Children with Autism Spectrum Disorder (ASD) frequently experience significant behavioral challenges that hinder adaptive functioning and increase caregiver stress. This study assesses the feasibility, acceptability, and preliminary efficacy of a telehealth-delivered group parent training program designed to address behavioral difficulties in children with ASD.
MethodAn open-label, single-arm trial was conducted with children aged 3–12 years diagnosed with ASD and behavioral difficulties, recruited from a tertiary hospital’s autism care program. Program effectiveness was evaluated using parent-reported measures on their children and on themselves assessing behavior problems, parental stress, and quality of life. Data analysis included pre-post comparisons and follow-up assessments at 3 and 6 months.
ResultsTwenty dyads parent-children were analyzed. Satisfaction with the program was moderate, with especially favorable feedback on the "planned ignoring" unit. Preferences for delivery mode and format varied, with suggestions to reduce the number of tasks and tailor content to individual needs. Significant reductions in irritability, lethargy, hyperactivity were observed immediately after treatment, with improvements in irritability and hyperactivity sustained at the 3- and 6-month follow-ups. Parental stress decreased significantly post-treatment but did not persist over time. Quality of life improved significantly compared to baseline, both immediately post-treatment and during follow-up evaluations.
ConclusionsThe telehealth-delivered group parent training program demonstrated feasibility and moderate acceptability, with significant improvements in child behavior and caregiver quality of life. However, the reduction in parental stress was not sustained over time. These findings underscore the potential of telehealth-delivered group interventions for managing ASD-related behavioral issues and indicate areas for program refinement to enhance adherence and long-term effectiveness.
Autism Spectrum Disorder (ASD) is a chronic neurodevelopmental condition that emerges in early childhood, characterized by deficits in social communication, restricted interests, and repetitive behaviors.1 According to a recent meta-analysis, nearly one in 100 children is diagnosed with ASD, with a significantly higher prevalence in males—up to four times more common than in females.2 However, this disparity may be influenced by challenges in identifying autistic profiles in females3,4 .
Individuals with ASD have a significant prevalence of co-occurring mental health disorders.5,6 The most common in children with ASD are Attention Deficit Hyperactivity Disorder (ADHD), conduct disorders, depressive symptoms, and anxiety disorders.7,8 The severity of these concurrent conditions is as high as in clinical samples without ASD.9 Additionally, children with ASD are more likely to exhibit internalizing and externalizing symptoms compared to neurotypical children,10 which can negatively interfere with their adaptive functioning.11 Regarding externalizing symptoms, aggression and hyperactivity occur more frequently in children with ASD than in those without ASD.12 It is estimated that around 30–50 % of children with ASD exhibit such behavioral disturbances.13,14 Additionally, it has been found that approximately one in four children with ASD meets the diagnostic criteria for oppositional defiant disorder or conduct disorder.11 It has been observed that children with ASD who display aggressive behavior are five times more likely to be hospitalized than those who do not exhibit such behavior, leading to increased medication use, symptom intensification, and worsening adaptive functioning.15 Furthermore, these behaviors can impact caregiver stress levels,16–19 especially when these behaviors persist over time and reinforce parents' feelings of incompetence in managing the situation.20 In this regard, a reduction in caregiver stress has been associated with behavioral improvements in the child,21,22 with a bidirectional relationship observed.23 Similarly, persistent behavioral challenges in children with ASD can negatively affect family finances, not only due to the high cost of specialized treatments but also because it can compromise work-life balance, as these children require greater attention from their caregivers.19,24 For this reason, the need for evidence-based treatment programs that minimize the risks associated with the chronicity of such behaviors in children with ASD has been highlighted.25
Parent training for children with ASD and behavioral difficultiesIn the context of behavioral interventions for ASD, parent training (PT) has gained increasing recognition as a critical component in the treatment of children with autism. PT interventions are designed to empower parents with the necessary skills and strategies to manage and modify their child's challenging behaviors effectively. Supporting this approach, a recent meta-analysis by Cheng et al.26 found evidence of the efficacy of PT in reducing disruptive behavior and enhancing positive or adaptive behaviors in children with ASD. The authors concluded that future research should focus on ensuring proper implementation of these programs in clinical settings. The literature also suggests that PT significantly reduces child behavior problems and parental stress, in addition to improving parental competence.17,20,26 In this regard, specific PT programs have been designed for children diagnosed with ASD, aimed at teaching specific skills to reduce and prevent disruptive behavior and promoting adaptive behaviors. The Research Units in Behavioral Intervention Parent Training for Disruptive Behavior (RUBI-PT)27,28 is a structured protocol based on the principles of applied behavior analysis, designed to guide therapists in teaching parents practical strategies to help manage their child's disruptive behavior in natural environments. The RUBI-PT is a manualized PT program developed by the Autism Network of the Research Units on Behavioral Intervention, specifically for parents of children with autism.27 The treatment includes 11 core sessions, 7 supplemental sessions, a home visit, and follow-up phone sessions. Each session includes a therapist script, activity sheets, a parent booklet, and treatment fidelity checklists. Additionally, video sequences accompany each main session, which therapists use to demonstrate the concepts taught, and parents are given homework between sessions. It is the first PT program specifically developed for parents of children with ASD that has demonstrated efficacy in reducing challenging behaviors,28 significant improvements in adaptive functioning,29 and improvements in eating behavior and sleep routines.30,31 However, these types of interventions require a considerable amount of time (12–24 weeks or more) and can lead to significant participant fatigue.28 Therefore, group-based face-to-face interventions have been implemented.13,32 Specifically, Burrell et al.13 conducted an intervention based on RUBI-PT, applying it in a group-based face-to-face format (RUBI-GPT) with parents of children aged 3 to 8 years with ASD and disruptive behaviors. RUBI-GPT lasted 24 weeks and included 10 group sessions, 1 individual parent-child session, and 1 supplemental session addressing issues such as feeding, hygiene, and sleep. Similarly, Rohacek et al.32 conducted a group-based face-to-face intervention based on Behavioral Parent Training (BPT) aimed at reducing challenging behaviors in children with ASD aged 5 to 9 years. This intervention consisted of 6 group sessions, with 38 caregivers randomly assigned, of which 29 completed BPT. Both studies reported a reduction in disruptive behaviors in children with ASD.
Telehealth-delivered parent training for children with ASD and behavioral difficultiesTelehealth refers to the provision of healthcare services through technological resources that optimize care, saving time and costs, and increasing accessibility.33 According to a review,34 telehealth has the potential to reduce barriers to intervention access, and recent findings indicate it is highly promising in terms of feasibility and efficacy.35 This type of intervention modality is particularly relevant in contexts where access to treatment is limited by geographical factors (e.g., rural areas)36; or for families with low socioeconomic status, who not only face structural barriers to care but also have less knowledge of available services37; or due to time constraints (e.g., balancing work and family life with access to intervention) .34 Additionally, technology is becoming more accessible and affordable, as younger generations of parents are increasingly knowledgeable and interested in this method of service delivery.
Regarding telehealth-delivered interventions, Comer et al.35 conducted the first controlled trial examining telehealth for delivering PT to families of neurotypical children. Following positive treatment response outcomes, the authors highlight the promising role of new technologies in expanding PT for behavioral management of their children. Despite strong evidence supporting the efficacy of PT in managing behavior problems in the ASD population, existing studies on telehealth interventions are limited. In this regard, Ros-DeMarize et al.38 found that families are interested in this type of treatment and its different formats, both online and group-based. Recent studies highlight the feasibility and effectiveness of telehealth PT for managing behavioral difficulties in children with ASD. For example, single-arm open-label trials implemented telehealth-delivered individual RUBI-PT with high therapist fidelity and promising outcomes, including reduced child behavior problems and improved caregiver well-being.(27,39–41) These studies, often conducted in underserved or rural populations, reinforce the feasibility and acceptability of one-on-one PT via synchronous telehealth sessions.
In parallel, group-based PT programs delivered face-to-face have proven effective in improving behavior in children with ASD,13 as well as parent-related aspects such as stress, anxiety, and depression,42 with reports of high satisfaction and acceptability in addressing their children's challenging behaviors.32 Moreover, this format promotes perceived acceptance and support from other parents, potentially reducing feelings of guilt, social isolation, and increasing confidence in managing their children's behavior.43 However, few studies have evaluated the efficacy of telehealth in group settings for families of children with ASD. A few studies have begun to address this gap. Kuravackel et al.44 and Dahiya et al.36 evaluated the CHOPE program, which combined individual and group sessions delivered either via telehealth or in-person. Both non-randomized comparison studies reported significant improvements in child behavior and parenting outcomes across settings, with comparable effects in urban and rural samples. More recently, a non-randomized comparison study by Graucher et al.45 assessed group-based RUBI-PT delivered both virtually and face-to-face, finding reliable improvements in behavior across formats in a diverse sample. Together, these findings highlight the potential of PT interventions, particularly those utilizing telehealth, to meet the needs of families in diverse and underserved settings while effectively addressing challenging behaviors in children with ASD. See Appendix 1 for a summary of studies on telehealth-delivered PT interventions for children with ASD and behavioral challenges.
In light of the limited evidence and existing gaps in the scientific literature, this study presents the BEHAVE Academy, a telehealth-delivered group PT program specifically designed for families and caregivers of children with ASD. The primary objective is to evaluate the acceptability, feasibility, and preliminary efficacy of this intervention in reducing disruptive behaviors, with a focus on both child and family outcomes. Furthermore, the study aims to assess the long-term sustainability of these improvements through follow-up evaluations conducted several months after the intervention. To our knowledge, this is the first study to evaluate a fully remote, group-based parent training program for autism in Spanish, with follow-up extending to 6 months.
MethodsStudy designThe present study is designed as an open-label, single-arm trial, meaning that all participants receive the same intervention without randomization to different groups, and both the researchers and participants were aware of the treatment being administered. This design allows for a focused evaluation of the feasibility, acceptability and preliminary efficacy in a real-world setting, that can inform future controlled studies.
ParticipantsParticipants were recruited from an ASD care program within the mental health service of a tertiary hospital, specifically targeting those undergoing diagnostic evaluations. The study included children who met the following criteria: (i) aged 3 to 12 years at baseline, (ii) a confirmed clinical diagnosis of ASD, and (iii) exhibiting challenging or behavioral difficulties defined as recurrent aggression, tantrums, and noncompliance in home or educational settings. Children were excluded if they (i) were concurrently enrolled in other PT programs at baseline or (ii) experienced changes in psychotropic medication during the study period (9 months) in order to reduce confounding and ensure that observed changes could be attributed to the intervention. Caregivers were required to provide informed consent and have access to high-speed internet for participation, with no additional inclusion or exclusion criteria applied to them. Given the feasibility nature of the study, no formal power calculation was performed. Instead, the sample size was determined based on practical considerations and availability of participants during the recruitment period.
InstrumentsThe evaluation instruments utilized in this study primarily consisted of parent-reported measures on their children and on themselves designed to assess key variables, including the behavioral problems of children diagnosed with ASD, as well as the stress and quality of life of their primary caregivers. Caregivers were required to have sufficient proficiency in Spanish to understand the materials and complete the questionnaires. The assessment battery comprised the following:
Ad hoc demographic and clinical questionnaire: This instrument collected various socio-demographic and clinical data including age, sex, psychiatric history, and psychopharmacological treatment details (including dosage). Additionally, information regarding the caregiver(s) participating in the online training, such as their relationship to the child, age, sex, academic/work status, and the socio-economic status of the family unit, was recorded.
Intervention fidelity was systematically assessed by therapists who completed structured checklists at the conclusion of each therapeutic session. To further evaluate adherence, attendance records and the completion of assigned tasks were reviewed at the beginning of each session. The acceptability of the intervention was gauged using a custom-designed Likert-type Parent Survey. This survey employed a four-point response scale (0 = not at all, 1 = a little, 2 = somewhat, 3 = very much), where participants were asked to select the option that best represented their views across four key domains of the intervention: satisfaction, goal-achievement, potential, and cost-benefit. Each domain consisted of three items, and domain scores were summed to yield an overall acceptability score. The interpretation of scores was as follows: 0–3 = Not valid, 3–6 = Slightly valid, 6–9 = Moderately valid, and 9–12 = Strongly valid. Participants were also surveyed on their preferences regarding the intervention's delivery method (face-to-face vs. telehealth) and format (individual vs. group). Additionally, they provided qualitative feedback through an open-ended question concerning potential modifications to the intervention. The utility of each component of the program was evaluated by an open-ended question and by using a four-point Likert scale (Not useful, Somewhat useful, Useful, Very useful). The perceived cost-benefit ratio of the intervention was evaluated from the parental perspective, focusing on the subjective balance between the time and effort required to participate and the perceived benefits for the child and family. These perceptions, along with preferences regarding the mode of delivery (telehealth vs. face-to-face), were collected post-intervention, after parents had completed the full program. Information about previous participation in behavioral or parenting interventions was not collected in this study.
Aberrant Behavior Checklist (ABC): This 58-item caregiver-completed questionnaire assesses behavioral difficulties in individuals with neurodevelopmental disorders using a four-point rating scale (0–3), where higher scores indicate more severe problematic behaviors.46 The ABCC includes five subscales: Irritability/Agitation/Crying, Lethargy/Social Withdrawal, Stereotypic Behavior, Hyperactivity/Noncompliance, and Inappropriate Speech.47 The tool has demonstrated excellent reliability, with internal consistency ranging from 0.83 to 0.9, test-retest reliability between 0.59 and 0.94, and established validity.11,46,48 Widely used in clinical trials, the ABCC is sensitive to treatment effects, particularly the Social Withdrawal subscale, in ASD populations.49
Home Situations Questionnaire - Autism Spectrum Disorder (HSQ-ASD): Originally designed to assess noncompliance in children with disruptive behavior disorders, this modified version for ASD includes 24 dichotomous (yes/no) items, where parents indicate whether their child experienced difficulty following instructions or rules in daily routine situations over the past four weeks. Severity is rated on a 1–9 Likert scale, with higher scores indicating greater severity (Burrell et al., 2020). Factor analysis identified two subscales—Social Inflexibility (α = 0.84) and Specific Demand (α = 0.89)—with significant test-retest reliability.50 The questionnaire also demonstrated convergent validity with other criterion measures.41
Parental Stress Index - Short Form (PSI-SF): Adapted for parents of children up to 12 years old, the PSI-SF assesses parental stress through 36 items rated on a five-point Likert scale. The index includes three subscales: Parental Distress, Parent-Child Dysfunctional Interaction, and Difficult Child Scale, with higher t-scores indicating greater stress, particularly at clinically significant levels (t ≥ 85) .51 The PSI-SF has shown reliability (α = 0.80–0.87) in typically developing populations. Zaidman-Zait et al.52 confirmed the tool's sensitivity to changes in parental distress severity among parents of young children with ASD.
Pediatric Quality of Life Inventory – Family Impact Module (PedsQL-FIM): This 36-item tool measures family quality of life across subscales for physical, emotional, social, and cognitive functioning, as well as communication, worry, daily activities, and family relationships. Scores are transformed into a 0–100 scale, where higher scores indicate better functioning.53,54 The PedsQL Family Impact Module has demonstrated high internal consistency (α ≥ 0.90) across studies, including those involving children with ASD.55
ProcedureThe study was conducted between January 2022 and December 2023 at a tertiary care center in Barcelona, Spain. Recruitment and intervention were conducted as part of routine clinical practice. Eligible families were provided with an information sheet and received both oral and written explanations of the study procedures. Those who agreed to participate gave informed consent in accordance with ethical guidelines. Any doubts about the informed consent were clarified. The intervention was delivered in 10 separate groups, each composed of three to five families, and led by two licensed therapists with at least 5 years of experience in behavioral intervention. The study utilized a single-group design with pre-post measurements, evaluating at four time points: Pre-training (two weeks before the intervention); Post-training (two weeks after the intervention); First follow-up (3 months after the intervention); Second follow-up (6 months after the intervention). A code was assigned to each participant for data collection and subsequent analysis. Data were collected via the REDCap platform56 on the servers of the hospital’s research institute website, accessible only to the study researchers. Approval for the study was obtained from the center’s clinical research ethics committee, and all participants gave written informed consent after receiving full information.
InterventionThe intervention design followed a structured plan, beginning with a pilot online group using the RUBI-PT program, involving four families with children diagnosed with ASD and behavioral problems. The program consisted of 12 weekly sessions, during which a therapist introduced the program content, with intersession tasks that included completing behavior logs and applying strategies discussed in the sessions. A qualitative evaluation assessed participant satisfaction with the session content, online attendance, and intersession task completion. The evaluation findings indicated that while the program was generally well-received, the weekly session frequency was deemed excessive. Many families reported difficulties in attending sessions due to scheduling conflicts. Furthermore, challenges were noted in understanding the theoretical content, which, though considered valuable, was perceived as complex. Additionally, the analysis revealed that the strategy of planned ignoring was often ineffective in many recorded instances. The behavioral difficulties observed were not primarily attention-seeking but were more indicative of emotional dysregulation, suggesting that co-regulation strategies by parents/caregivers were more appropriate in these cases.
In the subsequent phase, the Behavioral and Emotion Handling for Autism: A Video Education Academy (BEHAVE Academy) program was developed. This program comprises 10 webinars (each approximately 20–45 min in duration) that address common behavioral challenges in children with ASD. The webinars provide caregivers with strategies to manage behavioral difficulties that interfere with adaptive functioning, utilizing audiovisual examples created specifically in Spanish for this intervention (see Table 1). The webinars are distributed to families biweekly, in sets of two webinars each time, alongside written assignments that involve exercises mirroring the scenarios presented in the webinars. Families are also required to complete behavior logs, documenting the function of the observed behavior and the strategies employed to address it. Furthermore, the program includes five biweekly support sessions, each lasting 90–120 min, designed to clarify doubts and reinforce the application of behavioral techniques with a therapist specializing in ASD. Importantly, the BEHAVE Academy program incorporates a dedicated module focusing on emotional regulation, recognizing that children and adolescents with ASD frequently exhibit deficits in this area,57 which may contribute to heightened emotional responses and, consequently, the emergence of aggressive, disruptive, and challenging behaviors.58
Overview of the BEHAVE Academy program.
The data analysis aimed to evaluate the impact of the BEHAVE Academy Program on key dependent variables, specifically focusing on behavioral changes in children with ASD and the stress levels and quality of life of their primary caregivers. A within-subject pretest-posttest design was employed, incorporating comparisons from Baseline across three follow-up points: post-intervention (T1), 3-month follow-up (T2), and 6-month follow-up (T3). This methodology was selected to address repeated measurements taken before and after the intervention and to assess the program’s efficacy in mitigating problematic behaviors, reducing parental stress, and enhancing caregivers' quality of life. Statistical analyses included non-parametric repeated measures tests. Effect sizes were calculated using Cohen’s d (interpreted as 0.01 = very small, 0.20 = small, 0.50 = medium, 0.80 = large, 1.20 = very large, and 2.0 = huge effects). Additionally, an intent-to-treat (ITT) analysis was conducted for all participants who completed the baseline assessment, regardless of program completion status, utilizing the last observation carried forward (LOCF) method to handle missing data where applicable. Finally, responses from a self-administered questionnaire were analyzed to gauge participant satisfaction and perceived benefits of the program. No correction for multiple comparisons was applied, given the exploratory nature of the study. All analyses were conducted with a significance level set at α = 0.05.
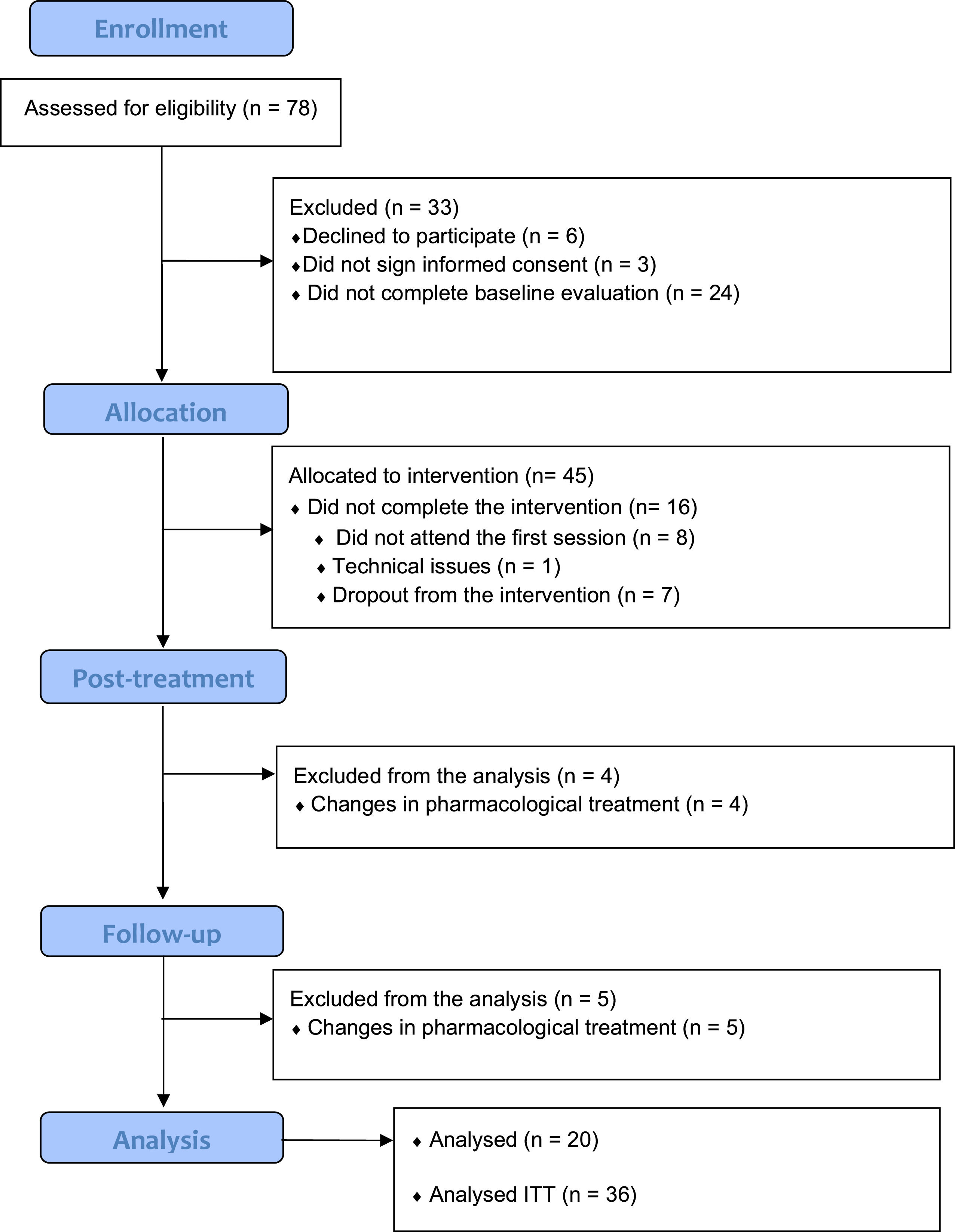
ResultsInitially, 78 families with children diagnosed with ASD and behavioral difficulties were invited to participate in the study. Of these, 45 consented to participate. However, 16 participants (36 %) did not complete the intervention. Among these, eight participants (18 %), despite completing the baseline evaluation, signing the consent form, and receiving the first two webinars, did not attend the initial online session. One participant (2 %) experienced technical difficulties during the first session and chose not to continue, while seven participants (16 %) withdrew during the intervention. Specifically, five participants attended two online sessions and viewed the first four webinars, one attended three sessions and watched the first six webinars, and one attended the first session and viewed only the first two webinars. Additionally, nine participants (20 %) modified their pharmacological treatment during the study and were excluded from the final analysis. As a result, the final dataset comprised 20 participants. Concerning missing data, one participant (5 %) had incomplete data at T2, and five participants (25 %) had incomplete data at T3; the Last Observation Carried Forward (LOCF) method was used to address these gaps. A detailed participant flowchart is presented in Fig. 1.
Feasibility and acceptabilityTherapists maintained a high level of fidelity to the intervention protocol, achieving a success rate of 98 %. Parents also demonstrated strong adherence to the treatment protocol, with attendance rates of 100 %, completion of inter-session tasks at 95 %.
At the end of the intervention, 22 participants (14 completers and 8 excluded because pharmacological treatment change) completed the Parent Survey. The average satisfaction score was 7.77 (SD = 1.45, range = 3–9), indicating moderate satisfaction with the intervention. Participants reported a near-to-moderate sense of goal achievement (M = 5.68, SD = 1.67, range = 2–8) and a moderate sense of empowerment concerning the maintenance of improvements and prevention of relapses (M = 8.00, SD = 1.2, range = 5–9). The intervention was also perceived as having a favorable cost-benefit ratio (M = 6.55, SD = 2.00, range = 3–12). A statistically significant difference was observed between completers and excluded participants in terms of goal achievement (z = −2.17, p = 0.03). Specifically, completers reported a significantly higher perception of having achieved their pre-established goals by the conclusion of the intervention. Regarding setting preferences, 46 % of participants indicated a preference for telehealth sessions, 14 % favored face-to-face sessions, and 40 % expressed no preference regarding the delivery mode. In terms of session format, 50 % preferred a group format, 10 % opted for individual sessions, and 40 % were indifferent. The "planned ignoring" module was rated as very useful by 80 % of participants, making it the most highly valued component. Other highly valued components included behavioral principles, management of reinforcers, prevention strategies, giving directions, and modeling, each rated as very useful by 60–65 % of participants. Emotional regulation, asking for help, chaining, following instructions, token economy, generalization, and maintenance were rated as very useful by 50–55 % of participants. In contrast, the unit on visual schedules was rated as very useful by only 40 % of participants, and behavioral logs received a very useful rating from 45 % of participants. Participant feedback frequently noted benefits such as enhanced understanding of the causes of behavioral difficulties in their children (“I have been able to understand the needs and how to redirect my child's behaviors”), increased self-competence and emotional balance (“It has helped me react to my child's current behaviors and to handle future behaviors as they arise, gain confidence, and not feel lost. It has been a tremendous help, not only in providing the right tools but also in helping my emotional balance, as what I didn't understand or thought had no solution now does, with work, patience, and routine”), and the value of connecting with others in similar situations (“Being able to resolve doubts about specific cases and hear about the cases presented by others. It has also helped me know that there are more people going through similar situations”). Suggested changes to the intervention primarily focused on reducing the number of inter-session tasks (“I would reduce the number of tasks, especially in the first two units”) and addressing the diverse profiles of children (“The intervention covers children with ASD of all types; some techniques require a minimum understanding by the child. It would be better to divide parents based on their children’s specific needs”).
Socio-demographic and clinical measuresTable 2 summarizes the demographic and clinical characteristics of completers (n = 20) and non-completers (n = 16). Both groups were comparable in terms of child age, sex, neurodevelopmental comorbidities, and psychotropic medication use. No statistically significant differences were found in any baseline clinical measures. Although some differences were observed in caregiver education and income levels, these differences were not statistically significant. Detailed values are provided in Table 2.
Demographic and clinical characteristics of the participants.
The results demonstrated significant improvements across several subscales of the ABC following treatment, with some effects persisting over time (see Fig. 2). In the Completers Analysis, there was a notable reduction in irritability from baseline (M = 13.20, SD = 9.81) to post-treatment (M = 9.45, SD = 5.98), which was statistically significant (z = −2.12, p = 0.03, d = −0.47). Lethargy also showed a significant decrease from baseline (M = 7.90, SD = 5.05) to post-treatment (M = 5.30, SD = 5.14) (z = −2.28, p = 0.02, d = −0.51), and this reduction remained marginally significant at the three-month follow-up (z = −1.94, p = 0.05, d = −0.43). Hyperactivity decreased significantly from baseline (M = 19.85, SD = 11.34) to post-treatment (M = 14.65, SD = 8.88), (z = −2.94, p < 0.01, d = −0.66), and this improvement persisted at both the three-month (z = −2.44, p = 0.01, d = −0.55) and six-month follow-ups (z = −2.70, p = 0.01, d = −0.60). The total ABC score also showed a significant reduction from baseline (M = 48.45, SD = 26.63) to post-treatment (M = 35.85, SD = 17.52), (z = −2.65, p = 0.01, d = −0.56), and remained significantly lower at the three-month (z = −2.13, p = 0.03, d = −0.48) and six-month (z = −2.11, p = 0.03, d = −0.47) follow-ups. In the intention-to-treat (ITT) analysis, similar patterns were observed; however, the effect sizes were generally slightly smaller compared to those reported in the Completers Analysis (see Appendix 2).
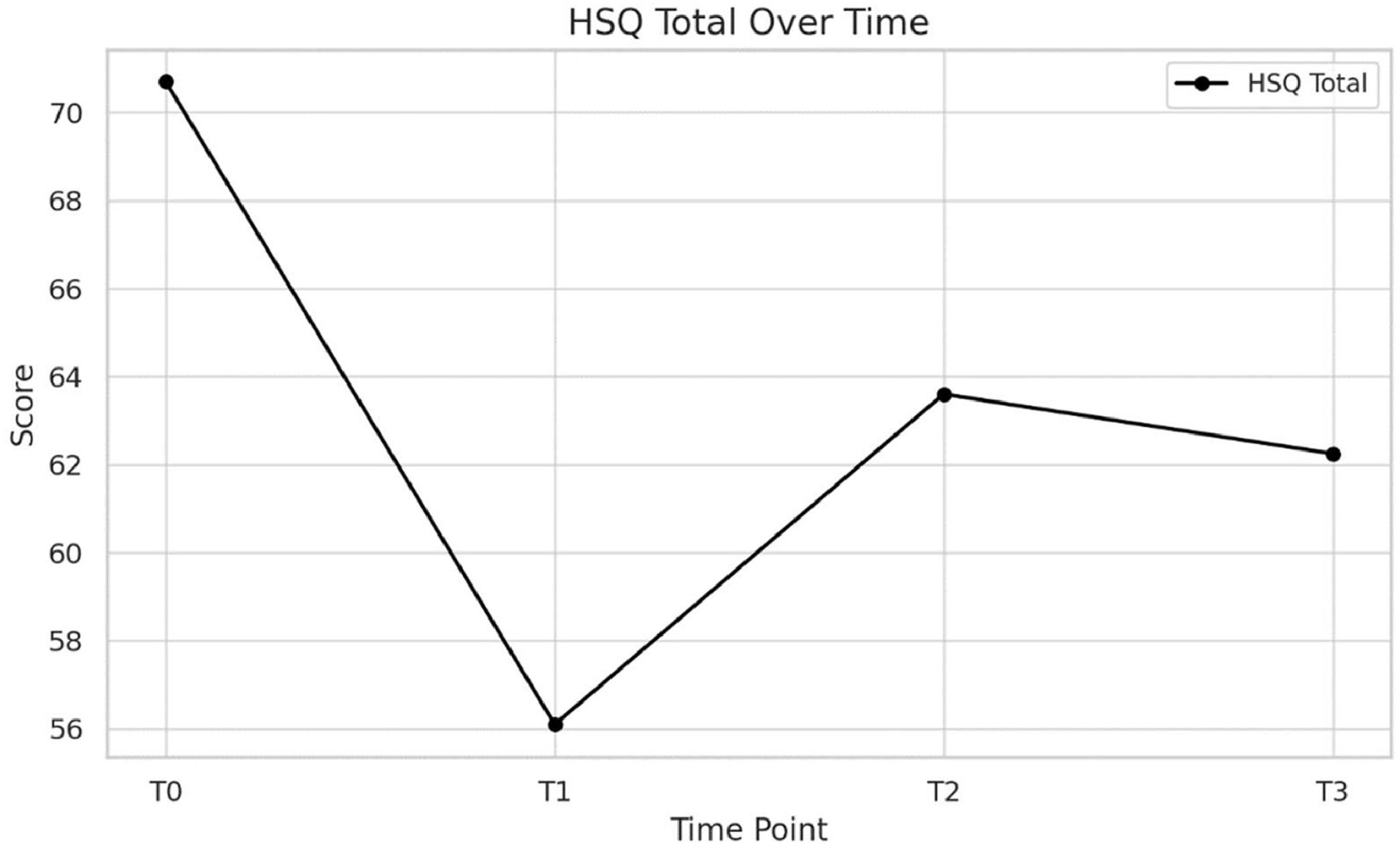
Home situations questionnaire (HSQ)The HSQ Total score showed a marginally significant decrease from baseline (M = 70.70, SD = 36.60) to post-treatment (M = 56.10, SD = 21.04) (z = −2.00, p = 0.05, d = −0.45). However, this improvement did not persist at the three-month (M = 63.60, SD = 38.46) or six-month follow-ups (M = 62.25, SD = 32.97) (see Fig. 3). In the intention-to-treat (ITT) analysis, a similar pattern was observed (see Appendix 2).
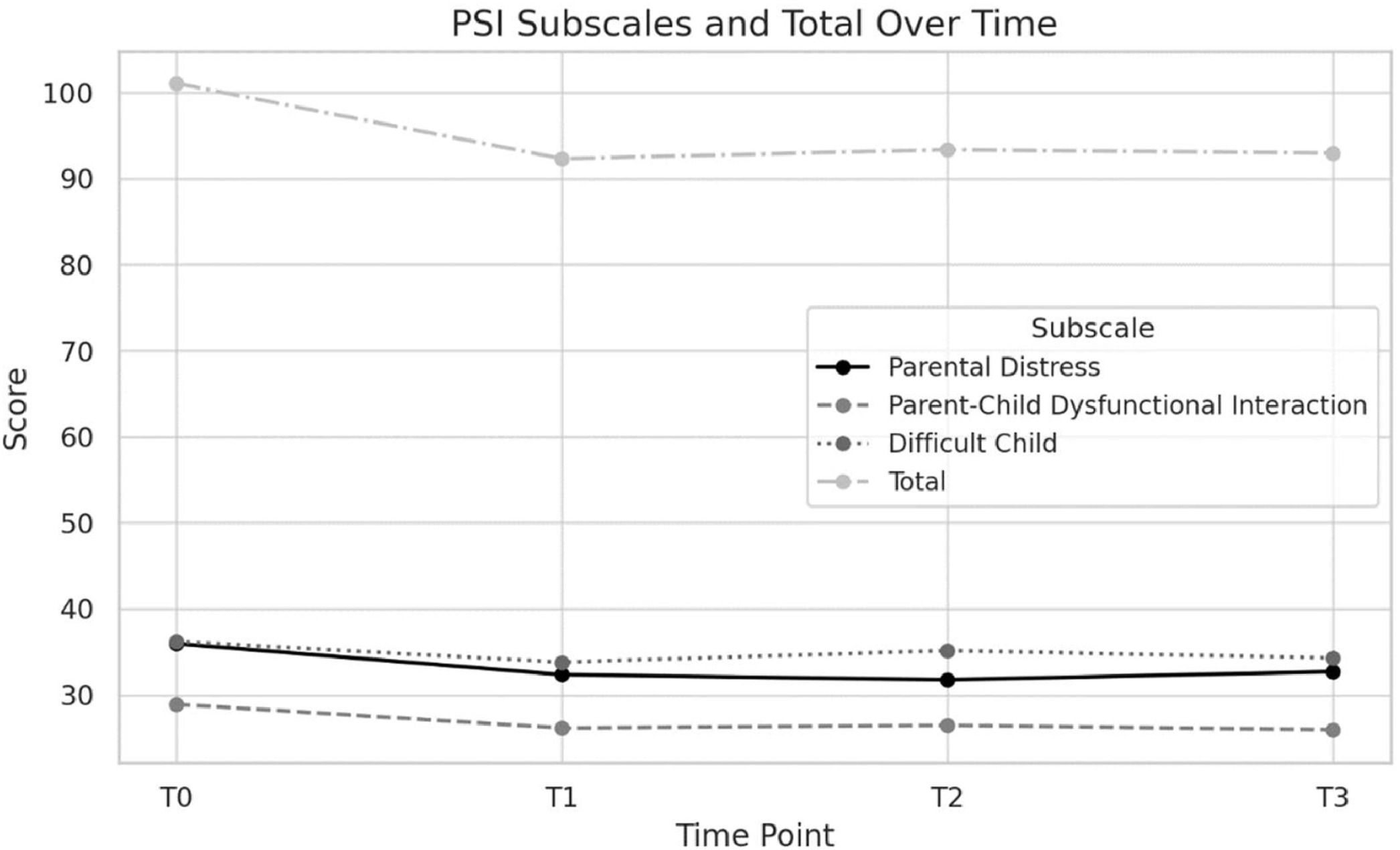
Parental stress index – short formA significant reduction was observed in the Parent-Child Dysfunctional Interaction subscale of the PSI-SF from baseline (M = 28.90, SD = 9.19) to post-treatment (M = 26.15, SD = 6.61) (z = −2.34, p = 0.02, d = −0.52). However, this effect did not persist at the three-month (M = 26.45, SD = 7.43) or six-month (M = 25.95, SD = 6.30) follow-ups. The Parent Distress subscale showed a marginally significant reduction from baseline (M = 35.95, SD = 12.64) to the three-month follow-up (M = 31.75, SD = 12.27) (z = −1.97, p = 0.05, d = −0.44), but this effect did not persist at the six-month follow-up (M = 32.70, SD = 11.54). The total PSI-SF score demonstrated a significant reduction from baseline (M = 101.05, SD = 29.90) to post-treatment (M = 92.30, SD = 21.81) (z = −2.31, p = 0.02, d = −0.52). However, this effect was not maintained at the three-month (M = 93.35, SD = 25.14) or six-month (M = 92.95, SD = 23.41) follow-ups (see Fig. 4). No significant differences were observed in the Difficult Child subscale at any evaluation timepoint. The intention-to-treat (ITT) analysis revealed a similar pattern (see Appendix 2).
Pediatric quality of life – family impact module (PedsQL-FIM)HRQoL scores showed a significant increase from baseline (M = 59.81, SD = 25.28) to post-treatment (M = 84.81, SD = 29.27) (z = −3.79, p < 0.01, d = −0.85). This improvement was maintained at both the three-month (M = 86.81, SD = 29.04) (z = −3.92, p < 0.01, d = −0.88) and six-month follow-ups (M = 86.19, SD = 30.29) (z = −3.88, p < 0.01, d = −0.87) (see Fig. 5). The intention-to-treat (ITT) analysis showed similar trends, although the effect sizes were generally smaller compared to the Completers Analysis (see Appendix 2).
An overview of all the results is provided in Table 3.
Results of the Wilcoxon signed-rank test for Completers (n = 20).
This study evaluated the feasibility, acceptability, and preliminary efficacy of a telehealth-delivered group PT program for families of children with ASD exhibiting behavioral difficulties. Our results indicate that this group-based telehealth intervention is a feasible and well-received approach, demonstrating potential to reduce disruptive behaviors in children and improve caregiver well-being, with some benefits sustained over time. These findings align with a growing body of literature supporting telehealth as an effective medium for behavioral interventions, particularly valuable in contexts with limited in-person services. While prior studies27,44 have highlighted the feasibility and satisfaction of individual telehealth PT programs, our study adds to the field by examining a group-based format. Group telehealth PT may combine the accessibility benefits of remote services with the social support inherent in group settings. This format is relatively underexplored but holds promise for enhancing family engagement and reducing caregiver isolation through shared community experiences. Parents in our study reported high satisfaction with the group format, noting that it fostered valuable peer support and encouraged shared learning—consistent with previous findings suggesting the benefits of group dynamics in PT settings.32,43
Feasibility and acceptabilityOur study’s high acceptability and feasibility ratings are consistent with findings from prior similar studies,27,39,40 which reported strong parent engagement and satisfaction with telehealth due to its convenience and accessibility. Like these studies, our results indicate that telehealth PT offers a viable alternative to in-person services, particularly for families limited by logistical challenges. Furthermore, our group-based approach extends findings by previous studies,40,45 which showed that group telehealth formats can uniquely benefit parents by reducing feelings of isolation and enhancing social support. Parents in our study echoed these findings, highlighting the value of connecting with others facing similar challenges—a benefit that individual telehealth programs may not fully capture. While the overall findings align with existing literature, discrepancies also emerged. For example, Bearss et al.27 observed that individual telehealth PT yielded higher adherence rates compared to some group formats, potentially due to individualized scheduling flexibility. Although our study demonstrated high attendance and engagement, some participants encountered scheduling conflicts, suggesting that group telehealth PT may benefit from additional scheduling accommodations or hybrid models to enhance accessibility further. Additionally, Kuravackel44 found that combining individual and group sessions within telehealth PT provided a more tailored experience, reducing stress and improving caregiver confidence. Future studies may explore mixed formats to optimize the benefits of group dynamics while maintaining the personalized support that individual sessions offer.
Preliminary efficacyThe telehealth-delivered PT program demonstrated significant reductions in child behavioral difficulties, with improvements measured by the Aberrant Behavior Checklist (ABC) across subscales such as irritability, lethargy, and hyperactivity. Reductions in irritability and lethargy were observed immediately post-treatment, and notably, hyperactivity improvements were sustained at three- and six-month follow-ups. These findings suggest that parents effectively applied behavioral strategies learned during the program to manage challenging behaviors, contributing to sustained improvements in some behavioral domains. However, the Home Situations Questionnaire (HSQ) scores indicated that not all gains persisted, highlighting the potential need for ongoing support to maintain improvements in daily contexts. The observed reductions in behavioral difficulties, especially in irritability and hyperactivity, are consistent with behavioral gains documented in prior studies.36,45 Over half of our study’s participants displayed reliable changes in behavior, aligning with Shanok et al. ,41 which also found that over 50 % of children showed significant behavioral improvements through telehealth PT. However, while our findings confirm post-intervention behavioral gains, the sustainability of these effects was mixed. For example, while reductions in irritability and hyperactivity persisted, other improvements diminished over time. This partial contrast with Martin et al. ,39 where sustained effects on child behavior and parental stress were more consistent, suggests that the addition of booster sessions could reinforce training and promote lasting improvements.
Caregivers in this study experienced significant reductions in stress, particularly in the Parent-Child Dysfunctional Interaction and Parent Distress subscales of the Parental Stress Index-Short Form (PSI-SF). These results align with prior research suggesting that PT can alleviate caregiver stress by enhancing parental competence and reducing challenging child behaviors.17,20 However, as observed in the current study, some improvements in parental stress diminished over time. This decline aligns with Martin et al. ,39 who also identified a need for booster sessions to sustain caregiver gains, suggesting that ongoing structured support could reinforce initial PT outcomes. The intervention also produced significant improvements in family quality of life, measured by the Pediatric Quality of Life Inventory – Family Impact Module (PedsQL-FIM). Unlike some parental stress reductions, these improvements in family quality of life were sustained over time, suggesting a lasting positive impact on family dynamics and overall well-being. This sustained improvement may reflect the broader influence of PT, not only in mitigating child behavioral symptoms but also in enhancing family functioning as a whole. The alleviation of caregiver stress and reduction in challenging child behaviors likely contributed to an improved family environment, supporting the notion that telehealth PT can extend benefits to multiple facets of family life.
LimitationsThis study has several limitations that should be noted when interpreting the findings. First, the single-arm, pretest-posttest design without a control group limits our ability to draw causal inferences about the efficacy of the telehealth PT intervention. The absence of randomization and a control condition, in contrast to prior studies,27,39 restricts our capacity to differentiate the intervention's effects from other external influences, such as changes in home dynamics or external support services. Future research should incorporate randomized controlled trials to strengthen the evidence base for telehealth-delivered PT for children with ASD, offering more robust causal insights into its effectiveness. The sample was not representative of the broader ASD population, as it included only families with stable medication regimens and sufficient internet access. Moreover, the high attrition rate (36 %) and low proportion of final completers relative to initial invitations (18 %) raise questions about the real-world feasibility of this model. Feedback from participants indicated that technical difficulties and conflicting schedules were common barriers to engagement, echoing findings from Shanok et al. ,41 where similar challenges in telehealth programs affected retention rates. Future studies might consider implementing strategies to improve retention, such as flexible scheduling, technical support, or alternative formats that better accommodate families' unique needs and constraints. The relatively small sample size further limits the study’s power to detect smaller effect sizes and may not fully represent the broader population of families of children with ASD. This constraint limits the generalizability of the findings and suggests that larger-scale studies are necessary to confirm these results. Additionally, excluding participants who changed psychotropic medication may limit the generalizability of our findings. Future studies should consider analyzing data up to the point of medication change. Regarding data analysis, the use of LOCF to handle missing data has known limitations, including potential bias and underestimation of variability.59 Alternative imputation methods should be considered in future research. Future research could benefit from examining potential variations in efficacy based on demographic factors, socioeconomic status, and children’s behavioral profiles to understand which subgroups might benefit most from telehealth-delivered PT. Finally, some participants reported difficulty completing inter-session tasks, which may have impacted their adherence to the program. This feedback suggests that certain program components might benefit from simplification or adjustments to better meet families’ needs. Future studies could explore ways to optimize task complexity and provide additional support to enhance adherence and engagement.
Clinical implicationsThese findings suggest that the intervention may be particularly beneficial for a subset of motivated families with stable routines and adequate resources. Future adaptations should consider stratifying interventions based on family needs, resources, and behavioral profiles of the children. The group-based telehealth format uniquely fosters a sense of community and shared experience among participants, a dynamic shown to benefit caregiver mental health and confidence, potentially reducing feelings of isolation. By providing a communal space for caregivers to connect, telehealth group PT supports mental well-being and enhances parental competence, reinforcing its value beyond individual outcomes.
ConclusionsThis study provides promising evidence for the feasibility, acceptability, and preliminary efficacy of a telehealth-delivered group PT program for managing challenging behaviors in children with ASD. The findings align with prior research, reinforcing telehealth as a viable, practical modality for delivering PT, especially in settings where in-person access is limited. By offering significant reductions in maladaptive child behaviors and improvements in caregiver stress and quality of life, this telehealth group PT intervention addresses a critical gap in ASD care, particularly for underserved families facing logistical barriers to traditional services. The group-based telehealth format offers distinct advantages, not only by expanding access to effective behavioral interventions but also by fostering a sense of community and shared experience among caregivers. This communal element helps alleviate caregiver isolation, enhancing parental competence and engagement, which are essential for sustained intervention success. These results build on previous studies underscoring the added value of group settings in telehealth PT by facilitating peer support and mutual learning. Future research should focus on refining telehealth PT by exploring different program structures, including the comparison of group and individual formats within telehealth, and assessing the effectiveness of booster sessions. Furthermore, larger and more diverse sample sizes are necessary to confirm these findings and to explore how telehealth interventions can best meet the needs of varied family demographics, socioeconomic backgrounds, and behavioral profiles.
Ethical considerationsThe study ensured the confidentiality of personal data in accordance with national and European data protection regulations. Ethical approval was secured from the center’s clinical research ethics committee prior to the study, and all participants provided signed informed consent after being duly informed.
FundingThis research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Declaration of generative AI and AI-assisted technologies in the writing processDuring the preparation of this work the author(s) used ChatGPT in order to check grammar and language. After using this tool/service, the author(s) reviewed and edited the content as needed and take(s) full responsibility for the content of the publication.
The Authors declare that there is no conflict of interest.
The authors thank all the children and families who have participated in the study. The authors also acknowledge the community stakeholders who have contributed to this study.
ABC: Aberrant Behavior Checklist; APSI: Autism Parenting Stress Index; BPS: Being a Parent Scale; BPT: Behavioral Parent Training; CHOPE: COMPASS for Hope; CGI-I: Clinical Global Impression – Improvement Scale; ECBI: Eyberg Child Behavior Inventory; HSQ-ASD: Home Situation Questionnaire – Autism Spectrum Disorder; NR: Non-reported; PAM-DD: Parent Activation Measure for Developmental Disabilities; PedsQL-FIM: Pediatric Quality of Life Questionnaire – Family Impact Module; PKQ: Parent Knowledge Questionnaire; PSI: Parental Stress Index – Short Form; PTKA: Parent Training Knowledge Assessment; RUBI-PT: Research Units in Behavioral Intervention - Parent Training; RUBI-T: Research Units in Behavioral Intervention - Telehealth; VABS-II: Vineland Adaptive Behavior Scales.