Lemierre's syndrome is a rare form of severe sepsis secondary to oropharyngeal infection characterized by septic thrombophlebitis of the internal jugular vein with disseminated infections, with the lungs being the most frequent target. We report the case of a previously healthy 15-year-old admitted to the intensive care unit because of septic shock, brain and lung abscesses, and a positive blood culture for Prevotella oris with a clinical presentation compatible with the diagnosis of Lemierre's syndrome.
ConclusionThis is an atypical presentation of Lemierre's syndrome because of the isolated microorganism.
Lemierre's syndrome, also known as postanginal septicemia or necrobacillosis, is a rare form of severe sepsis secondary to oropharyngeal infection. It is characterized by oropharyngeal infection, as well as a disseminated infection, in most cases to the lung and internal jugular vein, causing septic thrombophlebitis.1 Lemierre's syndrome was first described in the 1900s by Courmont and Cade. However, it was better characterized by André Lemierre in 1936. The syndrome was common before the development of antibiotics and was rapidly progressive and fatal in the first 7 to 15 days from the onset of the disease.2
Lemierre's syndrome is most commonly caused by Fusobacterium necrophorum. It generally affects males at a ratio of 2:1, mostly previously being healthy teenagers and young adults. It is secondary to an upper airway infection, commonly tonsillitis. However, it has also been described in pharyngeal, middle ear, paranasal sinus, parotid gland, and dental infections.3,4 Common symptoms include persistent fever, shivering, dysphagia, coughing, hemoptysis, dyspnea, arthralgias, malaise, vomiting, occasionally hyperbilirubinemia, mild jaundice, and elevated liver enzymes.5 Patients present ipsilateral internal jugular vein thrombosis in 30%–40% of cases, and also pulmonary nodular lesions, empyema, arthralgia or septic arthritis.6
We describe the case of a male with an atypical presentation of Lemierre's syndrome caused by Prevotella oris.
Case reportThe patient is a 15-year-old male whose symptoms began 3 days before hospitalization with headache, hyporexia, unquantified fever, nausea and vomiting. Twenty-four hours later, he presented drowsiness, right periorbital edema and hemoptysis. Because of these symptoms, he was taken to the pediatrics emergency room. The patient had a relevant history which accounted for a left petrous temporal bone fracture 6 months ago and a pharyngeal infection without treatment 3 weeks before admission. He had two tattoos and there was a high degree of suspicion of illicit drug consumption. The rest of the interview was unremarkable.
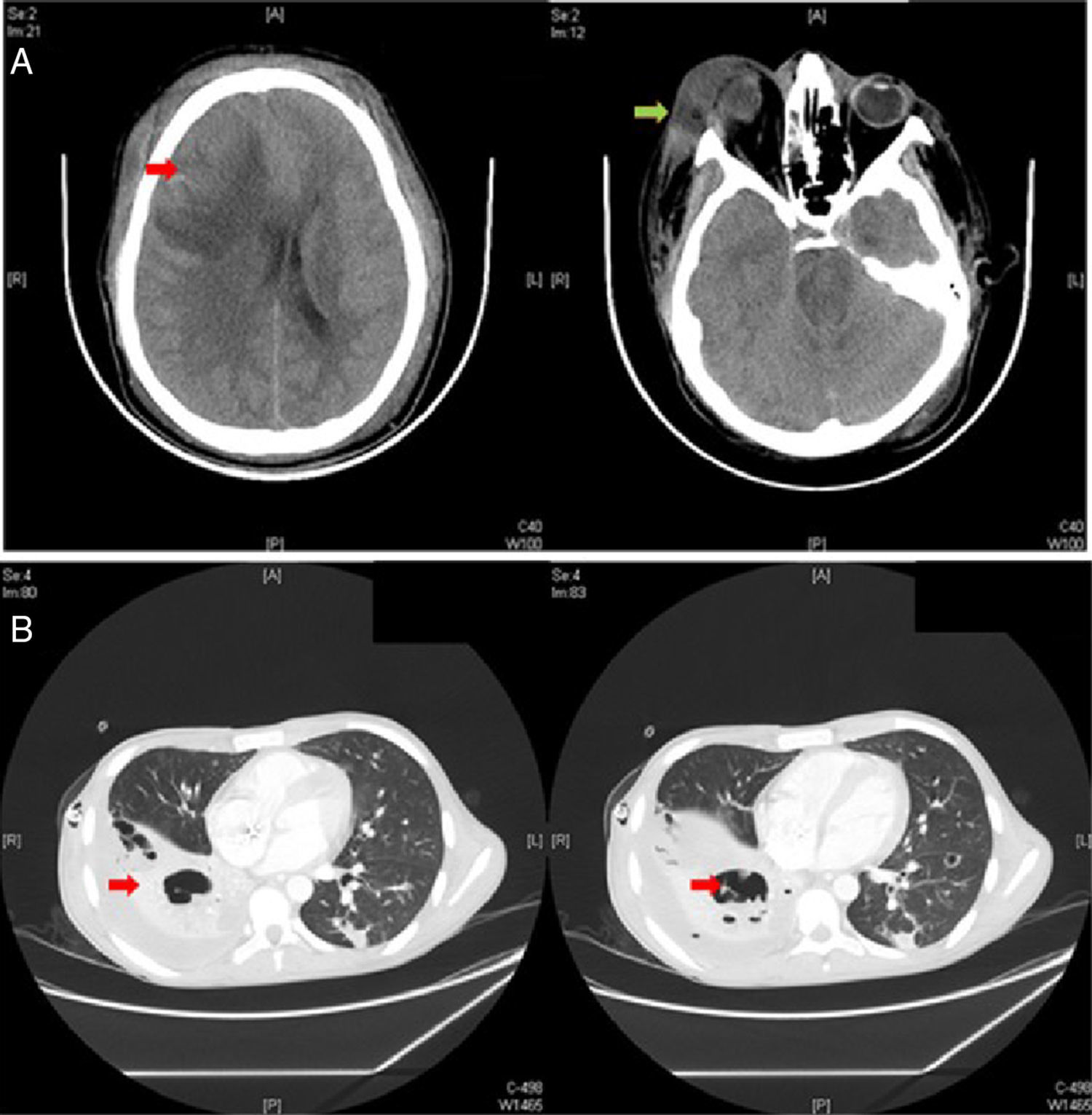
To search for neuroinfection, a brain CT was performed, revealing a right frontoparietal mass and brain edema, midline deviation and ventricular collapse (Fig. 1A). Furthermore, a contrasted MRI of the brain showed a matching image with a brain abscess, ethmoid and maxillary sinusitis and coronary sinus thrombosis, which were subsequently discarded on a brain angiotomography.
(A) Brain CT, revealing a right frontoparietal mass with brain edema (red arrow), midline deviation and ventricular collapse. The right periorbital edema is also observed together with ipsilateral periorbital cellulite (green arrow). (B) Chest contrast CT, where a right pleural effusion (red arrow, left) and a mild bilateral pulmonary parenchymal infiltrate and cavitation (red arrow, right) are observed. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
During the first 48h after admission, the patient developed septic shock, progressing to disseminated intravascular coagulation and multiple organ failure. Laboratory tests showed leukocytosis 14,400cells/μL, neutrophils 75%, bands 13%, platelets 4470μL−1, CRP 28.9mg/dL, creatinine 1.6mg/dL, BUN 79mg/dL, total proteins 4.4g/dL, albumin 2.2g/dL, AST 102IU/L, ALT 31IU/L, total bilirubin 13.8mg/dL, direct bilirubin 9.2mg/dL and indirect bilirubin 4.6mg/dL, which prolonged clotting time. Anti-HIV-1 and anti-HIV-2 antibodies, anti-hepatitis B and anti-hepatitis C antibodies were negative. A chest X-ray showed bibasal infiltrates. Due to the neurological deterioration, respiratory distress, and septic shock, he was transferred to the Pediatric Intensive Care Unit. He was started on mechanical ventilation and an empiric triple antibiotic therapy with ceftriaxone, metronidazole and vancomicin.
In the PICU (Pediatric Intensive Care Unit), beside the inotropic support, he presented a fever of 40.5°C and developed right pleural effusion. A thoracocentesis was performed, obtaining a black-brown fluid that was positive for Gram-negative bacilli on culture. Subsequently, he presented skin and soft tissue necrotic lesions suggesting septic embolism (Fig. 2).
On his 7th day in the PICU an emergency decompressive craniotomy was performed because of intracranial hypertension as well as brain abscess drainage. Then a contrasted CT chest scan was performed revealing several bilateral abscesses and pulmonary cavities in both lungs (Fig. 1B).
P. oris was reported on the admission blood culture and on the thoracocentesis pleural effusion culture. The susceptible antibiotic scheme performed consisted of penicillin G sodium, metronidazole and ciprofloxacin.
A Doppler ultrasound of the neck was performed to corroborate the clinical suspicion of Lemierre's syndrome; thrombophlebitis of the left jugular vein was detected. With this constellation of data the diagnosis was complete.
Regarding the evolution of our patient, he was admitted to the operating room again for a right lower lung lobectomy because of persisting empyema in addition to drainage of a right periorbitary abscess. After 6 days he was afebrile with no evidence of a systemic inflammatory response and he was discharged from the PICU. An antibiotic scheme of cefepime and metronidazole was continued for 4 weeks. The patient remained hospitalized for 2 weeks for the management of neurological symptoms and was later discharged from the hospital 6 weeks after admission with hematological recovery and without sequelae.
DiscussionThis case was an atypical presentation of Lemierre's syndrome because of the isolated microorganism. Lemierre's syndrome is a rare disease characterized by a history of oropharyngeal infection, Fusobacterium septicemia, disseminated infection, and clinical or radiological evidence of internal jugular vein thrombosis or supurative thrombophlebitis.1–9 However, evidence of thrombophlebitis or vein thrombosis is not an absolute requirement for diagnosis.8
P. oris was isolated in our case by blood culture. Prevotella are strict anaerobic unsporulated bacilli, members of the Bacteroidaceae family, which are classified as pigmented and non-pigmented. These bacteria are part of the normal oral flora and have been associated with the development of brain and lung abscesses. The gingival sulcus is the primary habitat of Prevotella in the oral cavity. Some virulence mechanisms of the microorganism are the presence of fimbriae and adhesins, its capacity to degrade immunoglobulins, its toxic action on fibroblastes, and its fibrinolytic and inhibitory action on B cells.7
This patient had a history of a pharyngeal infection and a clinical picture compatible with Lemierre's syndrome, since he had a positive culture for an anaerobic infection, multiple abscesses, and necrotic lesions in the skin and soft tissues that suggested septic embolism, evidence of a disseminated infection.
F. necrophorum, a commensal of the oral cavity, gastrointestinal and urogenital tract, is the most commonly associated pathogen, although others such as Fusobacterium nucleatum, Eikenella corrodens, Porphyromonas asacharolytica, Streptococcus pyogenes, Bacteroides and anaerobic streptococci have been involved.10 There are also isolated reports of Lemierre's syndrome caused by Staphylococcus spp.10 To our knowledge this is the first case in which P. oris was present.
In the pre-antibiotic era, necrobacillosis was a frequent complication of pharyngitis and was unavoidably associated with a poor prognosis (90% to 100% mortality). After the introduction of β-lactam antibiotics, the incidence was reduced to 0.8–1.5 cases per million per year. However, it remains a potentially dangerous condition, with an estimated mortality rate of around 15%, despite antibiotic therapy.1,2,8
The diagnosis of Lemierre's syndrome is mainly based on identification of the causal microorganism in one or more blood cultures. Nevertheless, early detection and treatment depend largely on clinical suspicion of the disease. Although penicillin remains the treatment of choice in most cases, cephalosporin, metronidazole or clindamycin can be used as first-line antibiotics because of the emergence of penicillin-resistant strains.8,9 Therapy is generally administered parenterally for a 2 week period, and later orally for a total duration of 6 weeks. Surgical drainage of an abscess is often indicated in patients who do not respond to antibiotic therapy.9
Lemierre's syndrome is currently a rare entity with a high mortality rate if not identified and treated promptly. It is important to know the disease, and have high clinical suspicion for early diagnosis and treatment to avoid complications.
Conflict of interestThe authors have no conflicts of interest to declare.
FundingNo financial support was provided.
We thank Angel Martinez-Ponce de Leon, M.D. and Jose Luis Treviño-Gonzalez, M.D. for their support and help and Sergio Lozano-Rodriguez, M.D. for helping with the manuscript.