To assess the effectiveness of a telephonic interview performed by primary care professionals among non-participants in the first round of the colorectal cancer early detection programme in the basic urban health area Guineueta in Barcelona, Spain.
Patients and methodsThe Primary Healthcare Team of La Guineueta contacted people who did not respond to the invitation to the first round of the colorectal cancer early detection programme using a standardised telephone call protocol. We analysed the impact of the intervention based on participation and diagnosed disease.
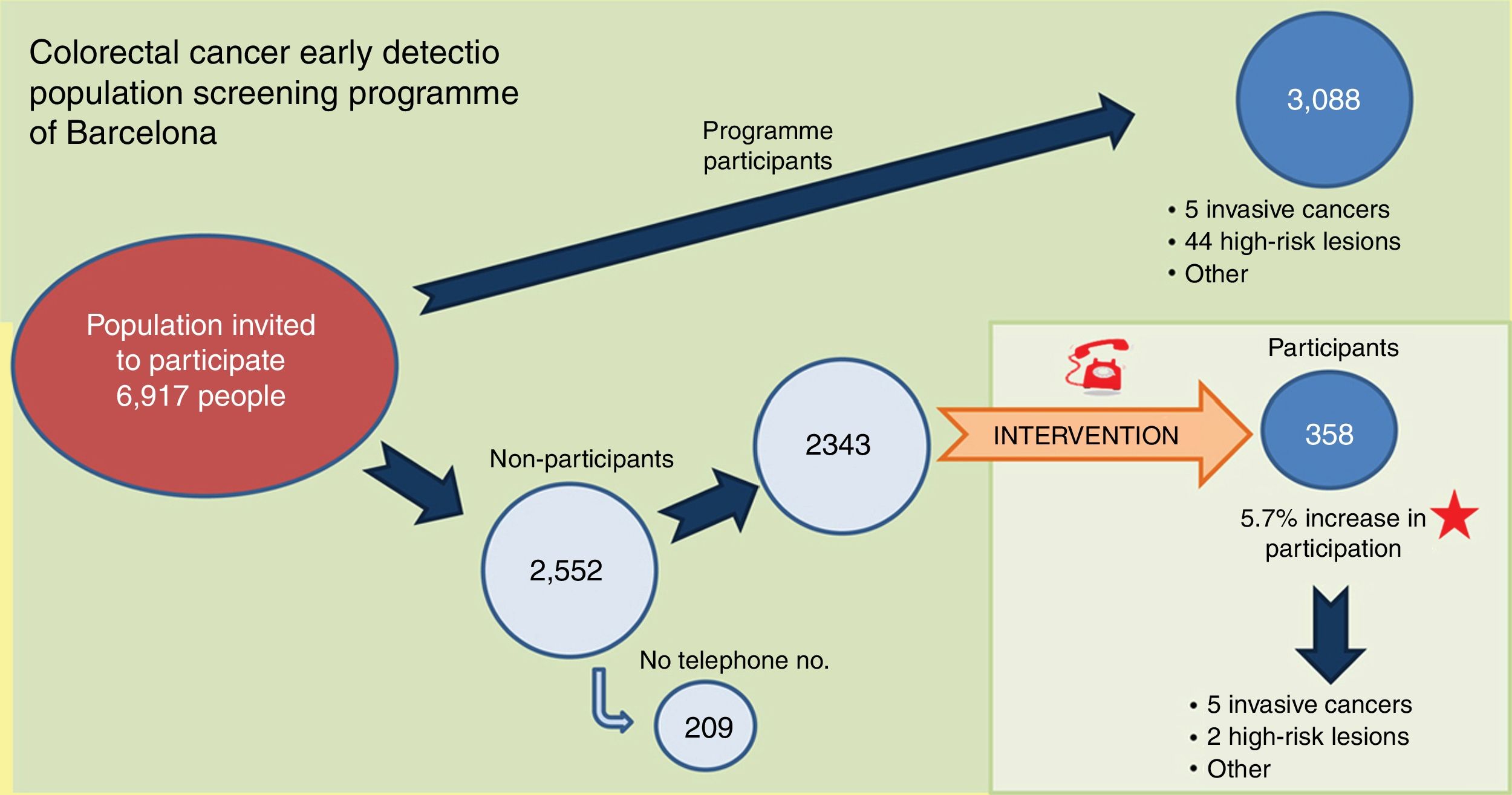
ResultsWe made 3327 phone calls to 2343 people. After the intervention the participation rate was 54.9%, which meant an increase of 5.7% with respect to the participation in the usual protocol for the programme (49.2%). The intervention allowed 5 cancers, 2 high-risk neoplasms and 8 low- and intermediate-risk lesions to be diagnosed. An average of 9 phone calls was necessary to achieve the participation of one additional person.
DiscussionThe telephonic intervention performed by primary care professionals has significantly increased the population participation rate and the detection of neoplasms with respect to the usual colorectal cancer early detection programme protocol.
Evaluar la efectividad de una entrevista telefónica realizada por profesionales de Atención Primaria en personas no participantes en la primera ronda del Programa de detección precoz de cáncer colorrectal (PDPCCR), en el área básica de salud (ABS) urbana Guineueta de Barcelona (España).
Pacientes y métodosUn grupo de profesionales de Atención Primaria del ABS Guineueta contactó, mediante un protocolo de llamadas telefónicas estandarizadas, con personas que no atendieron la invitación a participar en la primera ronda del PDPCCR. Se analiza el impacto de esta intervención en la tasa de participación y las enfermedades detectadas.
ResultadosSe realizaron 3.327 llamadas telefónicas a 2.343 personas. Tras la intervención, la tasa de participación fue del 54,9%, lo que supone un incremento del 5,7% con respecto a la participación del protocolo habitual del programa (49,2%). Se han diagnosticado 5 cánceres, 2 neoplasias de riesgo alto y 8 lesiones de riesgo bajo e intermedio. En promedio, han sido necesarias 9 llamadas para conseguir la aceptación de una persona adicional.
DiscusiónLa intervención telefónica de los profesionales de Atención Primaria ha aumentado de forma significativa la tasa de participación de la población y la detección de neoplasias con respecto al protocolo habitual del PDPCCR.
Colorectal cancer (CRC) is the most prevalent type of cancer among the Spanish population and the second-leading cause of mortality.1 CRC screening by faecal occult blood testing has been shown both to be effective and cost-effective in reducing mortality and incidence by detecting cancers at an early stage, as well as high-risk lesions.2,3
CRC screening programmes are aimed at men and women over the age of 50 with no additional risk criteria. The European Union recommends faecal occult blood screening every two years.4 In line with these recommendations, in 2014 Spain added CRC population screening programmes to its Basic Portfolio of Healthcare Services.5
A high participation rate improves the effectiveness of screening programmes. The European Commission quality assurance guidelines deem 45% to be an acceptable level of participation and 65% desirable.6 Its implementation in Spain has been a gradual process, with different organisational methods used in each autonomous community.7–9 The main barriers to participation in colorectal screening programmes have been reported to be the male gender, older people, a lack of education, financial uncertainty, belonging to ethnic minorities, immigrants and the self-perception of being in good health.10
Several studies have shown that various reminder card designs, telephone calls or emails can increase participation in population screening programmes.11–13 The involvement of GPs both in informing users14,15 and in the invitation system could also improve screening acceptance.13,16,17
Based on the hypothesis that a telephone call from primary care professionals and sending a personalised letter to people who have not participated in a population screening programme improves the overall rate of participation and disease findings, we implemented an intervention in a basic urban health area (ABS) of the city of Barcelona.
The aim of this study was to assess the impact of an intervention implemented during the first round of the Barcelona colorectal cancer early detection population screening programme (PDPCCR) by primary care professionals. The intervention involved making telephone calls to those people who had failed to respond to the invitation, to incentivise their participation.
Patients and methodsIntervention implemented during the first round of the Barcelona colorectal cancer early detection population screening programme in the Basic Urban Health Area (ABS) of Guineueta, located in the Nou Barris district of Barcelona, with a target population of 6917 people.
Between February and April 2016, the population of the Guineueta ABS was invited to take part in the routine colorectal cancer early detection population screening programme of Barcelona,8 which involved an immunological faecal occult blood test (IFOBT) with a cut-off point of 100μg Hb/g conducted every two years, aimed at men and women between the ages of 50 and 69. The invitation was sent in the form of a letter issued by the programme administration. A second reminder letter was sent to those recipients who failed to confirm their participation within two months of receipt of the invitation. The letters are a technical requirement of the programme design as they feature a barcode to identify the person concerned and to trace the sample. The kits were delivered to, and collected from, any of the participating pharmacies of the ABS, which passed the activity-related information to the technical office on a daily basis.
Participants were informed of negative results by letter, while participants with positive results were offered a colonoscopy appointment at the patient's referral hospital.
Although primary care physicians are not directly involved in the programme, they are aware of the programme dates in their ABS thanks to a preliminary informative talk given to primary care personnel by the technical office, to enable them to inform their patients, if necessary.
Once screening has been performed, the primary care physicians are responsible for the clinical follow-up of at-risk patients. This structure has yielded good participation results18 as well as excellent satisfaction rates from the programme's target population.19
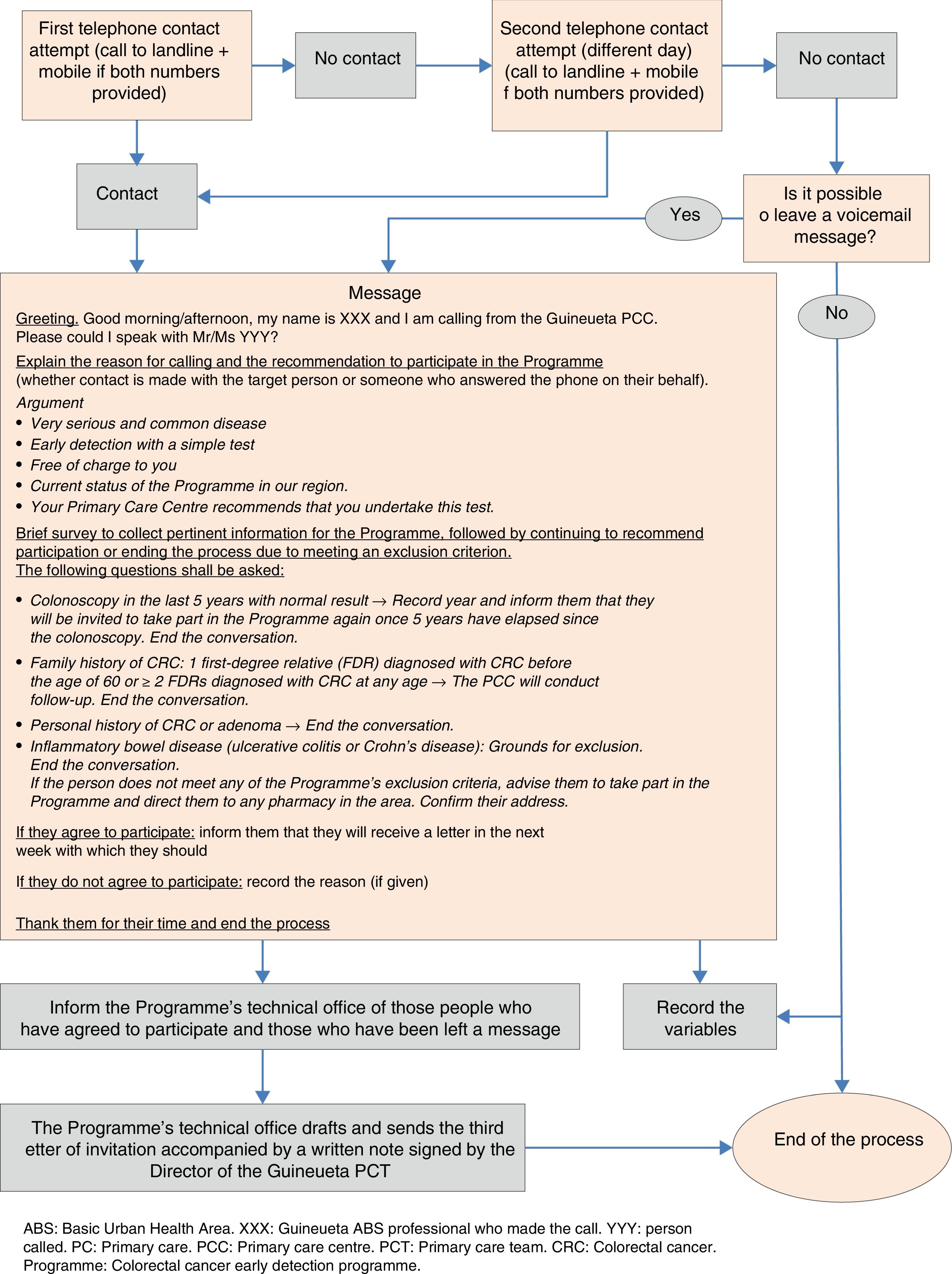
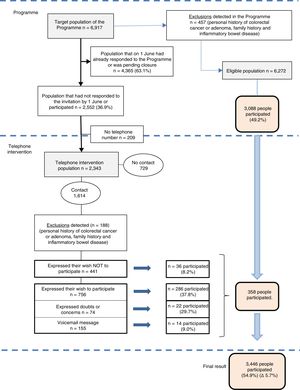
During the months of June, July and September 2016, four doctors, one nurse and an administrative assistant of the Primary Care Team (PCT) contacted people who did not respond to the programme invitation by means of a structured telephone interview (Fig. 1).
After the telephone call, the individuals were classified into three large groups:
- 1)
People who met the exclusion criteria of the CRC early detection population screening programme,8 who were recorded for subsequent verification by the programme's technical office.
- 2)
People who expressed their desire not to take part and provided reasons for their decision.
- 3)
People (or a family member who took the call) who expressed their desire to take part in the programme, who had some doubts or concerns or who could not be contacted directly but for whom a message was left on their voicemail or answering machine. As the team considered the likelihood of adherence to the programme to be high in these individuals, they were sent a third letter of invitation from the programme's technical office, together with a note signed by the Director of the Guineueta Primary Care Team highlighting the benefits of participating in the programme.
To assess whether the results obtained differed from other areas, they were compared with those obtained by the technical office of the other surrounding ABSs of the Nou Barris district with a similar socioeconomic status, included in the first round of the programme. The indicator used reflected the socioeconomic differences between ABSs and included: the percentage of the population with manual occupations, the percentage of the population with a low level of education, the early mortality rate, the rate of avoidable hospital admissions, the percentage of the population exempt from pharmacy copay, the percentage of the population with an annual income below 18,000 euros and the percentage of the population with an annual income above 100,000 euros.20
Two groups were created for data analysis purposes:
- 1)
“No intervention” (NoI), which included those people who responded to the programme invitation prior to implementation of the intervention (regardless of whether they participated or not), those who were still pending, programme exclusions detected and those without a valid telephone number.
- 2)
“Yes intervention” (YesI), which included those people who were telephoned.
The results are reported both for the target population as a whole, as well as for the aforementioned groups. The main indicators used were: exclusions (family history, personal history of adenoma or CRC and inflammatory bowel disease); temporary exclusion criteria (colonoscopy in the five years prior to or after receipt of the invitation by their primary care physician or another healthcare professional, whether for opportunistic screening or due to symptoms); a positive IFOBT; and results of the colonoscopy (negative, intestinal polyposis, inflammatory bowel disease, low-, intermediate- or high-risk lesions and invasive cancers). Non-invasive serrated lesions were included in the European guidelines for quality assurance risk groups.21
Bivariate analyses of the sociodemographic variables age and gender, and of the final statuses of the programme (“Participates”, “Does not participate” and “Exclusion”), were performed for each group. The chi-square test was used to compare categorical variables.
Logistic regression models were used to estimate the correlation between the sociodemographic factors age and gender, and participation.
The comparison was made with Guineueta's surrounding ABSs of a similar socioeconomic status.20 The main participation indicators and diagnosed disease were compared.
The statistical programme SPSS (version 23) was used for the analyses. A p-value <0.05 was considered to be statistically significant.
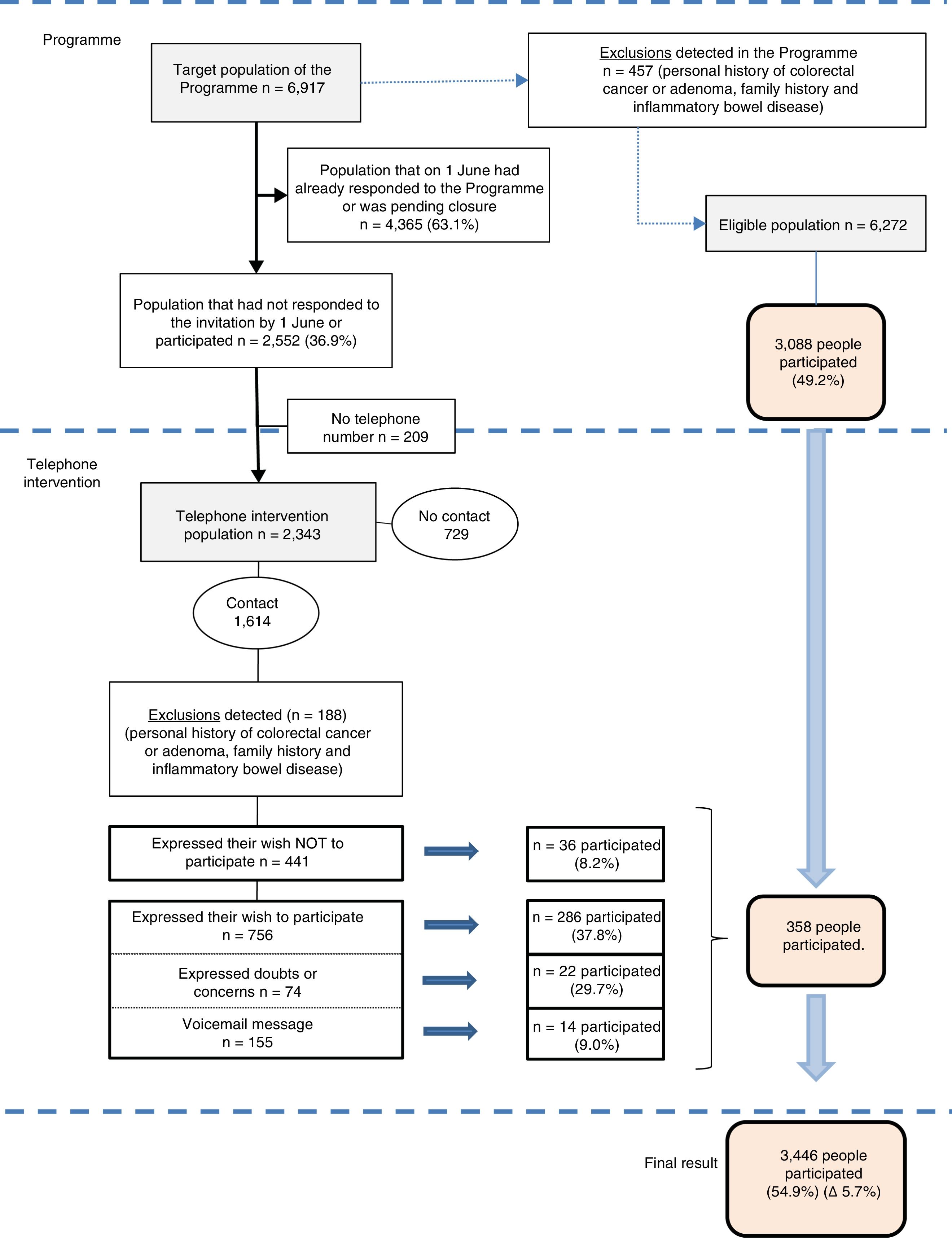
ResultsIn total, 3327 telephone calls were made to 2343 people who did not participate in the colorectal cancer early detection population screening programme (33.9% of the target population). Two or more calls were made in 1102 cases (47.0%).
A total of 1614 people (68.9%), with a mean age of 58.9 and with a similar male–female distribution (49.7% vs. 50.3%, respectively), were contacted by phone. A total of 188 people were excluded due to meeting the programme's exclusion criteria. The technical office sent a new letter of invitation to the 756 people who expressed their interest in participating, the 74 who expressed doubts or concerns and the 155 who were left a message on their answerphone (985 people in total), of which 322 ended up taking part. The rest (441 people) declined the invitation to participate, although 36 did end up taking part. One additional person participated in the programme for every nine telephone calls (3327 calls/358 additional participants) (Fig. 2).
A total of 729 people (31%) could not be contacted by phone, either because they did not answer (n=580) or because the telephone number recorded in the database was not valid (n=149) (data not shown).
29% (188/645) met the colorectal cancer early detection population screening programme exclusion criteria (Fig. 2), while almost 40% met the programme's temporary exclusion criteria (129/340) (Table 1).
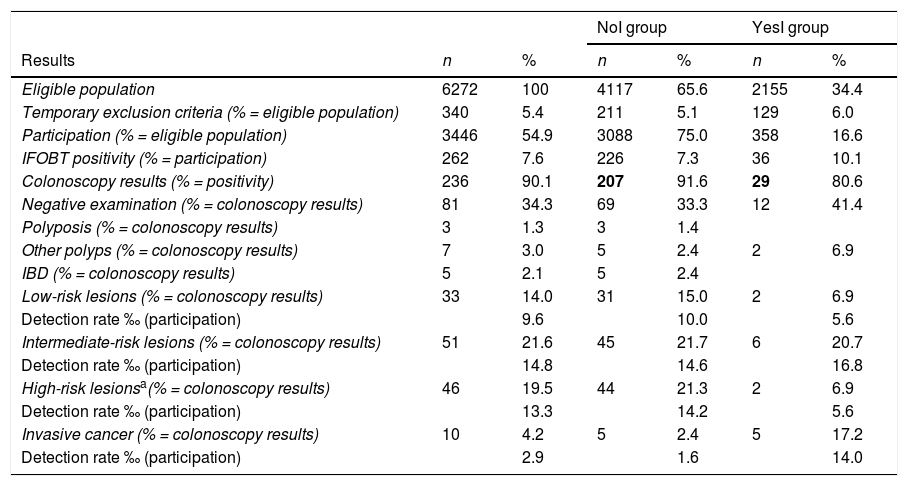
Description of the results of the programme as a whole and by group (no telephone intervention, yes telephone intervention).
| NoI group | YesI group | |||||
|---|---|---|---|---|---|---|
| Results | n | % | n | % | n | % |
| Eligible population | 6272 | 100 | 4117 | 65.6 | 2155 | 34.4 |
| Temporary exclusion criteria (% = eligible population) | 340 | 5.4 | 211 | 5.1 | 129 | 6.0 |
| Participation (% = eligible population) | 3446 | 54.9 | 3088 | 75.0 | 358 | 16.6 |
| IFOBT positivity (% = participation) | 262 | 7.6 | 226 | 7.3 | 36 | 10.1 |
| Colonoscopy results (% = positivity) | 236 | 90.1 | 207 | 91.6 | 29 | 80.6 |
| Negative examination (% = colonoscopy results) | 81 | 34.3 | 69 | 33.3 | 12 | 41.4 |
| Polyposis (% = colonoscopy results) | 3 | 1.3 | 3 | 1.4 | ||
| Other polyps (% = colonoscopy results) | 7 | 3.0 | 5 | 2.4 | 2 | 6.9 |
| IBD (% = colonoscopy results) | 5 | 2.1 | 5 | 2.4 | ||
| Low-risk lesions (% = colonoscopy results) | 33 | 14.0 | 31 | 15.0 | 2 | 6.9 |
| Detection rate ‰ (participation) | 9.6 | 10.0 | 5.6 | |||
| Intermediate-risk lesions (% = colonoscopy results) | 51 | 21.6 | 45 | 21.7 | 6 | 20.7 |
| Detection rate ‰ (participation) | 14.8 | 14.6 | 16.8 | |||
| High-risk lesionsa(% = colonoscopy results) | 46 | 19.5 | 44 | 21.3 | 2 | 6.9 |
| Detection rate ‰ (participation) | 13.3 | 14.2 | 5.6 | |||
| Invasive cancer (% = colonoscopy results) | 10 | 4.2 | 5 | 2.4 | 5 | 17.2 |
| Detection rate ‰ (participation) | 2.9 | 1.6 | 14.0 | |||
IBD: inflammatory bowel disease; NoI: no telephone intervention; programme: colorectal cancer early detection programme; YesI: yes telephone intervention.
Upon completion of the intervention, the participation rate was 54.9%, which represented a 5.7% increase on the participation achieved with the programme's standard protocol (49.2%). The IFOBT positivity rate was markedly higher in the YesI group than in the NoI group (10.1 vs 7.3%). With regards to the diagnosed disease, the detection rate of invasive cancers in the population as a whole was 2.9%, and this was also significantly higher in the YesI group than in the NoI group (14.0‰ and 1.6‰, respectively). The identification of 50% of the cancers was due to the intervention (n=5). There were no significant differences between the groups in terms of the diagnosis of other types of lesion of the colon (Table 1).
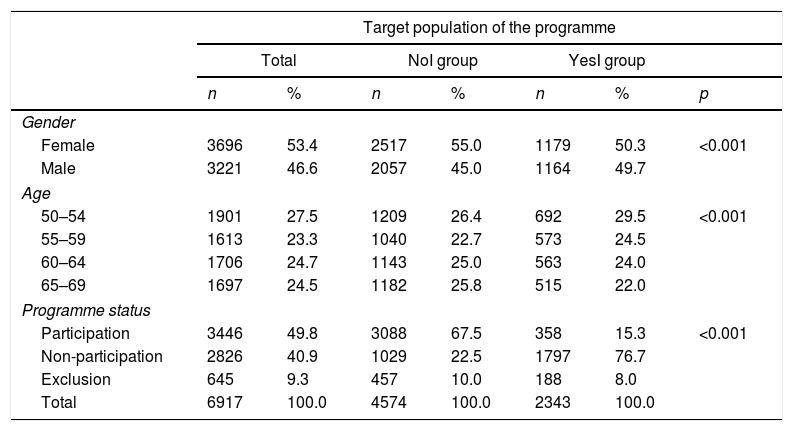
With regards to the sociodemographic variables, Table 2 shows that the characteristics of members of the NoI and YesI groups were significantly different. In terms of age, although almost no differences were found in the NoI group, in the YesI group, the number of people increased as age decreased (29.5% in the 50–54 age group vs 22.0% in the 65–69 age group).
Description of the sociodemographic characteristics age and gender, and of the final programme statuses (participation, non-participation and exclusion) by group (no telephone intervention, yes telephone intervention).
| Target population of the programme | |||||||
|---|---|---|---|---|---|---|---|
| Total | NoI group | YesI group | |||||
| n | % | n | % | n | % | p | |
| Gender | |||||||
| Female | 3696 | 53.4 | 2517 | 55.0 | 1179 | 50.3 | <0.001 |
| Male | 3221 | 46.6 | 2057 | 45.0 | 1164 | 49.7 | |
| Age | |||||||
| 50–54 | 1901 | 27.5 | 1209 | 26.4 | 692 | 29.5 | <0.001 |
| 55–59 | 1613 | 23.3 | 1040 | 22.7 | 573 | 24.5 | |
| 60–64 | 1706 | 24.7 | 1143 | 25.0 | 563 | 24.0 | |
| 65–69 | 1697 | 24.5 | 1182 | 25.8 | 515 | 22.0 | |
| Programme status | |||||||
| Participation | 3446 | 49.8 | 3088 | 67.5 | 358 | 15.3 | <0.001 |
| Non-participation | 2826 | 40.9 | 1029 | 22.5 | 1797 | 76.7 | |
| Exclusion | 645 | 9.3 | 457 | 10.0 | 188 | 8.0 | |
| Total | 6917 | 100.0 | 4574 | 100.0 | 2343 | 100.0 | |
NoI: no telephone intervention; programme: colorectal cancer early detection programme; YesI: yes telephone intervention.
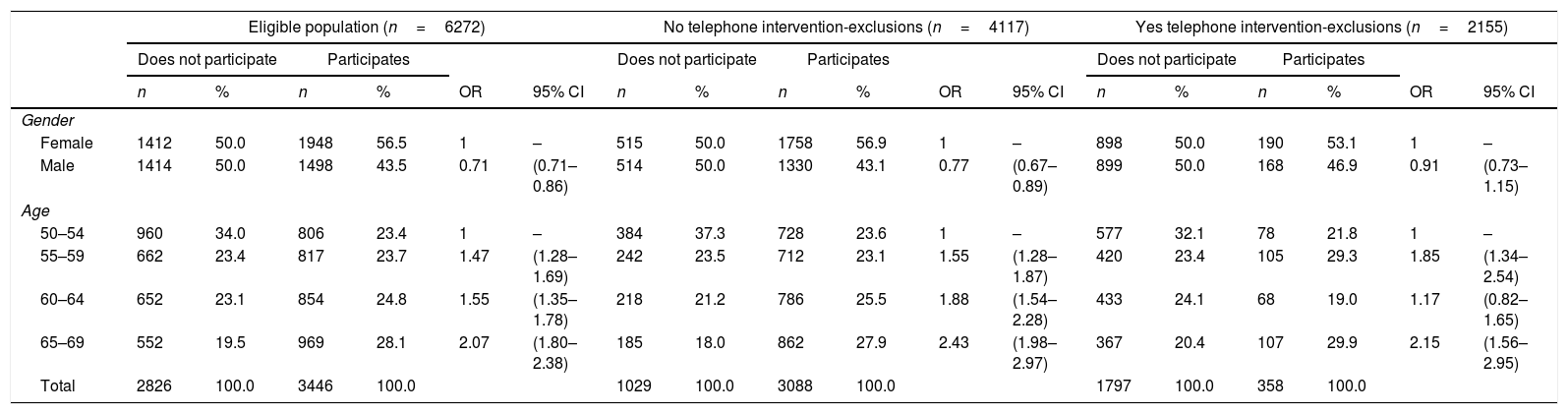
Considering gender and age (Table 3), fewer men were found to participate in the programme as a whole than women (RR=0.71; 95% CI: 0.71–0.86). Participation increased with age for both genders (1 in the 50–54 age group; 1.47 [1.28–1.69] in the 55–59 age group; 1.55 [1.35–1.78] in the 60–64 age group and 2.07 [1.80–2.38] in the 64–69 age group).
Logistic regression models of the correlation between the sociodemographic factors age and gender and participation by group (no telephone intervention, yes telephone intervention).
| Eligible population (n=6272) | No telephone intervention-exclusions (n=4117) | Yes telephone intervention-exclusions (n=2155) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Does not participate | Participates | Does not participate | Participates | Does not participate | Participates | |||||||||||||
| n | % | n | % | OR | 95% CI | n | % | n | % | OR | 95% CI | n | % | n | % | OR | 95% CI | |
| Gender | ||||||||||||||||||
| Female | 1412 | 50.0 | 1948 | 56.5 | 1 | – | 515 | 50.0 | 1758 | 56.9 | 1 | – | 898 | 50.0 | 190 | 53.1 | 1 | – |
| Male | 1414 | 50.0 | 1498 | 43.5 | 0.71 | (0.71–0.86) | 514 | 50.0 | 1330 | 43.1 | 0.77 | (0.67–0.89) | 899 | 50.0 | 168 | 46.9 | 0.91 | (0.73–1.15) |
| Age | ||||||||||||||||||
| 50–54 | 960 | 34.0 | 806 | 23.4 | 1 | – | 384 | 37.3 | 728 | 23.6 | 1 | – | 577 | 32.1 | 78 | 21.8 | 1 | – |
| 55–59 | 662 | 23.4 | 817 | 23.7 | 1.47 | (1.28–1.69) | 242 | 23.5 | 712 | 23.1 | 1.55 | (1.28–1.87) | 420 | 23.4 | 105 | 29.3 | 1.85 | (1.34–2.54) |
| 60–64 | 652 | 23.1 | 854 | 24.8 | 1.55 | (1.35–1.78) | 218 | 21.2 | 786 | 25.5 | 1.88 | (1.54–2.28) | 433 | 24.1 | 68 | 19.0 | 1.17 | (0.82–1.65) |
| 65–69 | 552 | 19.5 | 969 | 28.1 | 2.07 | (1.80–2.38) | 185 | 18.0 | 862 | 27.9 | 2.43 | (1.98–2.97) | 367 | 20.4 | 107 | 29.9 | 2.15 | (1.56–2.95) |
| Total | 2826 | 100.0 | 3446 | 100.0 | 1029 | 100.0 | 3088 | 100.0 | 1797 | 100.0 | 358 | 100.0 | ||||||
95% CI: 95% confidence interval; OR: adjusted odds ratio; programme: colorectal cancer early detection programme.
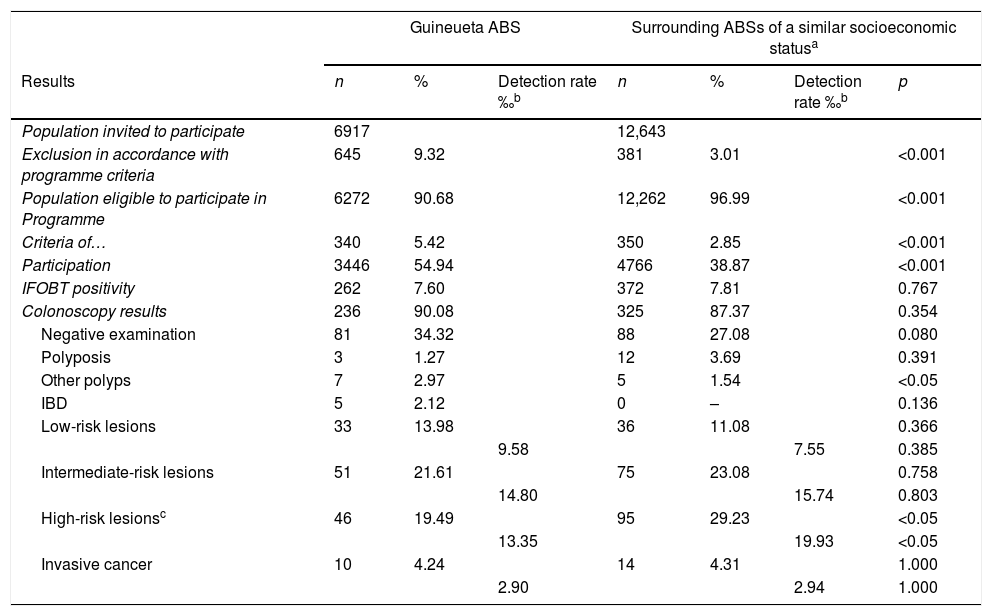
Upon comparison of the various indicators that affected participation (exclusions, temporary exclusion criteria and number of participants) of the ABS in question with the surrounding ABSs of similar socioeconomic status, significant differences in favour of the ABS in question were found in all cases. Specifically, participation in the Guineueta ABS was significantly higher than in the surrounding ABSs (54.9% vs 38.9%) (Table 4).
Comparison of Guineueta ABS with surrounding ABSs of a similar socioeconomic status.
| Guineueta ABS | Surrounding ABSs of a similar socioeconomic statusa | ||||||
|---|---|---|---|---|---|---|---|
| Results | n | % | Detection rate ‰b | n | % | Detection rate ‰b | p |
| Population invited to participate | 6917 | 12,643 | |||||
| Exclusion in accordance with programme criteria | 645 | 9.32 | 381 | 3.01 | <0.001 | ||
| Population eligible to participate in Programme | 6272 | 90.68 | 12,262 | 96.99 | <0.001 | ||
| Criteria of… | 340 | 5.42 | 350 | 2.85 | <0.001 | ||
| Participation | 3446 | 54.94 | 4766 | 38.87 | <0.001 | ||
| IFOBT positivity | 262 | 7.60 | 372 | 7.81 | 0.767 | ||
| Colonoscopy results | 236 | 90.08 | 325 | 87.37 | 0.354 | ||
| Negative examination | 81 | 34.32 | 88 | 27.08 | 0.080 | ||
| Polyposis | 3 | 1.27 | 12 | 3.69 | 0.391 | ||
| Other polyps | 7 | 2.97 | 5 | 1.54 | <0.05 | ||
| IBD | 5 | 2.12 | 0 | – | 0.136 | ||
| Low-risk lesions | 33 | 13.98 | 36 | 11.08 | 0.366 | ||
| 9.58 | 7.55 | 0.385 | |||||
| Intermediate-risk lesions | 51 | 21.61 | 75 | 23.08 | 0.758 | ||
| 14.80 | 15.74 | 0.803 | |||||
| High-risk lesionsc | 46 | 19.49 | 95 | 29.23 | <0.05 | ||
| 13.35 | 19.93 | <0.05 | |||||
| Invasive cancer | 10 | 4.24 | 14 | 4.31 | 1.000 | ||
| 2.90 | 2.94 | 1.000 | |||||
ABS: Basic Urban Health Area: IBD: inflammatory bowel disease; programme: colorectal cancer early detection programme.
No significant differences were detected in the IFOBT positivity rate, the percentage of colonoscopies performed, the results of the colonoscopies and the positive predictive values for IFOBT compared to the surrounding ABSs (except for inflammatory bowel disease and high-risk lesions) (Table 4). Fig. 3 summarises the most pertinent data obtained during the standard colorectal cancer early detection population screening programme and the intervention.
DiscussionThe telephone intervention increased participation in the colorectal cancer early detection population screening programme by 5.7%, achieved a higher invasive cancer detection rate than the standard programme and involved a use of resources that resulted in the participation of one person for every nine telephone calls.
The participation rate achieved after the intervention was 54.9%, which was higher than the programme implemented in the region of Aragon (45.3%)22 and higher than that achieved in other countries.23 However, with the introduction of immunological testing and the experience accrued, some programmes enjoy markedly higher participation rates, such as the Basque programme (68.4%),24 the British programme (66.4%)25 and the Danish programme (65.3%).26 In the city of Barcelona, the intervention resulted in a participation rate which was higher than the first round participation results published in other areas of the city (43.6%)18 and, as the study results show, higher than the participation achieved by the ABSs of the same district and round with a similar socioeconomic status.
This intervention suggests that telephone calls made by primary care professionals to incentivise participation, together with personalised letters, may effectively increase participation in a screening programme. These findings are similar to those reported in other studies involving a primary care intervention, whether multifaceted interventions that combine several strategies,27 specific strategies involving the direct intervention of professionals14,15,17,28 or the sending of reminder letters17,29 or emails.30
In terms of the profile of the participating population, the standard implementation of the programme saw more female and older participants, which is to be expected from CRC population screening programmes.18,25,31 However, the direct telephone call intervention was found to incentivise the participation of the younger population. Furthermore, people who participate at least once in a screening programme are more likely to participate in later rounds, meaning that this increase in the rate of participation may be maintained in the future.10,32
The results show that people who participated thanks to the primary care intervention had a markedly higher IFOBT positivity rate and cancer detection rate. With this in mind, the healthy volunteer bias that has been reported in the standard implementation of population screening programmes is worthy of mention,25,33 which posits that people who spontaneously agree to take part in a programme are better informed, are more concerned about their health and have healthier lifestyles. However, this intervention stimulated the participation of people with more risk factors for developing CRC. Despite this, no significant differences were found versus the surrounding ABSs of similar socioeconomic status in terms of the positive predictive value for cancer.
Neither the investment in terms of the working hours of the professionals to implement this intervention, nor the cost of sending 985 letters to the population that the study group deemed most likely to participate, have been calculated. However, the fact that the participation of one additional person was achieved for every nine telephone calls/2.7 letters (985/358) seems, a priori, to be an acceptable investment.
The main strength of the study is that it provides further evidence to support the positive impact that collaborative strategies involving primary care have on increasing participation in population screening programmes. It is also worth highlighting that the intervention doubled the number of invasive cancers detected compared to the normal programme, with the health benefits that this could entail. However, it also detected a significant number of people who met the programme's exclusion criteria.
The main limitation of the study was the fact that the study design precluded us from ascertaining whether intervention by a doctor, nurse or administrative assistant was most effective. In addition, the time and resources used were not quantified, and a differential analysis of the effectiveness of the letter versus the telephone call was not performed.
ConclusionsTelephone calls made by primary care professionals may help to increase participation in CRC screening programmes. The high prevalence of advanced cancers identified amongst the population that declined the initial invitation justifies the implementation of new strategies to encourage this group to participate in population screening programmes.
Authors/contributorsF.J. Luque-Mellado, J. Grau Cano, I. Condomines-Feliu and Lidia Paino-Pardal were responsible for the conception and design of the study. The initial population data were worked on and subsequently contributed by J. Grau Cano and I. Torá Rocamora. F.J. Luque-Mellado, I. Condomines-Feliu, M. Cuadras-Rofastes, M. Pacheco Ortiz and L. Paino-Pardal were responsible for contacting the target population, the telephone calls, incentivising participation and data collection, with each author making in excess of 500 telephone calls. From the programme itself, Elvira Romero Díaz and Juan Carlos Camuñez Bravo sent the third letters and verified the exclusions reported from the implementation of the intervention. J. Grau Cano and I. Torá Rocamora compiled the information and researched the associated references. I. Torá Rocamora conducted the analysis of the information obtained and the other authors made subsequent contributions. Various sections of the manuscript were drafted by F.J. Luque-Mellado, J. Grau Cano, I. Torá Rocamora, I. Condomines-Feliu and L. Paino-Pardal. All the authors critically reviewed the manuscript, with significant intellectual contributions, and approved the final version. The authors also take responsibility for, and declare that the various aspects that make up the manuscript were reviewed and discussed to ensure that they were expressed as fully and accurately as possible.
FundingThis research did not receive specific financial support from public sector agencies, the commercial sector or non-profit organisations.
Conflicts of interestNone.
To the PROCOLON research group for its continuous contribution to improving the programme: Rafael Abós-Herrándiz, Eva abril, Marta Aldea, Cristina Álvarez, Marco Antonio Álvarez, Montserrat Andreu, Isis Araujo, Josep M. Augé, Anna Aymar, Guillermo Bagaria, Francesc Balaguer, Xavier Bessa, Montserrat Bonilla, Andrea Burón, Sabela Carballal, Antoni Castells, Xavier Castells, Mercè Comas, Rosa Costa, Míriam Cuatrecasas, Josep M. Dedeu, Maria Estrada, Imma Garrell, Jordi Gordillo, Rafael Guayta, Cristina Hernández, Mar Iglesias, Laura Llovet, María López-Cerón, Francesc Macià, Leticia Moreira, Laura Moreno, M. Francisca Murciano, Gemma Navarro, Teresa Ocaña, Maria Pellisé, Mercè Pintanell, Ángels Pozo, Teresa Puig, Faust Riu, Liseth Rivero-Sánchez, Cristina Rodríguez, María Sala, Ariadna Sánchez, Agustín Seoane, Anna Serradesanferm, Judit Sivilla, Antoni Trilla.
To the applicable members of the technical office and the primary care professionals who participated, for their collaboration and dedication to the implementation of this intervention.
Please cite this article as: Luque Mellado FJ, Paino Pardal L, Condomines Feliu I, Tora-Rocamora I, Cuadras Rofastes M, Romero Díaz E, et al. Impacto de una intervención de Atención Primaria en el programa de detección precoz de cáncer colorrectal. Gastroenterol Hepatol. 2019;42:351–361.