Primary sclerosing cholangitis (PSC) is a rare cholestatic liver disease that typically affects middle-aged men with ulcerative colitis (UC). However, recent studies point out to epidemiological changes. Our aim was to determine if the epidemiology, clinical course and outcome of patients with PSC followed at a reference hepatology centre resemble what is described in the literature.
Patients and methodRetrospective search of patients with a diagnosis of PSC treated in our centre between 2000 and 2019.
ResultsCohort of 55 patients (mean age 37 years), 44% women. Most were large duct type (79%). Most diagnoses were made after 2011. At time of diagnosis, 63% of patients were asymptomatic. The median time from suspicion to diagnosis was 2 years. After a mean follow-up time of 7 years, one third developed cirrhosis, and 25% required liver transplantation (LT); among these, the disease recurred in almost half. Inflammatory bowel disease (IBD) was present in 45%, especially UC. Although statistical significance was not reached, PSC in women was characterised by higher rate of asymptomatic presentation and more frequent association with UC versus other forms of IBD. Women also had more frequently cirrhosis at diagnosis and required LT more often than men.
ConclusionThe epidemiology of PSC is changing. The number of women affected is greater than what was expected from the literature, with a recent increase in incidence. There seems to be differences between sexes in the form of presentation and disease course that should be confirmed in subsequent studies.
La colangitis esclerosante primaria (CEP) es una enfermedad hepática colestásica rara que típicamente afecta a varones de mediana edad con colitis ulcerosa. No obstante, estudios recientes apuntan a cambios epidemiológicos. Nuestro objetivo es determinar si la epidemiología, presentación clínica y curso evolutivo de pacientes con CEP seguidos en un centro de referencia se asemejan a lo descrito en la literatura.
Pacientes y métodosBúsqueda retrospectiva de pacientes con diagnóstico de CEP atendidos en nuestro centro entre los años 2000 y 2019.
ResultadosCohorte de 55 pacientes (media de edad 37 años), 44% mujeres, afectos de CEP, 79% de ducto grande. Casi dos tercios fueron diagnosticados a partir de 2011. En el momento del diagnóstico, un 63% de los pacientes se encontraba asintomático. La mediana de tiempo desde la sospecha hasta el diagnóstico fue de 2 años. Un 34% desarrolló cirrosis en el seguimiento, y 25% requirió trasplante hepático (TH) tras una media de tiempo de 7 años; entre estos, la enfermedad recurrió en un 46%. Un 45% presentaba una EII, sobre todo colitis ulcerosa (CU). Si bien no se alcanzó significación estadística, la CEP en mujeres se caracterizó por mayor tasa de presentación asintomática, mayor asociación con CU frente a otras formas de EII, así como cirrosis al diagnóstico y necesidad de TH con mayor frecuencia que los hombres.
ConclusionesLa epidemiología de la CEP está cambiando. El número de mujeres afectas es mayor al descrito previamente, objetivándose un aumento reciente de la incidencia. Podrían existir diferencias entre sexos en la forma de presentación y evolución que deberán confirmarse en estudios posteriores.
Primary sclerosing cholangitis (PSC) is a rare cholestatic liver disease characterised by progressive obliteration of intra- and extrahepatic bile ducts, secondary to inflammation and fibrosis, leading to end-stage liver failure after an average of 13–21 years.1 Its incidence and prevalence rates range between 0–1.3 per 100,000 inhabitants/year and 0–16.2 per 100,000 inhabitants/year, respectively.2 It is characterised by male predominance (M:F, 2:1), mean age of onset of around 40 years old, absence of specific autoantibodies, and poor response to immunosuppression. Liver transplantation (LT) is the only effective treatment to increase survival, but the disease recurs in up to 20–30% of patients.3,4 It is associated with an increased risk of biliary and colorectal cancer.5 Many studies have demonstrated its close relationship with inflammatory bowel disease (IBD), with a prevalence in patients with PSC of around 70% according to series.6–8
As with other autoimmune liver diseases (ALD), such as primary biliary cholangitis (PBC) or autoimmune hepatitis (AIH), sex plays a role not only in the prevalence of the disease, but also in its evolutionary course.9 Thus, for example, in PBC, men generally require LT at older ages than women, with the proportion of transplants for this indication having increased in recent years with regard to the female sex.10 On the other hand, they present a worse response to treatment, a more aggressive course and a higher incidence of hepatocellular carcinoma (HCC) and overall mortality from the disease compared to women.11,12
Regarding AIH, male sex is a risk factor for developing HCC.13 However, susceptibility to developing the disease itself is reduced, compared to the female sex. In addition, it has been observed that the long-term prognosis is better in men than in women with AIH.14
The influence of sex on PSC is less clear. In Spain, there are no studies that investigate the impact of sex on PSC, nor is there recent data on the epidemiology, onset, clinical picture, evolution and response to treatment of this disease in the Mediterranean area. Therefore, the objective of our study is, firstly, to describe the most relevant features of patients with PSC, such as the association with IBD or the need for LT, followed up at a reference centre with LT in the Comunidad Valenciana [Autonomous Community of Valencia], and to see if it resembles what is described in the literature. Secondly, we will perform an analysis to see if differences exist related to sex in patients with PSC.
Patients and methodsA retrospective search for patients diagnosed with PSC treated at our centre, Hospital Universitario y Politécnico La Fe de Valencia [La Fe University and Polytechnic Hospital of Valencia], between 2000 and 2019, was carried out. Whether or not the diagnosis was made during that period of time or beforehand was not taken into account. Both patients followed up in outpatient clinics and those who had required hospitalisation were included. The medical records of the patients were reviewed using Electronic Health Record software from the hospital (ORION CLINIC) and the centre for specialties and primary care (ABUCASIS), through which the information was obtained.
Inclusion and exclusion criteriaPatients ≥16 years of age (of legal age medically, and, therefore, followed up by adult hepatology outpatients) with an established diagnosis of PSC, including small-duct PSC, were included. Patients with AIH overlap were also selected for the study. Other similar clinical entities such as immunoglobulin G4-associated cholangitis, PBC, or isolated AIH were not included.15
Patients who had undergone LT for this indication and non-transplant patients were included. Those patients for whom a diagnosis could not be verified by clinical, radiological and/or histological criteria were excluded from the study.
All causes of secondary sclerosing cholangitis or diseases that may mimic PSC were excluded,16,17 including cholangiocarcinoma, choledocholithiasis, bile duct injury following surgery, inflammatory pseudotumour of the liver, eosinophilic cholangitis, mast cell cholangiopathy, portal hypertensive biliopathy, AIDS cholangiopathy, recurrent pyogenic cholangitis and ischaemic cholangitis, among others.
VariablesThe main variables of the study were the following: baseline demographic data, including age, sex, race/ethnicity and body mass index (BMI); coexistence of IBD (type, year of diagnosis, treatments received and dates, colectomy) or of other autoimmune diseases; form of onset and time to diagnosis; main laboratory alterations (glutamic oxaloacetic transaminase [GOT], alanine aminotransferase [ALT], gamma-glutamyl transferase [GGT], alkaline phosphatase [ALP], bilirubin, Quick test [QT], albumin) from laboratory tests at diagnosis, pre-LT laboratory tests and those from the last consultation; autoantibodies and serologies; type of PSC (small-duct/classic/mixed); overlap with AIH; stage of fibrosis at diagnosis and at last visit; progression to compensated and/or decompensated cirrhosis, development of HCC and/or cholangiocarcinoma (CC); need for LT; death and cause of death. Among treatments, use of ursodeoxycholic acid (UDCA), start date and dose (greater than or equal to 15 mg/kg/day); endoscopic treatments, radiological treatments and chronic excessive alcohol intake (if alcohol consumption was greater than 30 g/day in men and 20 g/day in women) were recorded.
Statistical methodsThe IBM SPSS® Statistics v25.0.0 software programme was used. Quantitative variables were expressed in terms of mean and standard deviation or median and interquartile ranges. For qualitative variables, frequency and percentage were used. For comparisons, the Chi-square test was used to compare qualitative variables and Student’s t-test to analyse quantitative variables.
All analyses were stratified by sex and adjusted for age at diagnosis. A p value <0.05 was considered statistically significant.
Ethical approvalFinally, it is stated that the study was reviewed and approved by the Medicines Research Ethics Committee (mREC) of the Hospital Universitario y Politécnico La Fe.
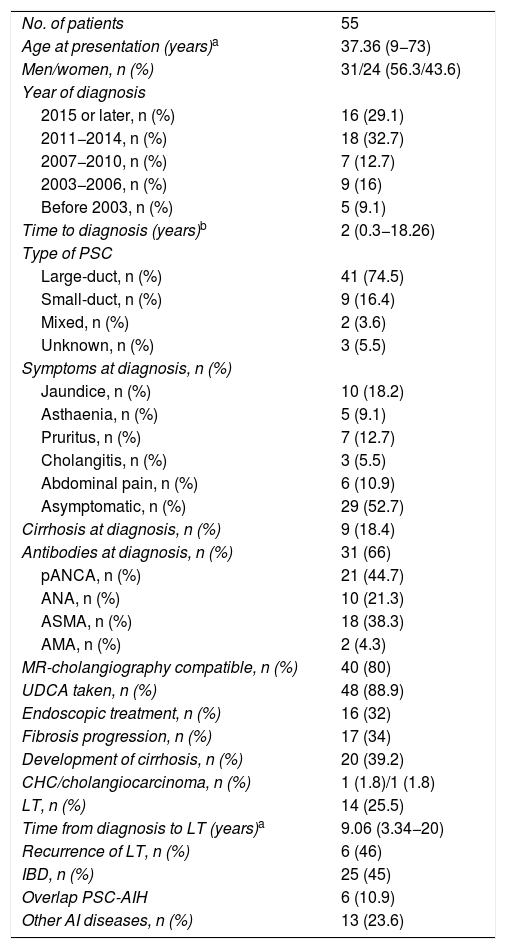
ResultsBaseline characteristics of the patients without differentiating by sex (Table 1)We identified 55 patients with a diagnosis of PSC treated at our centre between 2000 and 2019. Two patients initially selected were excluded because they did not meet the diagnosis of PSC: in both cases the final diagnosis was sclerosing cholangitis secondary to recurrent cholangitis due to recurrent intrahepatic lithiasis.
Description of baseline variables in patients with PSC.
| No. of patients | 55 |
| Age at presentation (years)a | 37.36 (9−73) |
| Men/women, n (%) | 31/24 (56.3/43.6) |
| Year of diagnosis | |
| 2015 or later, n (%) | 16 (29.1) |
| 2011−2014, n (%) | 18 (32.7) |
| 2007−2010, n (%) | 7 (12.7) |
| 2003−2006, n (%) | 9 (16) |
| Before 2003, n (%) | 5 (9.1) |
| Time to diagnosis (years)b | 2 (0.3−18.26) |
| Type of PSC | |
| Large-duct, n (%) | 41 (74.5) |
| Small-duct, n (%) | 9 (16.4) |
| Mixed, n (%) | 2 (3.6) |
| Unknown, n (%) | 3 (5.5) |
| Symptoms at diagnosis, n (%) | |
| Jaundice, n (%) | 10 (18.2) |
| Asthaenia, n (%) | 5 (9.1) |
| Pruritus, n (%) | 7 (12.7) |
| Cholangitis, n (%) | 3 (5.5) |
| Abdominal pain, n (%) | 6 (10.9) |
| Asymptomatic, n (%) | 29 (52.7) |
| Cirrhosis at diagnosis, n (%) | 9 (18.4) |
| Antibodies at diagnosis, n (%) | 31 (66) |
| pANCA, n (%) | 21 (44.7) |
| ANA, n (%) | 10 (21.3) |
| ASMA, n (%) | 18 (38.3) |
| AMA, n (%) | 2 (4.3) |
| MR-cholangiography compatible, n (%) | 40 (80) |
| UDCA taken, n (%) | 48 (88.9) |
| Endoscopic treatment, n (%) | 16 (32) |
| Fibrosis progression, n (%) | 17 (34) |
| Development of cirrhosis, n (%) | 20 (39.2) |
| CHC/cholangiocarcinoma, n (%) | 1 (1.8)/1 (1.8) |
| LT, n (%) | 14 (25.5) |
| Time from diagnosis to LT (years)a | 9.06 (3.34−20) |
| Recurrence of LT, n (%) | 6 (46) |
| IBD, n (%) | 25 (45) |
| Overlap PSC-AIH | 6 (10.9) |
| Other AI diseases, n (%) | 13 (23.6) |
The numbers in parentheses indicate the prevalence of the variable.
AI: autoimmune; AIH: autoimmune hepatitis; AMA: antimitochondrial antibodies; ANA: antinuclear antibodies; ANCA: anti-neutrophil cytoplasmic antibodies; ASMA: anti-smooth muscle antibodies; HCC: hepatocellular carcinoma; IBD: inflammatory bowel disease; LT: liver transplant; MRI: magnetic resonance imaging; PSC: primary sclerosing cholangitis; UDCA: ursodeoxycholic acid.
Hepatitis B and C virus serology was negative in all cases, while 16 had immunity against hepatitis A virus. Wilson’s disease and haemochromatosis were ruled out in 74.5% and 30.9%, respectively.
Epidemiology and associated autoimmune diseaseThe men to women ratio in our cohort was practically 1:1 (31 M:24 W). All patients were of Caucasian ethnicity. The mean age at diagnosis was 37.36 years.
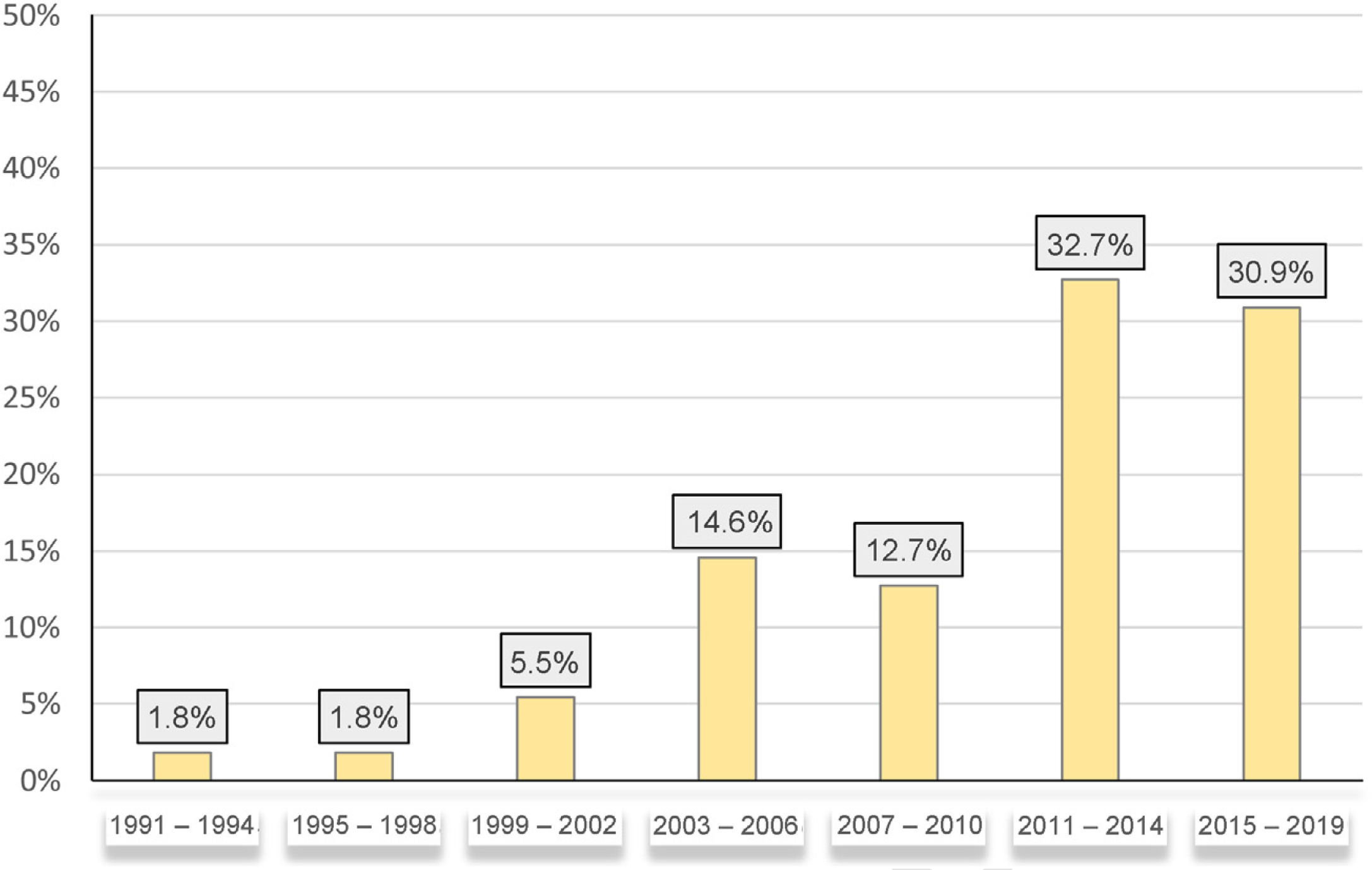
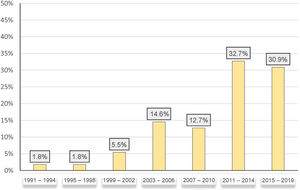
The percentage of patients diagnosed with PSC in our sample increased over the years, such that up to 64% of patients were diagnosed after 2011 (Fig. 1).
Although only four patients had a family history (in first-degree relatives) of autoimmune or liver disease, more than 50% of the patients had a personal medical history of other autoimmune diseases in addition to PSC. IBD was the most common associated immune-mediated disease (25 patients, 45% of the total). The other immune-mediated diseases were, in order of frequency: autoimmune hypothyroidism-Hashimoto’s thyroiditis (five patients, 9.1%), perineal hidradenitis (one patient, 1.8%), allergic asthma (one patient, 1.8%), vasculitis (1.8%), eosinophilic colitis (1.8%), allergic rhinitis (1.8%), polyarticular juvenile idiopathic arthritis (1.8%) and coeliac disease (1.8%). Regarding toxic habits, 10 were smokers and five had a chronic excessive intake of alcohol.
Clinical picture, diagnostic techniques, autoantibodies at diagnosisThe most common clinical picture at the time of diagnosis of the disease was jaundice (21.7%). However, the asymptomatic state was more common, being observed in 63% of the patients. Pruritus (15.2%), isolated abdominal pain (13%), asthenia (10.9%) and cholangitis (6.5%) constituted the rest of the clinical manifestations at diagnosis.
The median time to diagnosis from first suspicion was two years (range: 0.3 years–18.26 years). Among the complementary imaging tests used to diagnose the disease, liver ultrasound was used in up to 92.7% of patients. However, despite its widespread use, in 24 patients (50%) the result was normal, that is, it did not show biliary or parenchymal alterations. Magnetic resonance cholangiography, used in 96.1% of patients, found characteristic pathological changes in the bile duct in 41 patients (74.5%).
Liver biopsy was performed in 30 patients (54.5%), the main reasons being to rule out associated AIH and the histological diagnosis of small-duct PSC. The biopsy was compatible with PSC-AIH in six patients (10.9%).
Autoantibodies were determined in 47 patients. A titre equal to or greater than 1:40 was considered positive. Perinuclear anti-neutrophil cytoplasmic antibodies specific for myeloperoxidase (pANCA) were the most prevalent antibodies, present in 44.7% of the total, followed by anti-smooth muscle antibodies (ASMA) 38.3%, antinuclear antibodies (ANA) 21.3% and antimitochondrial antibodies (AMA) 4.3%.
Classic or large-duct PSC was present in 74.5% of patients. Small-duct PSC constituted 16.4% of the sample. Both entities were present in two patients (mixed PSC).
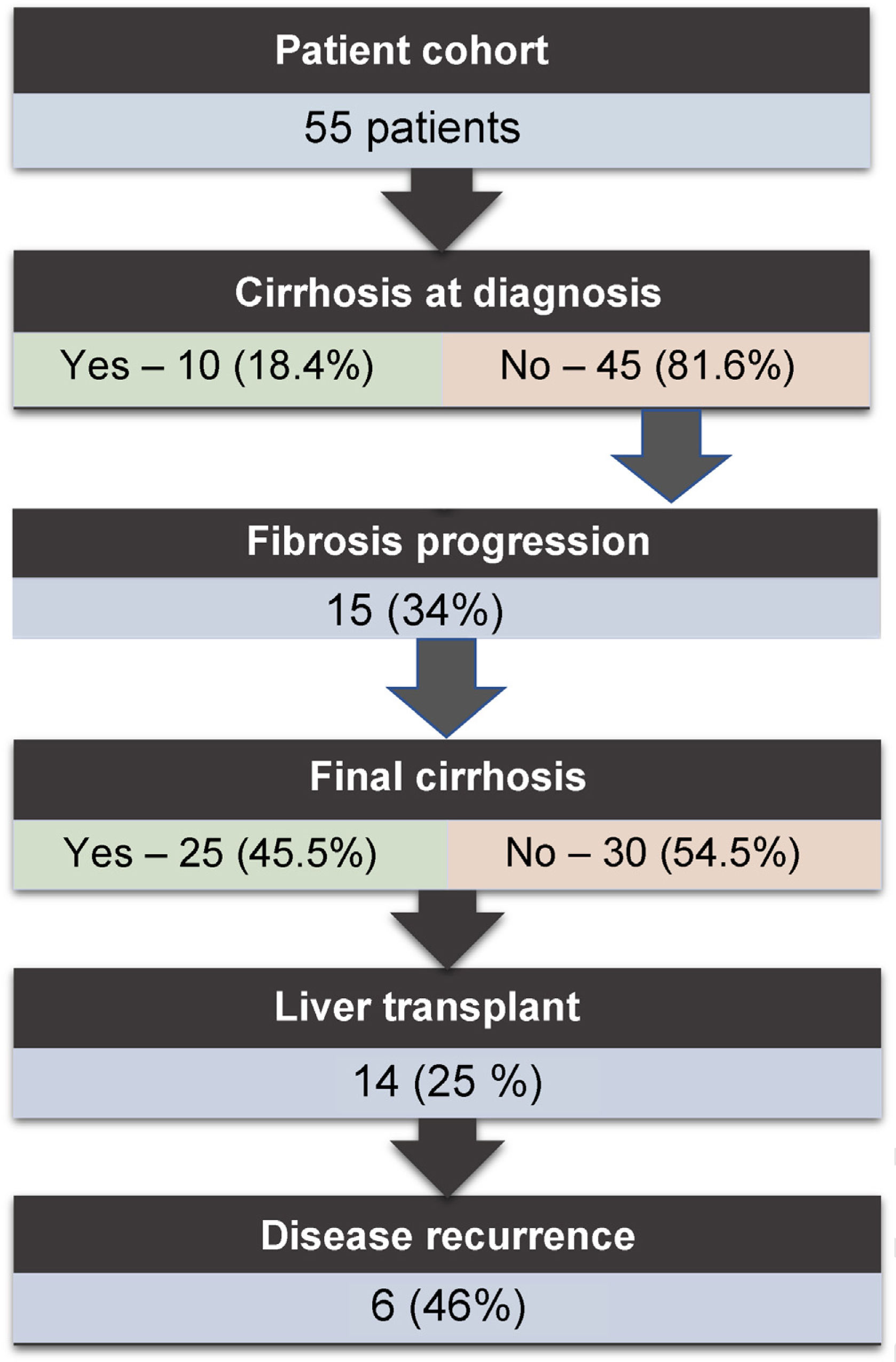
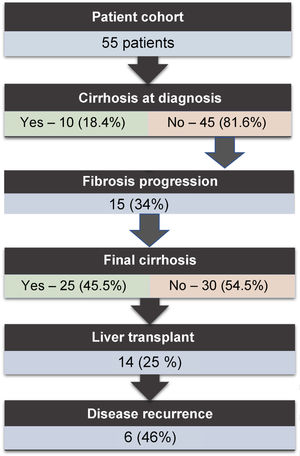
Disease evolution, treatment and liver transplantationAt diagnosis, 18% of the patients already had cirrhosis (in only two patients was it decompensated). An average of nine years elapsed from the onset of the disease to the first decompensation of cirrhosis in the patients in whom the disease progressed. After a mean follow-up of seven years, a third of the patients developed cirrhosis, and 25% required LT (n = 14); among these, the disease recurred in practically half. The main indication for LT was advanced liver failure with severe portal hypertension (n = 7). Other indications were recurrent cholangitis (n = 5) or liver abscesses (n = 1). Among the patients with recurrence of the disease, 33.3% had an associated IBD. Total or subtotal colectomy as final treatment for ulcerative colitis (UC) was required in two patients with LT. There was no recurrence of the disease in these patients. The evolution of the patients in our cohort is represented in Fig. 2.
Only two cases of cancer were reported: one case of HCC and one case of CC; no cases of colon cancer. Death occurred in four patients (7.3%): one due to CC, one due to end-stage liver failure and two due to septic shock.
Among other complications of the disease, five patients reported intolerable pruritus (9.3%) and two of these patients required the use of extracorporeal albumin dialysis (MARS). None of the patients underwent transplant for this reason. Recurrent cholangitis was detected in 11 patients (20.4%).
UDCA was prescribed in up to 88.9% of patients (with a dose higher than 15 mg/kg in 37% of these). Interventional treatments were also employed in 16 patients (29.1%): ERCP in 14 patients and interventional radiology in two. The indications for these treatments were stenosis of the bile duct in eight patients, recurrent cholangitis in six, and drainage of abscesses in two.
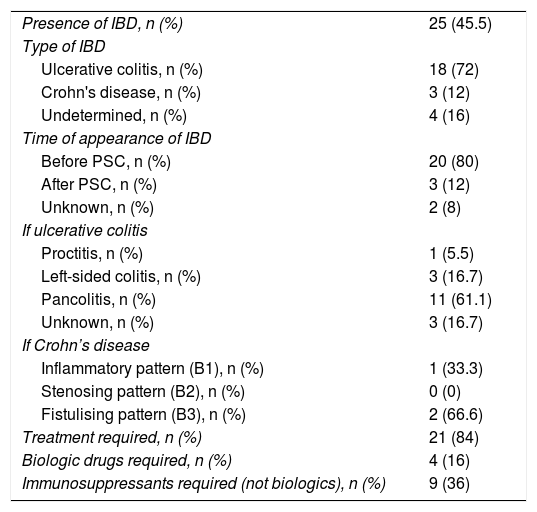
Inflammatory bowel disease (Table 2)IBD was present in 25 patients (45%). It preceded the diagnosis of PSC in 87% of patients. The most common form of IBD was UC (72%), which stood out above indeterminate colitis (16%) and Crohn's disease (12%). UC led most frequently by far to pancolitis (61.1%), followed by left-sided colitis and proctitis.
Inflammatory bowel disease.
| Presence of IBD, n (%) | 25 (45.5) |
| Type of IBD | |
| Ulcerative colitis, n (%) | 18 (72) |
| Crohn's disease, n (%) | 3 (12) |
| Undetermined, n (%) | 4 (16) |
| Time of appearance of IBD | |
| Before PSC, n (%) | 20 (80) |
| After PSC, n (%) | 3 (12) |
| Unknown, n (%) | 2 (8) |
| If ulcerative colitis | |
| Proctitis, n (%) | 1 (5.5) |
| Left-sided colitis, n (%) | 3 (16.7) |
| Pancolitis, n (%) | 11 (61.1) |
| Unknown, n (%) | 3 (16.7) |
| If Crohn’s disease | |
| Inflammatory pattern (B1), n (%) | 1 (33.3) |
| Stenosing pattern (B2), n (%) | 0 (0) |
| Fistulising pattern (B3), n (%) | 2 (66.6) |
| Treatment required, n (%) | 21 (84) |
| Biologic drugs required, n (%) | 4 (16) |
| Immunosuppressants required (not biologics), n (%) | 9 (36) |
The numbers in parentheses indicate the prevalence of the variable.
Montreal classification: evolutionary pattern (Behaviour): B1: inflammatory pattern; B2: stenosing pattern; B3: fistulising pattern.
IBD: inflammatory bowel disease; PSC: primary sclerosing cholangitis.
Among those with Crohn's disease, two patients presented a fistulising pattern (B3 of the Montreal Classification of Crohn's disease) and another patient had a solely inflammatory pattern (B1 of the Montreal Classification of Crohn's disease).
Up to 84% of patients with IBD required treatment (immunosuppressants, 5-ASA, biological drugs, etc.) for their disease during follow-up. In nine patients (36%) the use of immunosuppressants was required and in four patients, biological drugs were employed (16%).
Analysis according to the sex of the patientsEpidemiology and associated autoimmune diseaseThe men to women ratio in our sample was practically 1:1 (31 M:24 W). The mean age at diagnosis was very similar in both groups (37.25 years in men vs. 37.51 years in women) (p = 0.947). The mean time to diagnosis from the first clinical manifestation or laboratory test abnormality was higher in the group of women compared to men (4.45 years on average in women vs. 3.71 years on average in men; p = 0.736). In other words, it took 7.5 months longer on average to diagnose women than men. No significant differences were observed in the proportion of the disease between the two groups in recent years (from 2011 to the present, 19 men [61.3% of the total number of men] and 15 women [62.5% of the total number of women]; p = 0.854). Neither were differences seen in the presence of other autoimmune diseases in addition to PSC (15 in men [48.4%] vs. 14 in women [58.3%]; p = 0.464).
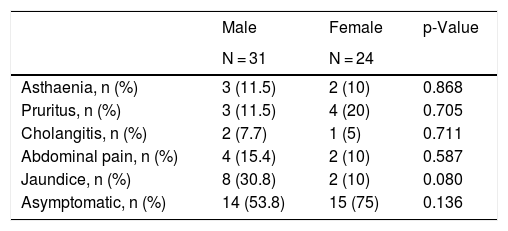
Clinical manifestations, diagnostic techniques and autoantibodies on diagnosisThe most common clinical presentation at diagnosis in men was jaundice (p = 0.080), while in women it was pruritus (p = 0.705). In both groups, cholangitis was the least common clinical manifestation. In some cases several manifestations occurred simultaneously. There were no significant differences regarding the clinical manifestations at the time of presentation of the disease, as shown in Table 3.
Differences in clinical manifestations according to sex.
| Male | Female | p-Value | |
|---|---|---|---|
| N = 31 | N = 24 | ||
| Asthaenia, n (%) | 3 (11.5) | 2 (10) | 0.868 |
| Pruritus, n (%) | 3 (11.5) | 4 (20) | 0.705 |
| Cholangitis, n (%) | 2 (7.7) | 1 (5) | 0.711 |
| Abdominal pain, n (%) | 4 (15.4) | 2 (10) | 0.587 |
| Jaundice, n (%) | 8 (30.8) | 2 (10) | 0.080 |
| Asymptomatic, n (%) | 14 (53.8) | 15 (75) | 0.136 |
The numbers in parentheses indicate the prevalence of the variable.
Small-duct disease was diagnosed in six men (19.4% of men) and three women (14.3% of women).
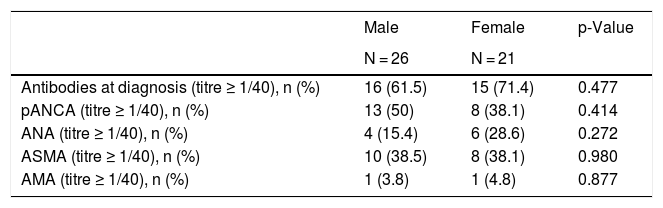
The presence or absence of autoantibodies was available in 26 men and 21 women. Autoantibodies were found in 16/26 (61.5%) of men and 15/21 (71.4%) of women, respectively, with no statistically significant differences. The most common autoantibodies were perinuclear anti-neutrophil cytoplasmic antibodies (pANCA) in 13 men (50%) and eight women (38.1%); p = 0.414, and anti-smooth muscle autoantibodies (ASMA) in 10 men (38.5%) and eight women (38.1%); p = 0.980.
At diagnosis, 28 men (93.3%) had biochemical cholestasis. In the group of women, all (100%) had cholestatic biochemical alterations. Table 4 shows the main findings related to laboratory test abnormalities.
Differences in laboratory parameters according to sex.
| Male | Female | p-Value | |
|---|---|---|---|
| N = 26 | N = 21 | ||
| Antibodies at diagnosis (titre ≥ 1/40), n (%) | 16 (61.5) | 15 (71.4) | 0.477 |
| pANCA (titre ≥ 1/40), n (%) | 13 (50) | 8 (38.1) | 0.414 |
| ANA (titre ≥ 1/40), n (%) | 4 (15.4) | 6 (28.6) | 0.272 |
| ASMA (titre ≥ 1/40), n (%) | 10 (38.5) | 8 (38.1) | 0.980 |
| AMA (titre ≥ 1/40), n (%) | 1 (3.8) | 1 (4.8) | 0.877 |
| Male | Female | p-Value | |
|---|---|---|---|
| N = 31 | N = 21 | ||
| Biochemistry of cholestasis at diagnosis, n (%) | 28 (93.3) | 21 (100) | 0.227 |
| ALT/GPT at diagnosis (UI/l)a | 101.65 | 104.47 | 0.923 |
| AST/GOT at diagnosis (UI/l)a | 79.69 | 89.73 | 0.674 |
| GGT at diagnosis (UI/l)a | 542.12 | 274.68 | 0.085 |
| ALP at diagnosis (UI/l)a | 354.75 | 415.35 | 0.583 |
| Total bilirubin at diagnosis (mmol/l)a | 3.49 | 1.72 | 0.194 |
| Albumin at diagnosis (g/l)a | 4.13 | 4.04 | 0.617 |
The numbers in parentheses indicate the prevalence of the variable.
ALP: alkaline phosphatase; ALT/GPT: alanine aminotransferase/glutamic-pyruvic transaminase; AMA: antimitochondrial antibodies; ANA: antinuclear antibodies; ANCA: anti-neutrophil cytoplasmic antibodies; ASMA: anti-smooth muscle antibodies; AST/GOT: aspartate aminotransferase/glutamic oxaloacetic transaminase; GGT: gamma-glutamyl transferase; LKM-1: liver kidney microsome type 1 antibodies.
13 men (52%) and 12 women (48%) were diagnosed with IBD associated with PSC, with no significant differences. In both subgroups, IBD presented before the diagnosis of PSC in the majority of patients (90.9% in men and 83.3% in women). Within the type of IBD, UC stood out above Crohn's disease and indeterminate colitis (72% UC vs. 12% CD vs. 16% indeterminate colitis). The proportion of UC in women (91.7%) was higher than that of men (53.8%) who presented a more homogeneous distribution of IBD subtypes with CD and indeterminate colitis. However, these results did not achieve statistical significance (p = 0.088).
Biologic drugs (30.7 vs. 0%) and immunosuppressants (IS) (53.8 vs. 16.6%) were used to a greater extent in men compared to women, p = 0.068 and 0.053, respectively.
Disease evolution, treatment and liver transplantationCirrhosis was found at diagnosis in four men and five women, and there were only two cases of decompensated cirrhosis at diagnosis, both in women, and in both cases in the form of ascites, with no significant differences (p = 0.116).
In patient follow-up, stage of fibrosis progressed in nine men and eight women (p = 0.754) and the final stage of cirrhosis was reached in a total of 20 patients (10 men vs. 10 women; p = 0.427). LT was required in seven men (22.6%) and seven women (29.2%), with no significant differences between the two groups (p = 0.578).
Disease recurred after transplantation more frequently in men than in women: four men (57.1% of transplanted men) vs. two women (33.3% of the transplanted women), with no statistical significance (p = 0.391).
DiscussionPSC is a rare cholestatic disease of unknown aetiology for which there is no specific treatment.1,3 In this study, we report a cohort of 55 patients with PSC followed up in an LT reference centre in the Mediterranean basin, in Spain. Our patients presented typical epidemiological characteristics of the disease, similar to those described in the literature, with a mean age of 30–40 years.5. The percentage of men was lower than the 60–70% described in most series published to date.2 There is recent evidence of an increased incidence of the disease,18 as supported by the results of our work. This increased incidence in our environment could be related to the increase in IBD in Western countries,1 in which both entities are increasingly prevalent.
The autoimmune burden of patients with PSC is very high, probably higher than that of patients with IBD, as demonstrated by a study in which up to 24% of patients with PSC presented an associated autoimmune disease and, in up to 9%, two or more autoimmune diseases.19 Likewise, the overlap between PSC and AIH in the West varies between 8–49%.3 It is possible that the evaluation for LT, at which time numerous laboratory, imaging and endoscopic diagnostic tests are performed, explains, in part, the higher than 50% rate of patients with another associated autoimmune disease.
In our centre, a colonoscopy was not performed on all patients with PSC. The percentage of patients with IBD was lower than that described in most published series.23 However, the characteristics of IBD in these patients, with a diagnosis prior to PSC and with pancolitis as the main subtype of UC, were similar to those described in most publications.24
LT is the only effective treatment to improve the prognosis of PSC.8 It represents 4% of the total LT in Europe (according to the European Liver Transplant Registry)21 and 1.4% of LT in Spain (data from the Registro Español de Trasplante Hepático [Spanish Registry of Liver Transplantation] 2018). The criteria used in clinical practice to define recurrence, which may erroneously include cases of ischaemic stenosis or ductopenic rejection,4 could explain the high requirement for retransplantation both in our series and in others, with recurrence rates of around 10–27% having been described in the literature.22
Unlike multicentre studies or international registries where rates of mortality, CC and colorectal cancer are described at around 14–28, 4–11 and 2–7%, respectively,7 these rates were much lower in our cohort. Among the various reasons that could justify the low mortality at our hospital, is the high rate of LT and its relative promptness (average seven years until LT) compared to other series, which describe 9–12 years on average after diagnosis.4
Despite the controversy over the efficacy of UDCA in improving survival or the need for LT,25 the majority of our patients received this therapy in line with most of the published works.
It has been widely demonstrated that sex plays an important role in hepatic autoimmune diseases, especially AIH and PBC.9 Our research found no significant differences in the analysis by sex in the variables studied, possibly due to the small sample size of the subgroups. Even so, some non-significant differences were observed that are worth mentioning. The mean time elapsed between clinical presentation and definitive diagnosis was higher in women than in men, perhaps due to the deep-rooted concept that this is a disease that fundamentally affects men. Regarding IBD, several studies have shown a higher prevalence in men,26,27 as well as lower frequency of UC in women.27 These data are not confirmed in our cohort. Several studies have analysed the microbiota, detecting differences between the sexes that could predispose patients to immune-mediated diseases, a factor that should be taken into account and studied in future research on IBD and PSC.28
Although differences between the sexes in disease severity have not been clearly demonstrated in PSC, a higher risk of disease progression in men compared to women has recently been described.27 In our cohort of patients, no significant differences were found in fibrosis progression, death, need for LT, or post-LT recurrence. Male sex and intact colon (not operated on) at the time of transplantation are associated with a higher risk of post-LT recurrence.3,28 In our series, no differences were found in patients with recurrence, either in the history of IBD or in the history of colectomy.
Small-duct PSC is associated with a better long-term prognosis of the disease and is not related to CC, as long as it does not progress to large-duct PSC, which occurs in 20–25% of cases.3,5 In Western countries it represents an average of between 6–16% according to studies.20 Although it has been described as more common in women, which could explain the different prognosis of the disease between men and women,27 in our cohort it was more common in men.
Among the weaknesses of this observational study, the small sample size stands out, as well as the geographical area it covered (single-centre study) that could make it difficult to extrapolate the results to other areas of Europe, or its retrospective nature, which prevents an adequate evaluation of the natural evolution and prognosis of the illness. In addition, the absence of data in the medical records for some variables represented a loss of information. Finally, as this is a study that has been carried out in an LT reference centre, we cannot rule out the fact that both the increase in cases in recent years, as well as the high percentage of cirrhotic patients in our cohort, are secondary to a selection bias.
ConclusionsAt our centre, the epidemiology of PSC seems to be changing. The number of women affected is greater than that described in the literature, and there is a recent increase in diagnoses of this disease. In addition, although no significant differences between the sexes have been found, interesting trends in presentation and evolution can be seen. Determining whether these results are real or the result of selection bias is not possible with our data. This retrospective study in a tertiary centre with LT could serve as a starting point for future research in the same setting, with the participation of other centres or regions in order to achieve a larger sample size that would allow us to confirm or reject the trends found in our research.
FundingThis study received no specific funding from public, private or non-profit organisations.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Mínguez Sabater A, Conde Amiel I, Ladrón Abia P, Martínez Delgado S, Camarasa Pérez Á, Berenguer M. Características e impacto del sexo en una cohorte de pacientes con colangitis esclerosante primaria: experiencia de un centro trasplantador de la cuenca mediterránea. Gastroenterol Hepatol. 2022;45:177–185.