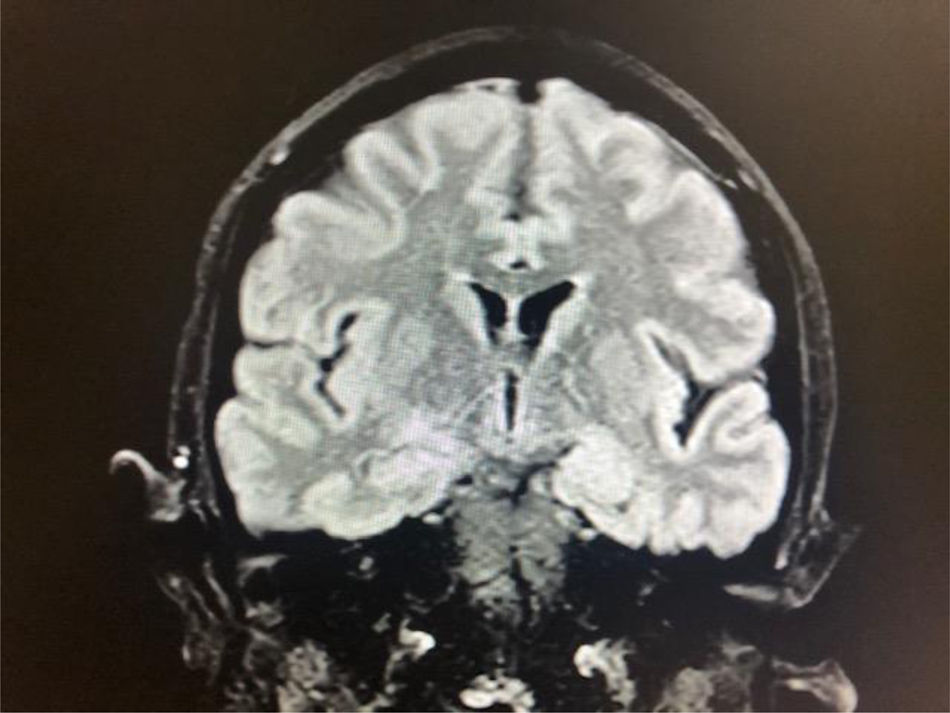
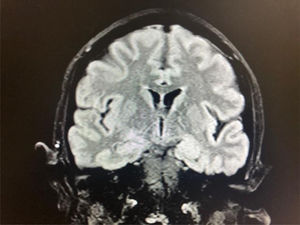
On 20 March 2020, she presented fever, and nasopharyngeal exudate was sampled to test for SARS-CoV-2 infection. Results from the RT-PCR assay were positive for SARS-CoV-2. The chest radiography showed no abnormal findings. The patient was then transferred to the internal medicine department, where treatment was started with hydroxychloroquine and lopinavir/ritonavir. She presented several episodes of focal seizures and some generalised seizures, which led us to perform a lumbar puncture. Cerebrospinal fluid (CSF) analysis revealed high protein levels (54.5 mg/dL) and a predominantly lymphocytic (90%) leukocyte count of 44 cells/µL. An electroencephalography (EEG) revealed epileptic discharges in the left frontotemporal region, and a brain MRI study (Fig. 1) showed hyperintensities in the left hippocampus. PCR testing of the CSF yielded negative results for SARS-CoV-2 and other viruses.
In line with these findings, we started treatment with methylprednisolone and valproate, suspecting anti-NMDAR encephalitis. This working diagnosis was confirmed 2 days later: serum and CSF results for NMDAR antibodies were positive.
Over the following days, we observed a decrease in the patient’s level of consciousness, and she was admitted to the intensive care unit (ICU). A further EEG study showed a delta brush pattern together with spike-and-wave discharges in anterior regions (Appendix, supplementary material). During the patient’s stay at the ICU, we observed buccolingual dyskinesia and choreo-dystonic movements of the right hand. Given the lack of response to the first-line immunomodulatory treatment, we added immunoglobulins to a new 5-day cycle of methylprednisolone. We also withdrew valproate and used lacosamide and perampanel to control epilepsy.
Studies performed to identify the possible paraneoplastic origin of anti-NMDAR encephalitis detected a left ovarian teratoma, which was removed by laparotomy. The abnormal movements and delta brush EEG pattern (Appendix, supplementary material) persisted despite immune therapy and resection of the teratoma.
During her stay at the ICU, the patient presented such complications as hypovolaemic shock and post-surgical intra-abdominal infection, as well as pneumonia, thrombosis of the left iliac vein, and bilateral pulmonary embolism attributed to SARS-CoV-2 infection. Neurological status remained unchanged, with the delta brush pattern persisting in a subsequent EEG (Appendix, supplementary material).
She was transferred from the ICU to the neurology ward a month later, when systemic and respiratory symptoms had stabilised. There, she presented generalised choreo-dystonic movements, blepharoclonus, and focal seizures (Appendix, supplementary material) that progressively improved when rituximab, benzodiazepines, and olanzapine were added to treatment. Rituximab had not previously been used due to the concomitant SARS-CoV-2 infection.
On 29 May, she was discharged from hospital with cognitive sequelae such as hypoprosexia, emotional lability, and memory disorder, and enrolled in an intensive neurorehabilitation programme.
Anti-NMDAR encephalitis is one of the most frequent types of autoimmune encephalitis; its clinical presentation is characterised by simultaneous onset of neurological and psychiatric symptoms. It usually manifests at earlier ages in patients with underlying neoplasia.1 Early detection, immune therapy, and the study to determine malignancy are essential in the management of the condition.2
Confirmed trigger factors for anti-NMDAR encephalitis are tumours and herpes simplex encephalitis.1,2 Two studies have suggested a possible association between the HLA class I allele B*07:02 and the HLA class II allele DRB1*16:0.3 In this case, we suspect that SARS-CoV-2 infection acted as a trigger for the onset of anti-NMDAR encephalitis.
COVID-19 has been characterised as a progressive condition with overlapping stages. Firstly, there is a viral stage, which is thought to be asymptomatic or mild in 80% of patients. In the remaining 20% of cases, the disease may be severe or critical. Most of the patients in this group present a second stage characterised by hyperreactivity of the immune system. The third stage corresponds to a state of hypercoagulability. Finally, the fourth stage is characterised by multi-organ lesions and failure.4,5 Identifying autoimmune phenomena in patients with COVID-19 has enabled us to detect some immune-mediated neurological conditions, such as Guillain-Barré syndrome, acute necrotising encephalitis, myelitis, limbic encephalitis, and multiple cranial neuropathy associated with SARS-CoV-2 infection.6–8
This case illustrates the slow clinical progression of a patient with anti-NMDAR encephalitis and COVID-19. We assume that the loss of immune regulation secondary to SARS-CoV-2 infection may contribute to perpetuate autoimmunity, even though all therapeutic decisions were made opportunely. To our knowledge, this is the first case of anti-NMDAR encephalitis associated with COVID-19.
Please cite this article as: Alvarez Bravo G, Ramió i Torrentà L. Encefalitis anti-NMDA-R secundaria a infección por SARSCoV- 2. Neurología. 2020;35:699–700.