To analyze the effect of sodium glucose cotransporter 2 (SGLT2) inhibitors in a group of insulin-dependent type 2 diabetes mellitus (T2D) patients.
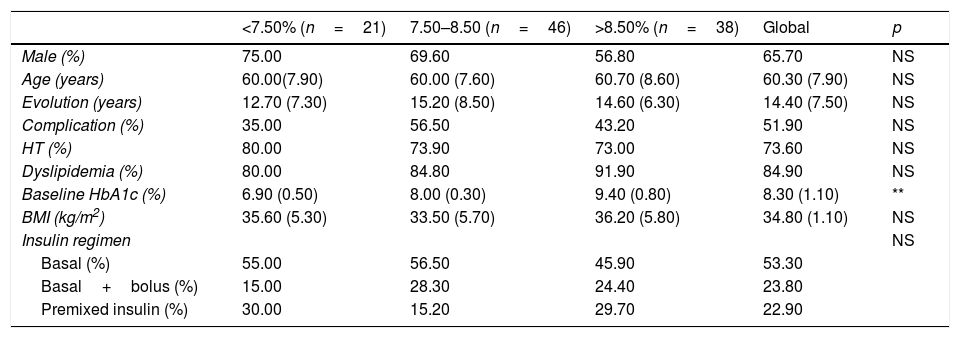
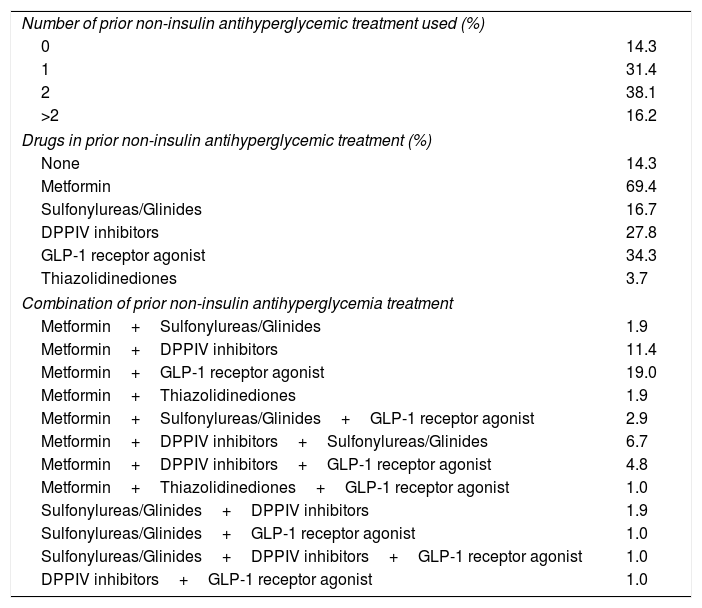
Patients and methodsOne hundred and five insulin treated T2D patients were enrolled. Primary endpoints were: fasting plasma glucose, HbA1c, weight, total insulin doses (TDI), total basal insulin (TDB) and total rapid insulin (TDR). Secondary variables were: total cholesterol, LDL cholesterol (cLDL), HDL cholesterol (cHDL), triglycerides and systolic (SBP) and diastolic (DBP) blood pressure. Safety and tolerance were evaluated through the appearance of severe hypoglycemia, ketoacidosis and infections.
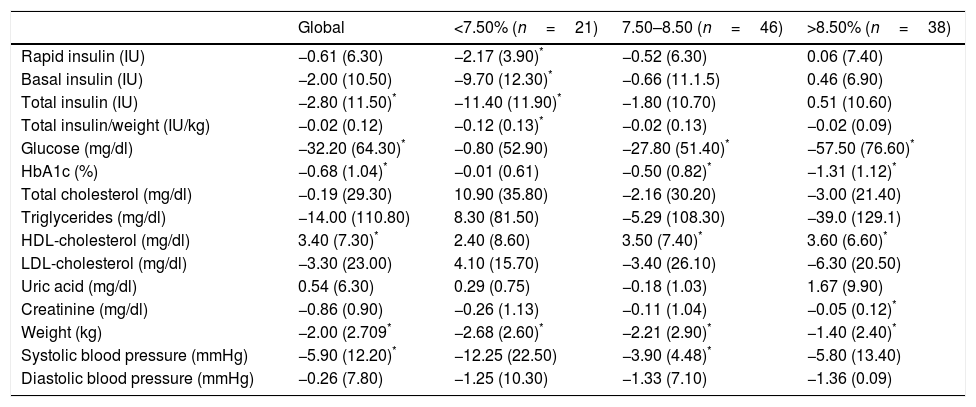
ResultsAfter 4 months follow-up, a 0.7 (1.0)% HbA1c reduction was found, accompanied by a −2.8 (11.5) UI/day TDI decrease. Weight dropped for 73.7% of patients, with an average −2.0 (2.7) kg reduction. A global cHDL increase was noted after treatment, while no differences were observed for total cholesterol, triglycerides or cLDL. SBP dropped significantly, but no change in DBP was observed.
ConclusionThe use of SGLT2 inhibitors in insulin treated T2D patients resulted in reduction of HbA1c, which was associated to weight loss, cHDL increase and SBP decrease.
Analizar el efecto de los inhibidores del cotransportador sodio glucosa tipo 2 (iSGLT2) en grupo de pacientes con diabetes mellitus tipo 2 (DM2) tratados con insulina.
Pacientes y métodosSeleccionamos ciento cinco pacientes con diabetes tipo 2 tratados con insulina. Los objetivos primarios: glucosa plasmática ayunas, HbA1c, peso, dosis total de insulina (DTI), dosis de insulina basal (DTB), dosis de insulina rápida (DTR). Como secundarios: Colesterol total, LDL colesterol (cLDL), HDL colesterol (cHDL), triglicéridos and tensión sistólica (TAS) and diastólica (TAD). La seguridad y tolerancia se valoró como hipoglucemia, cetoacidosis o infecciones.
ResultadosTras 4 meses, la HbA1c se redujo en 0,7 (1,0)% acompañado de una disminución en DTI de −2,8 (11,5) UI/día. El 73,7% de los pacientes perdieron peso, con un descenso medio de −2,0 (2,7) kg. El cHDL aumentó, mientras que no observamos diferencias en el colesterol total, triglicéridos o cLDL. TAS disminuyó significativamente sin observar cambios en TAD.
ConclusiónEl uso de iSGLT2 en pacientes con DM2 tratados con insulina reduce la HbA1c asociando pérdida de peso, aumento enl cHDL y descenso en TAS.