To assess the accuracy of pharmaceutical anamnesis obtained at the Emergency Department (ED) of a tertiary referral hospital and to determine the prevalence of medication reconciliation errors (RE).
Materials and methodsThis was a single-center, prospective, interventional study. The home medication list obtained by a pharmacist was compared with the one recorded by a doctor to identify inaccuracies. Subsequently, the home medication list was compared with the active prescription at the ED. All unexplained discrepancies were checked with the doctor in charge to evaluate if a RE has occurred. A univariate analysis was performed to identify factors associated with RE.
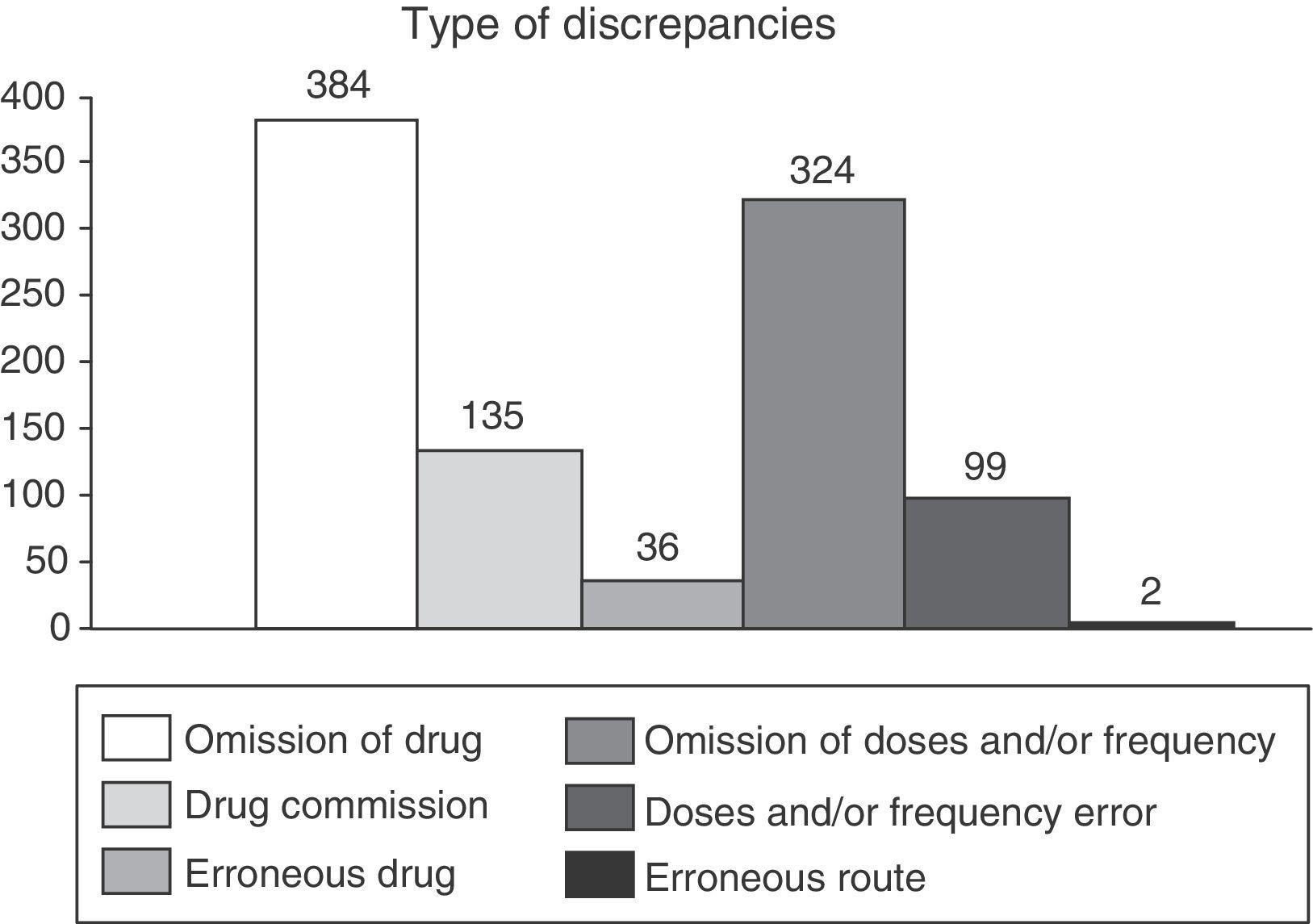
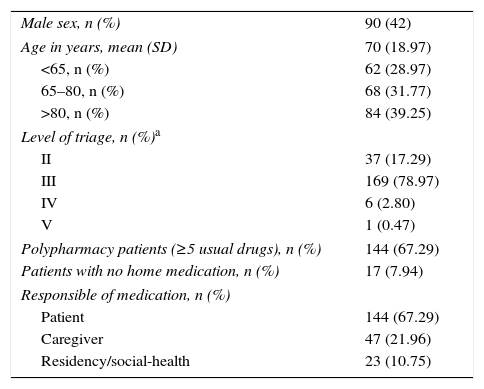
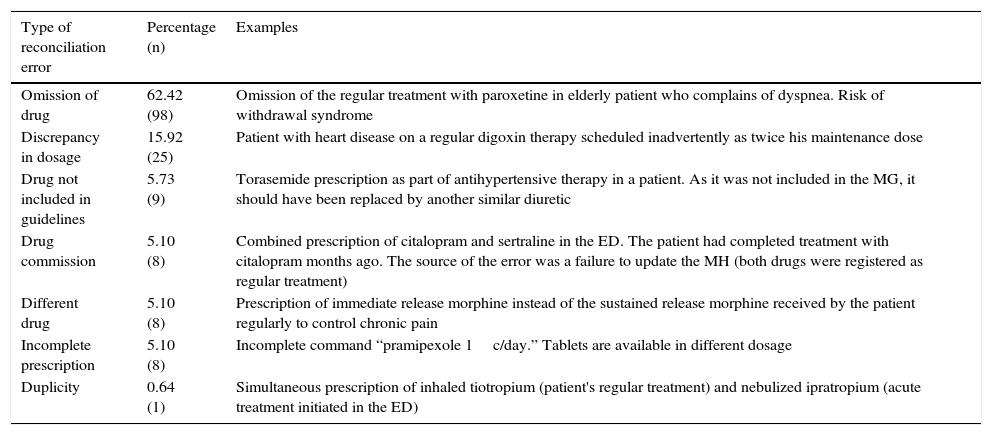
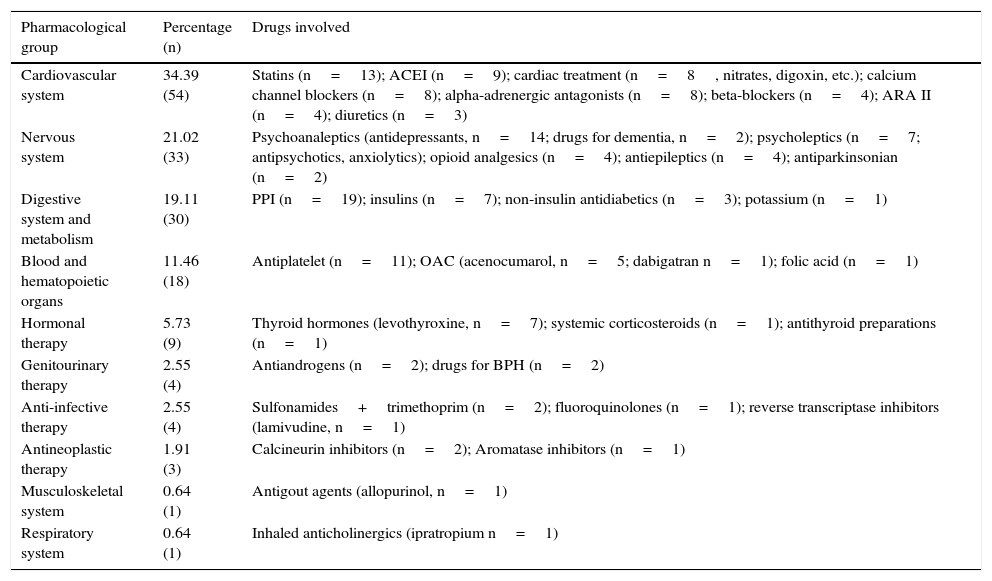
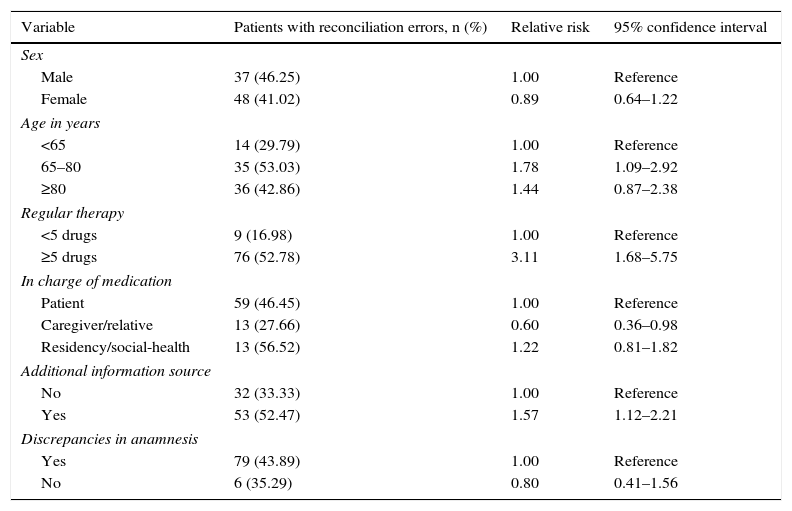
ResultsThe pharmacist identified a higher number of drugs than doctors (6.89 versus 5.70; p<0.05). Only 39% of the drugs obtained by doctors were properly written down in the patient's record. The main cause of discrepancy was omission of information regarding the name of the drug (39%) or its dosage (33%). One hundred and fifty-seven RE were identified and they affected 85 patients (43%), mainly related to information omission (62%). Age and polymedication were identified as main risk factors of RE. The presence of a caregiver or relative in the ED was judged to be a protective factor. No relationship was found between inaccuracies in the registries and RE.
ConclusionsThe process of obtaining a proper pharmaceutical anamnesis still needs improvement. The pharmacist may play a role in the process of obtaining a good quality anamnesis and increase patient safety by detecting RE. Better information systems are needed to avoid this type of incidents.
Evaluar la calidad de la historia farmacoterapéutica registrada en un servicio de urgencias hospitalario (SUH) de un hospital de tercer nivel. Determinar la prevalencia de errores de conciliación (EC).
Material y métodoEstudio unicéntrico, prospectivo y de intervención. Se comparó la lista de medicación habitual obtenida por un farmacéutico frente a la registrada por el médico para identificar discrepancias. Posteriormente, se comparó la medicación habitual con la prescripción activa (SUH). Todas las discrepancias no justificadas se comentaron con el médico para determinar si se trataba de un EC. Se realizó un análisis univariante para identificar factores asociados con la aparición de EC.
ResultadosEl farmacéutico identificó un mayor número de fármacos habituales por paciente respecto al médico (6,89 frente a 5,70; p<0,05). Únicamente el 39% de los fármacos identificados por el médico se registraron correctamente en la historia clínica. La principal causa de discrepancia fue la omisión de información a nivel de fármaco (39%) o de posología (33%). Se detectaron 157 EC que afectaron a 85 pacientes (43%), mayoritariamente por omisión (62%). Los principales factores asociados a EC fueron la edad y la polimedicación. La presencia de un cuidador/familiar responsable de la medicación fue un factor protector. No se encontró asociación entre discrepancias en el registro y EC.
ConclusionesLa recogida de la historia farmacoterapéutica es un proceso susceptible de mejora. El farmacéutico puede ayudar a obtener una anamnesis de calidad e incrementar la seguridad del paciente interceptando EC. Es necesario mejorar los sistemas de información para evitar este tipo de incidentes.