To evaluate the impact of a code sepsis (CS) activation, complying with recommendations, the evolution of patients with severe sepsis in the emergency room and determine independent factors associated to mortality.
MethodAll patients attending the emergency room with severe sepsis during a 6-month period were included. Complying with Surviving Sepsis Campaign recommendations, patients’ average stay, intensive care admissions and 30-day mortality were assessed. Two groups were compared: CS activation (A) and no activation (NA).
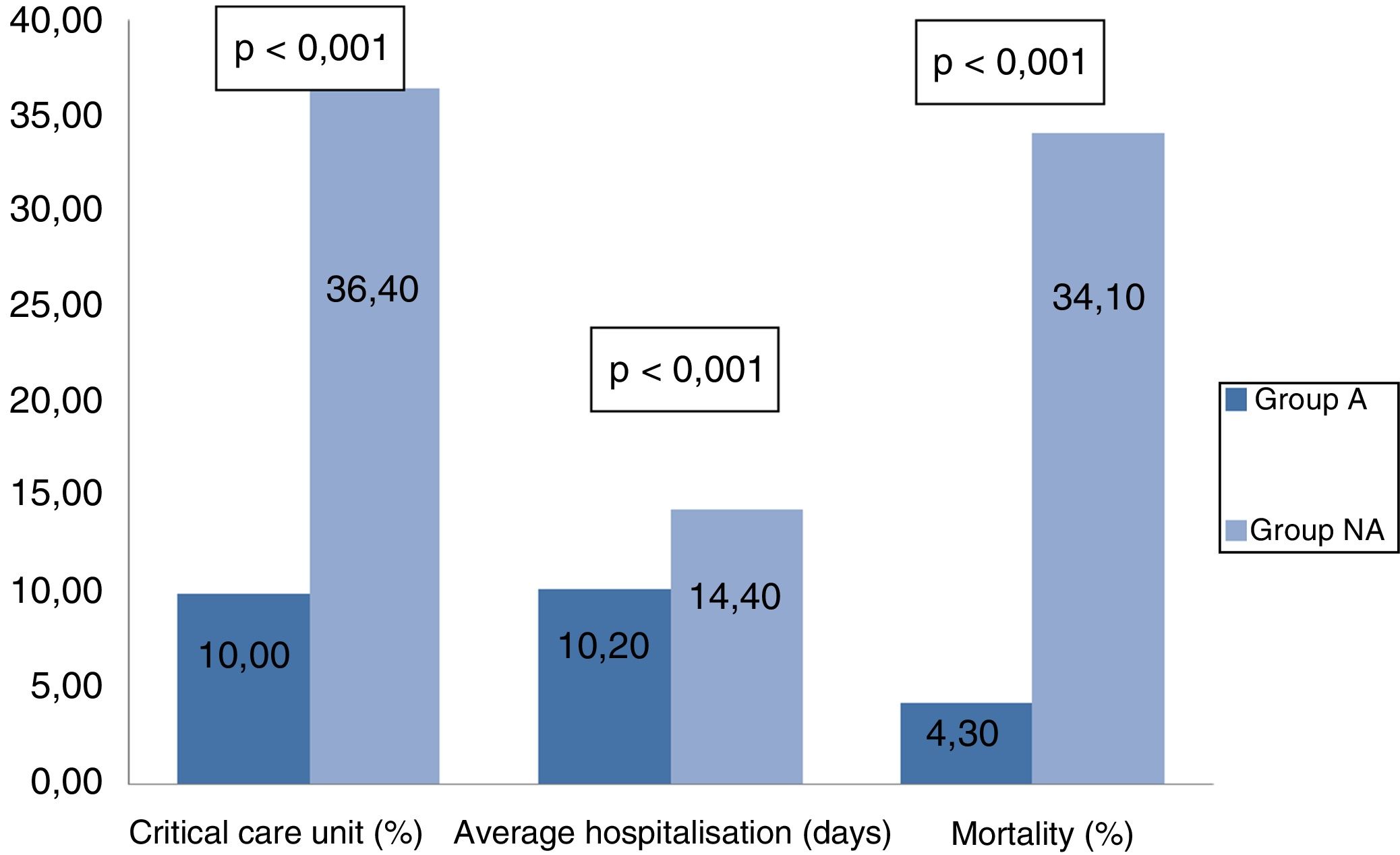
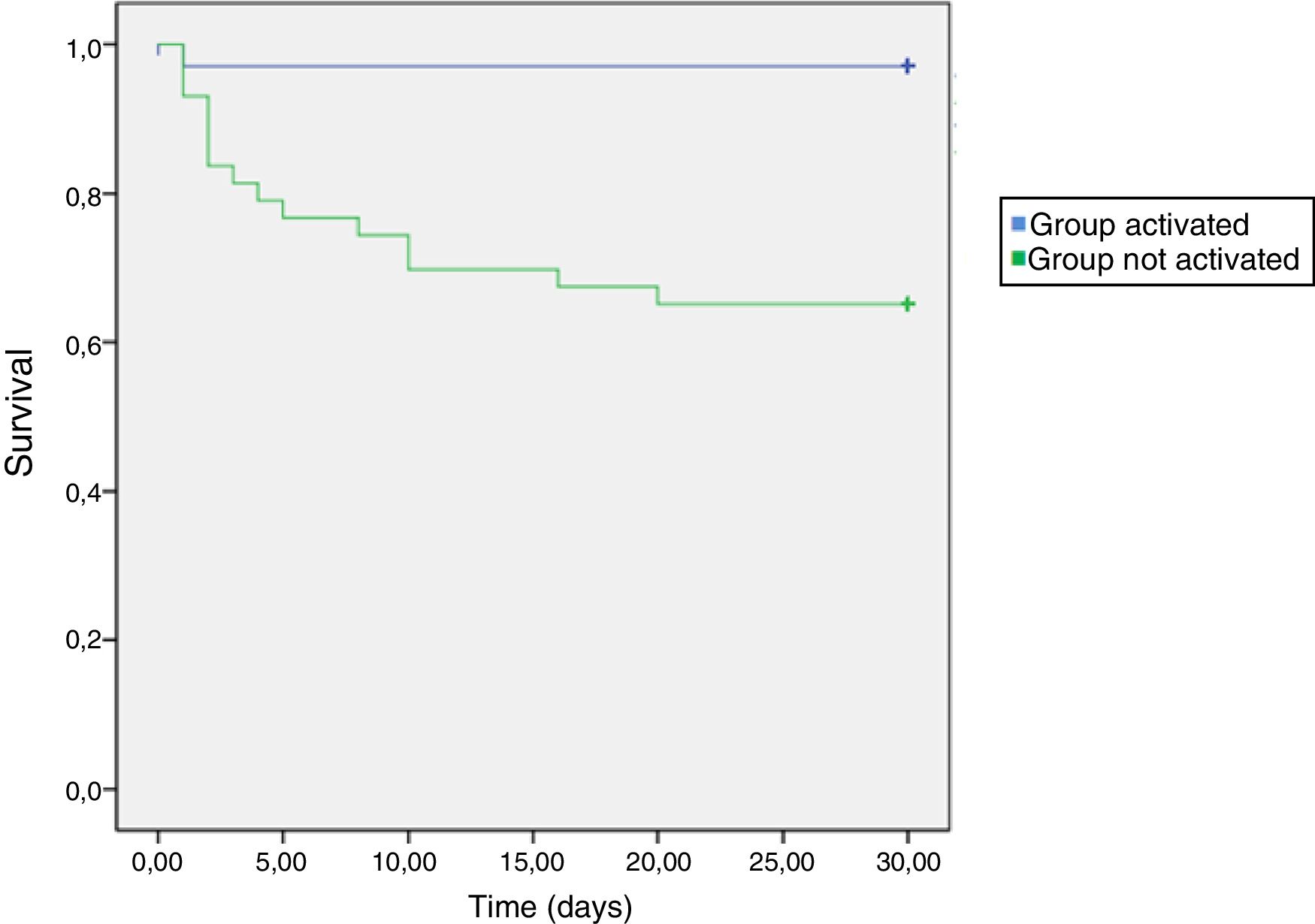
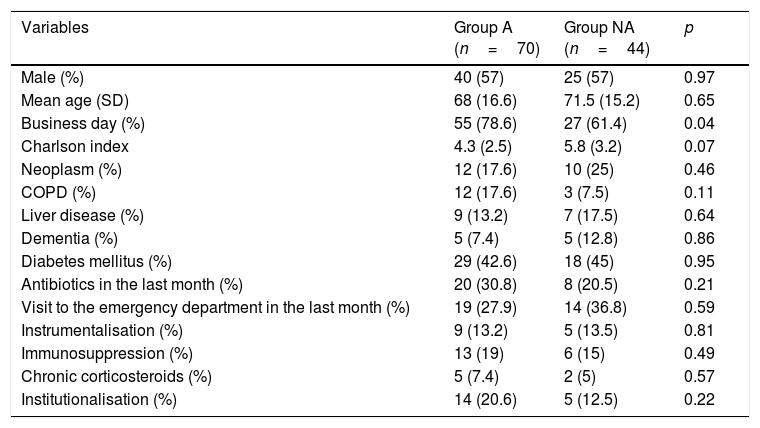
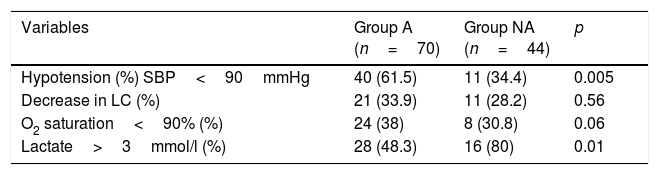
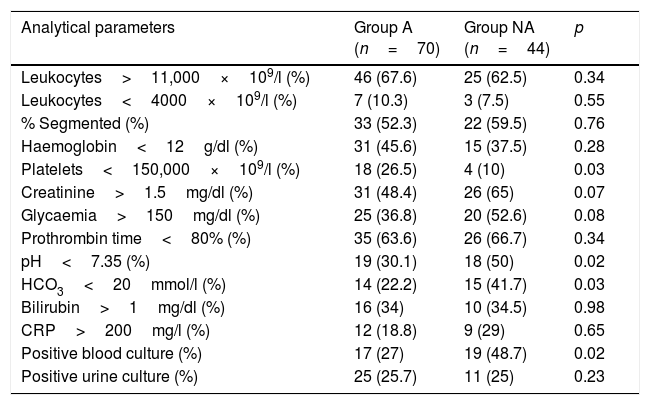
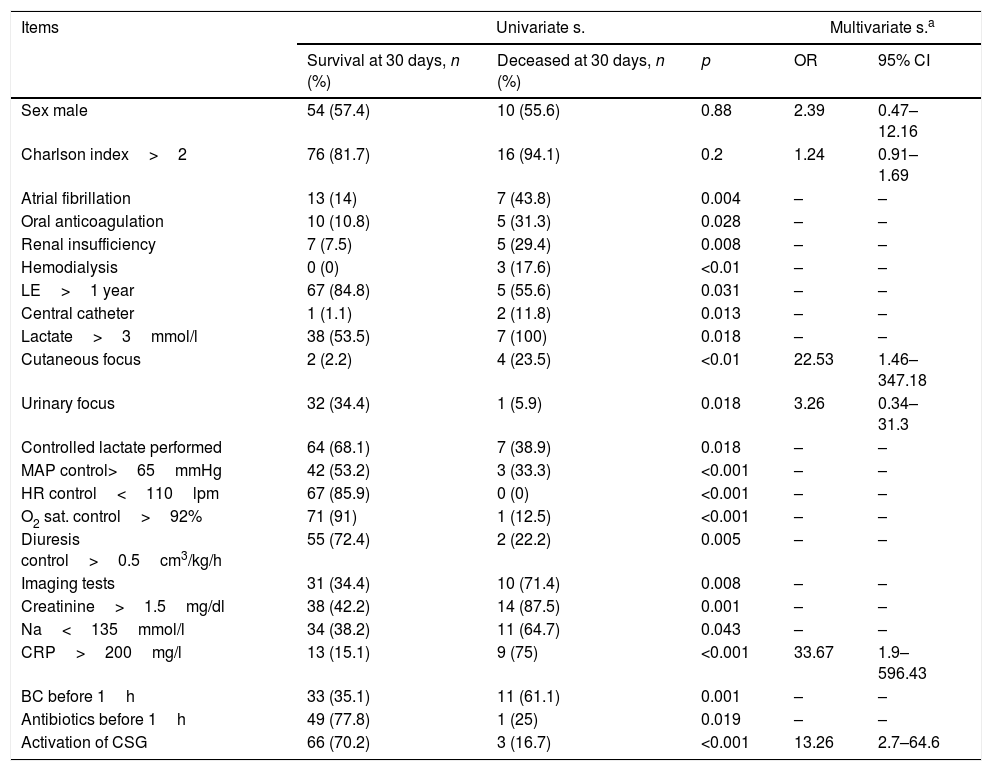
ResultsA total of 114 episodes were found, 61.4% belonging to group A and 38.6% to NA. Patients in group A presented hypotension more frequently (61.5% vs. 34.4%; p=.005). Patients in group NA more frequently had lactate levels of >3mmol/l (48.3% vs. 80%; p=.01), and abdominal focus of sepsis (34.3% vs. 13%; p=.01). In group A, blood cultures were more frequently drawn in the first hour (95% vs. 41.7%; p<.001), early antibiotic was administered (76.9% vs. 25%; p=.005) and fluid replacement carried out (54.5% vs. 18.2%; p=.01). Global achievement of CS objectives was higher in group A (31.4% vs. 9.1%; p=.006). In group NA more patients were admitted to the intensive care unit (10% vs. 36.4%; p<.001), had longer average stays (10.2 days SD 6.9 vs. 14.4 days SD 5.8; p<.001) and a higher mortality rate (4.3% vs. 34.1%; p<.001).
CRP >200mg/l (OR 33.7; p<.001) and the no activation of CS (OR 13.3; p=.001) resulted in being independent factors associated with mortality.
ConclusionsThe implementation of a CS improves compliance with SSC recommendations and decreases intensive care admissions, average stays and mortality.
Evaluar el impacto de la implantación de un código sepsis (CS) en la evolución de pacientes con sepsis grave (SG)/shock séptico (SS). Determinar los factores independientes asociados a mortalidad.
MétodoEstudio de cohortes de pacientes con diagnóstico de SG/SS que consultaron en urgencias de un hospital terciario durante 6 meses. Se analiza el cumplimiento de las recomendaciones de la Surviving Sepsis Campaign, la estancia media, el ingreso en críticos y la mortalidad a 30 días. Se comparan 2 grupos: activación CS (A) y no activación (NA).
ResultadosSe detectaron 114 episodios, 61,4% del grupo A y 38,6% del NA. El grupo A presenta con mayor frecuencia presión arterial sistólica <90mmHg (61,5% vs 34,4%; p=0,005) y el NA mayor elevación del lactato >3mmol/l (48,3% vs 80%; p=0,01) y foco abdominal (34,3% vs 13%; p=0,01). En el grupo A más frecuentemente se cursaron hemocultivos en la primera hora (95% vs 41,7%; p<0,001), se inició antibiótico precoz (76,9% vs 25%; p=0,005), se hizo reposición hídrica inicial (54,5% vs 18,2%; p=0,01) y se cumplieron globalmente los objetivos (31,4% vs 9,1%; p=0,006). El grupo NA tuvo mayor necesidad de ingreso en críticos (10% vs 36,4%; p<0,001), estancia hospitalaria (10,2días; desviación estándar 6,9 vs 14,4días; desviación estándar 5,8; p<0,001) y mortalidad (4,3% vs 34,1%; p<0,001).
Una determinación de proteína C reactiva >200mg/l (odds ratio 33,7; p<0,001) y la no activación del código (odds ratio 13,3; p=0,001) resultaron factores independientes asociados a mortalidad.
ConclusionesLa implantación de un CS mejora el cumplimiento de las recomendaciones y se asocia a una reducción de los ingresos en unidades de críticos, estancia media y mortalidad. La elevación de la proteína C reactiva y la no activación del código son factores independientes asociados a mortalidad. Existe un gran margen de mejora en la detección de los pacientes con SG/SS, así como en la optimización del tratamiento inicial en urgencias.