Introduction
The presence of foreign bodies (FBs) in soft tissues of the upper extremity is a common and challenging situation in clinical practice. Sometimes the foreign body is partially visible or palpated, being relatively easy to locate and extract them. However, is not infrequent that the FBs are located deep into the subcutaneous tissue or too small to be palpated requiring surgical procedures to locate and extract them. In this situation, physicians are often in a dilemma as to whether to attempt to extract the FB or to observe and perform the surgery only if a complication or symptoms are observed.
Foreign bodies can mimic tumors,1,2 migrate and cause significant morbidity3,4 cause acute and chronic pain5, infections and limitation of daily activities. In fact, there have been reports of pseudoaneurysms6 and life-threatening infections secondary to FBs,4 making reasonably to try to extract them when possible.
In recent years, different imaging modalities have been used to localize FBs in soft tissues including computed tomography (CT),7 microwave-induced thermoacustic tomography8 and different modalities of ultrasound (US).9-11 The US has become the preferred diagnostic modality for these situations10 due to its reliability and sensibility to detect and facilitate the extraction of both radiolucent and radiopaque materials.9,10 However, US is not always available and in some situations radiographs are the only option to detect and localize FBs (e.g. rural areas or developing countries).
Radiographs are useful to locate radiopaque FBs and have been used to guide surgeons to locate and remove them.12,13 Different and ingenious techniques have been used by physicians who only have plain radiographs for these situations obtaining variable rates of success (personal communications).
Objective
To present a simple and reliable technique to effectively localize and remove radiopaque FBs in soft tissues using X-rays.
Methods
Patients: All patients with radiopaque FBs in soft tissues of the upper extremities received in our service in the period of April 2005 to September 2008 were included in the study. All patients agreed to participate in the study and signed informed consent.
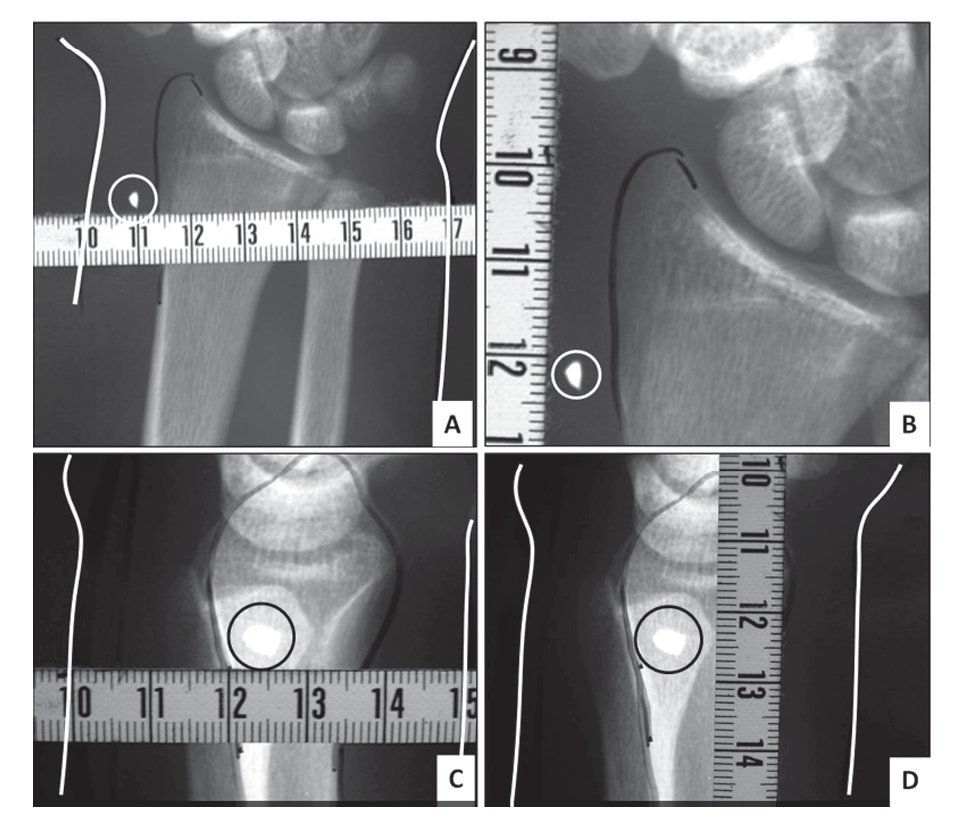
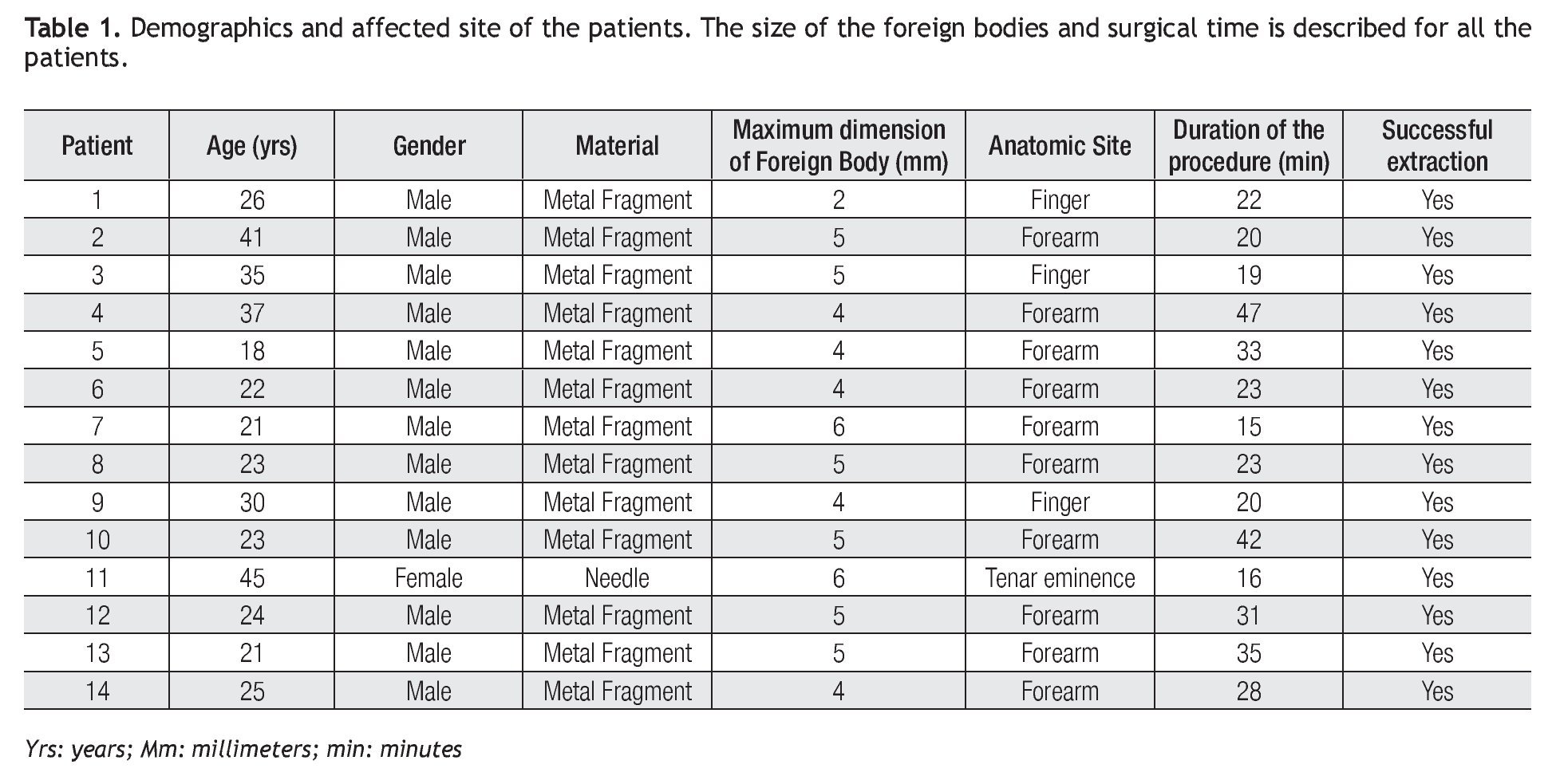
Radiographs: Plain radiographs of the affected area in antero-posterior (AP) and lateral views were obtained for every patient. The distance from the foreign body to an adjacent palpable osseous reference (e.g. joint, bony prominence) was obtained in the radiographs. Additionally, the distance from the interface between soft tissues and air (i.e. skin) to the FB was also obtained (Figure 1).
Figure 1.Radiographs marking. The distance from a palpable osseous reference to the object is measured in antero-posterior and lateral views. A and B show the measurements in the antero-posterior view. C and D show the measurement in the lateral view. The white line demarks the skin. The palpable osseous reference is outlined in black. The foreign body is encircled.
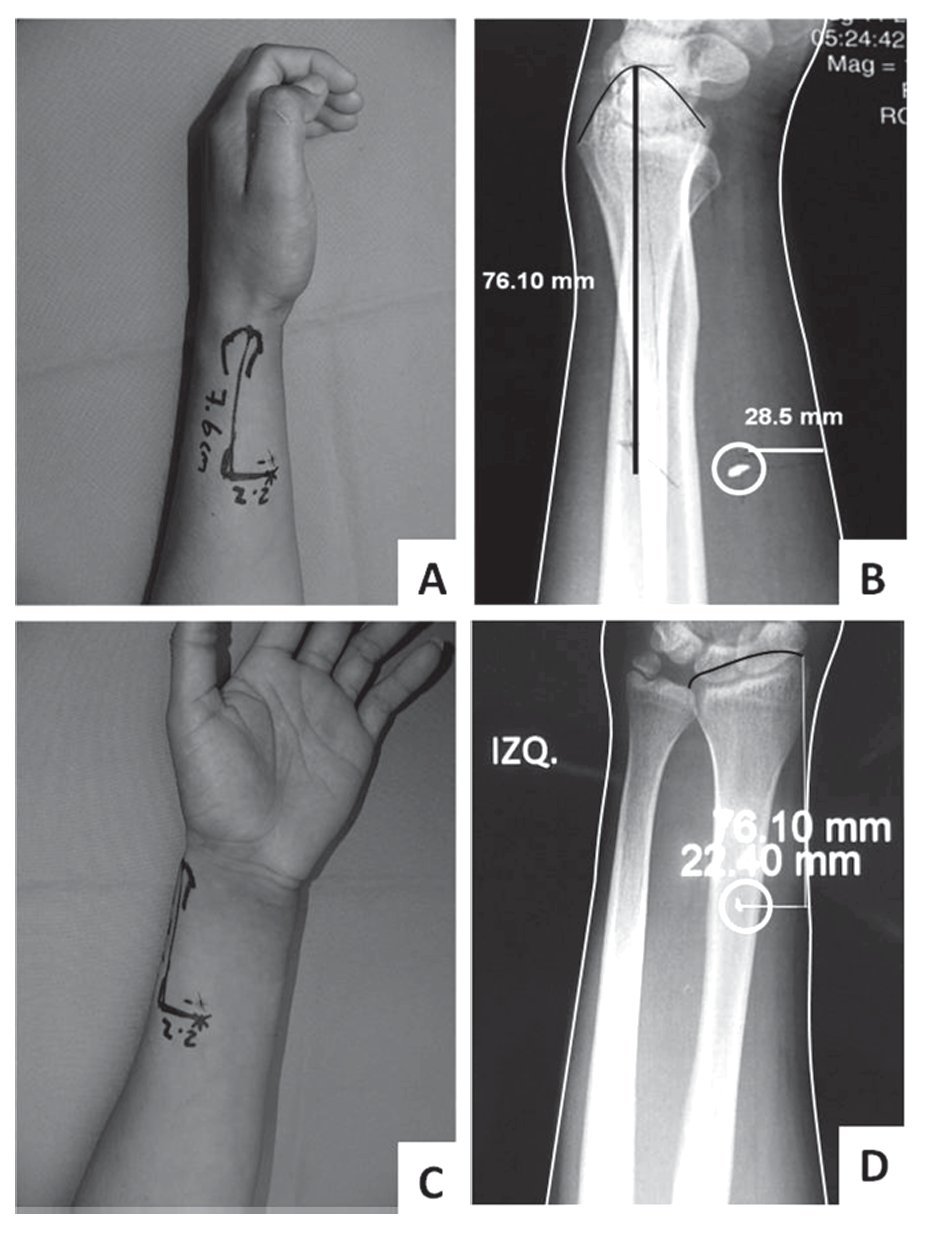
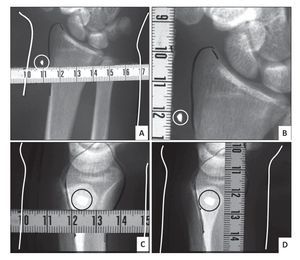
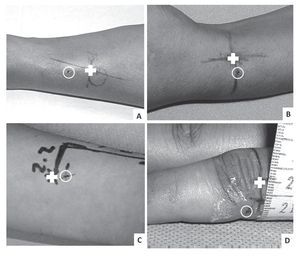
Patient Marking: The selected osseous reference was located by palpation and the obtained distance from this reference to the FB (obtained in the radiographs) was marked in the patient in AP and lateral aspects of the affected area (Figure 2). This point determined the site of the incision.
Figure 2.Patient marking. The patient is marked following the markings in the radiographs. A: marking in the lateral view. B: Distances obtained in the radiographs. C and D show the marking on the skin based on the radiograph in the Antero-posterior view.
Location and extraction: The skin was prepared with standard surgical-protocols of asepsis. Local anesthesia with 2% Lidocaine and 1:200 000 epinephrine was infiltrated in the marked site. A 2 cm incision in the determined site was performed according to the lines of minimal tension and the depth of the incision was made according to the observed depth in the radiographs. The foreign body was located and extracted using blunt dissection. After hemostasis the wounds were closed with Vicryl® 4-0 for deep tissues and 5-0 nylon for skin. The wound was covered with Neosporin® and the patient was seen at 7 - 10 days for stitch removal. The time of the entire surgical procedure (from incision to closure) was recorded.
Results
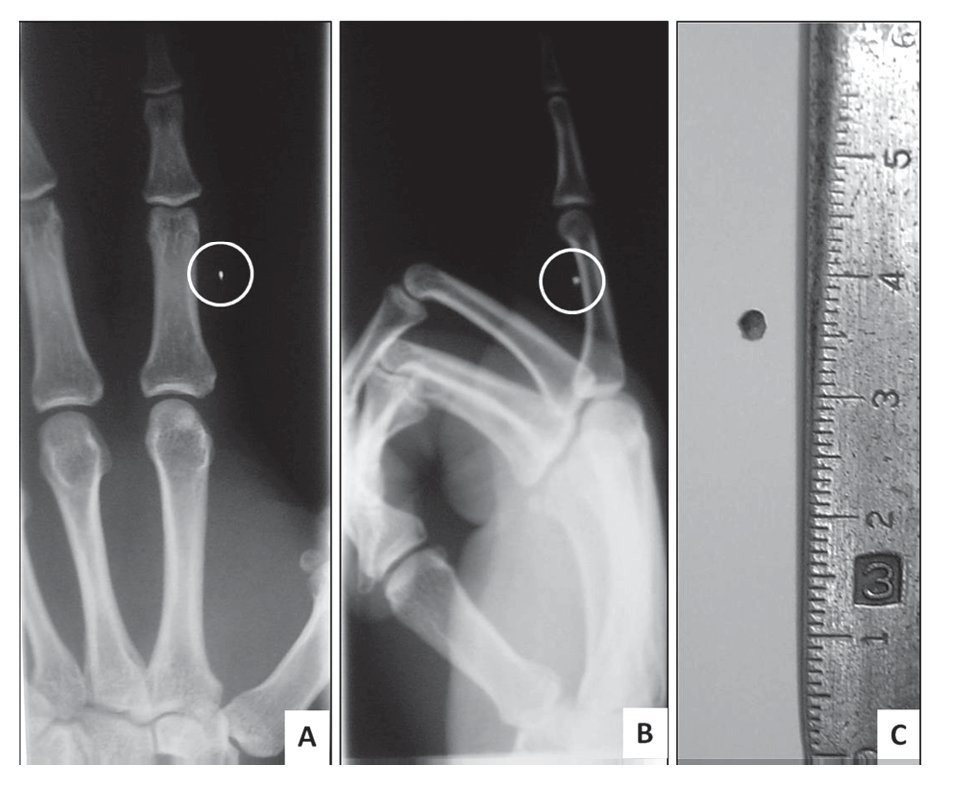
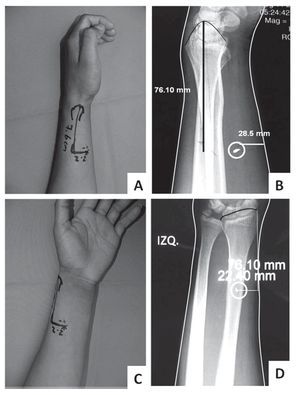
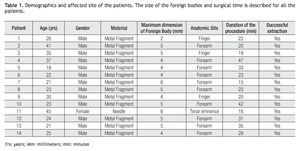
Fourteen consecutive patients with radiopaque FBs were included in the protocol. All patients agreed to participate in the study and there were no exclusions. All foreign bodies were localized and extracted. The mean age of the patients was 28 ± 8 years. Male patients were more frequent in a proportion of 6:1 compared to females. Most of the FBs were metal fragments released while hammering metal (85%) and the rest were needle fragments (15%). All FBs were extracted through the 2 cm incision. Average surgical time was 26 ± 9 minutes. The mean size of the fragments was 4.5 mm ± 1 mm, being the smallest fragment only 2 mm of diameter (Figure 3). Table 1 shows the data of the patients.
Figure 3.Foreign body in a finger. A 2 mm foreign body was successfully located and extracted using the described technique. A: Antero-posterior view. B: Lateral View. C: Foreign body.
One patient had a lesion of the sensitive branch of the radial nerve that was repaired after the extraction of the FB. There were no complications related to the procedure. All patients returned to normal activities within a week.
Discussion
For many years, plain radiographs were the only option to detect FBs. However, it is not possible to detect radiolucent materials with radiographs making clear that a more sensitive diagnostic method was required. In recent years, ultrasound has been shown to be better to detect retained FBs in soft tissues14-17 and is becoming the preferred diagnostic modality for these situations. However,US is not available in all facilities, and it is often required to refer the patient to another center.
In remote areas of developing countries the radiographs are perhaps the only available diagnostic tool for physicians. Patients from these areas have to be referred to nearest cities and even there plain radiographs might be the only diagnostic option. We have received patients in our facility that had to travel for at least 6 h to our hospital, referred from small clinics after failed removal of FBs.
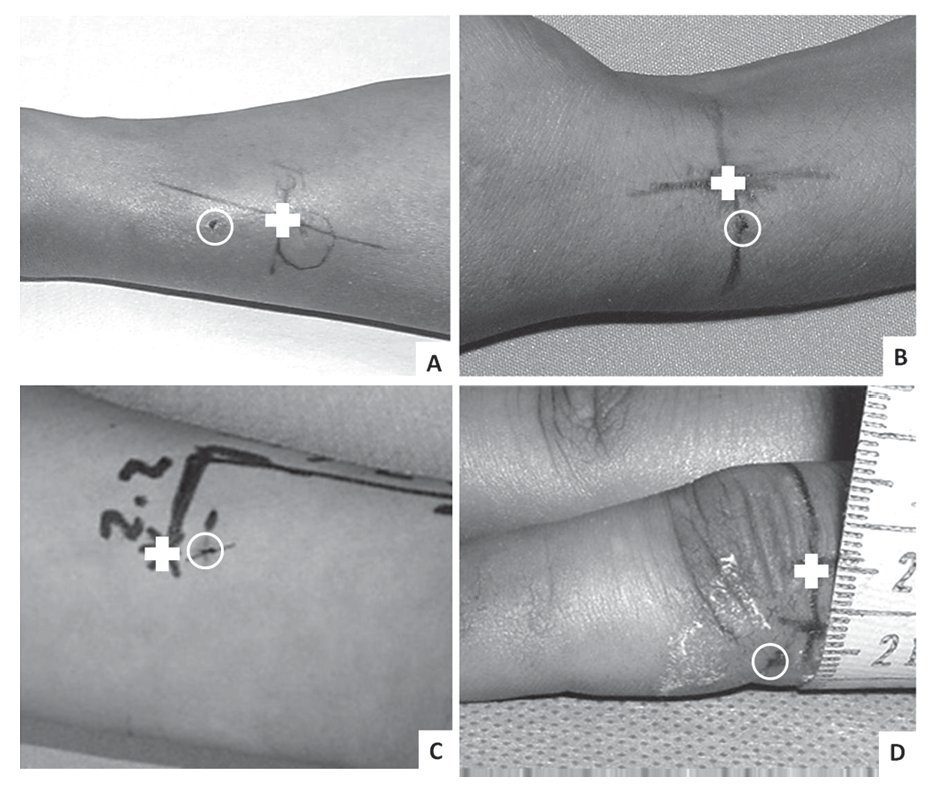
In a recently published article, Tuncer et al emphasize the utility and feasibility of plain radiographs for soft tissues in the hand.12 In their article they included patients with glass fragments in the hand of 26 patients. In our series of 14 consecutive patients we did not have patients with retained glass fragments and most of them were located in the forearm (Table 1). This might have been secondary to the fact that most patients received in our service are stable patients seeking for attention after a work-related injury. Accidents related with broken glass are usually seen in emergency room and X-rays of the hand are always obtained, helping the location and removal of them through the wound. We believe that planning the correct site of the incision is important for successful extractions of FBs. Inexperienced physicians usually make the incisions in the site where the FB penetrated the skin, but sometimes the foreign body is centimeters away from this site making very difficult to extract them (Figure 4). This might be due to migration or deep penetration of the object that behaves as a projectile when is released. One of the patients in the study had a needle in the tenar eminence with the puncture (entry site) located almost in the wrist. The local physician tried to remove the needle extending the incision up to 3 cm without success. We found the needle 4 cm distal to the entry point and removed it by incising the palm in the correct point after the described protocol. This migration might have been caused by inadvertent push of the needle when trying to locate it, which is a frequent complication when trying to locate them through the entry site. We feel that is easier to locate the middle point of the needle and incise right over this area, having more surface of the needle in the plane of the dissection than trying to locate them from behind.
Figure 4.The actual location of the foreign body (FB) can be distant from the entry mark in the skin. The white circle shows the entry site of the foreign body. The white cross indicates the location of the FB as determined by using the described technique. The incision was planned in this site and not in the entry point
Standard radiographs provide images with practically actual measurements (scale 1:1), making possible to measure the distance from the FB to a palpable reference and then measure it on the surface. Theoretically, there might be some discrepancy from the actual measurements to the obtained ones in radiographs, but they would be a few millimeters and still be located within the surgical field. It is important to measure the depth of the FB in radiographs to have a good idea of the actual depth of the FB in the patient. It is not uncommon that the surgeon makes an incision in the site of the puncture and blindly dissects the tissues with scissors from superficial to deep, trying to find the foreign body. This creates more damage to the tissues and edema in sites potentially distant from the site where the FBs actually is. By using this technique, we can limit blind dissection from superficial to deep tissues and we would have fewer chances to push the FB away from the surgical field.
There are different options besides the radiographs to detect radiopaque FBs with proved efficacy. Young and cols. demonstrated the effectiveness of US and fluoroscopy to localize FBs allowing successful removal of 68 FBs. The size of the FBs ranged from 2.5mm - 160.0 mm and of the incisions from 4 mm to 6 mm.18 We were able to remove FBs measuring 2 to 6 mm through a 2 cm incision, demonstrating that plain radiographs are as effective as US and fluoroscopy for these purposes.
We cannot overemphasize that we our aim is not to prove that X rays are superior to US for detection of radiopaque FBs. Instead, we want to prove that plain radiographs are useful and reliable for detection and removal of very small FBs in soft tissues.
The described technique is a simple and effective method to locate and extract radiopaque foreign bodies located in soft tissues of the upper extremities. We propose this technique for those situations where radiographs are the only available tool to locate them.
Corresponding author: Gabriel Ángel Mecott.
Madero y Gonzalitos S/N Col. Mitras Centro, Monterrey, N.L. México. CP.64460.
Telephone: (+52) 8183476117, Fax: (+52) 8183476117.
E-mail:gmecott@hospitaluniversitario.org.
Recibido: Febrero 2011.
Aceptado: Abril 2011