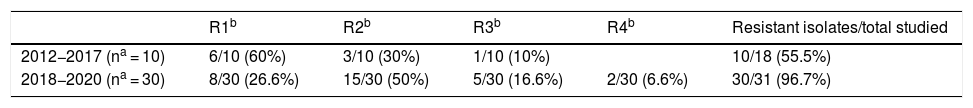
The antimicrobial resistance of Helicobacter pylori Helicobacter pylori (H. pylori) seriously restricts treatment options1. H. pylori resistance in Spain to one or more active antimicrobials ranges from 17.9% to 51.2% for clarithromycin (CLH), 32% to 33.3% for rifampicin (RD), 17.8% to 38.7% for levofloxacin (LE) and 27% to 39.2% for metronidazole (MZ), while 27.2%–66.6%; 12.4%–20%; 2.4%–12.8% and 1.4% are resistant to one, two, three and four antibiotics, respectively2–5. This study analysed antimicrobial resistance from 2012 to June 2020. Gastric biopsies were cultured in Columbia agar, Chocolate agar and Thayer-Martin agar (bioMérieux and BBL) in microaerophilic conditions for 10 days. The susceptibility study was performed in Mueller Hinton Fastidious Agar (bioMérieux) using the ETEST (bioMérieux). The antimicrobials studied and the breakpoints used were those recommended by the European Committee on Antimicrobial Susceptibility Testing (EUCAST)6. In total, 49 H. pylori isolates were studied, 40 (81.6%) of which were resistant to one or more antimicrobials. Overall, 35% (14/40) of the isolates were resistant to one antimicrobial: 50% (7/14) were resistant to CLH, 35.7% (5/14) to MZ and 14.3% (2/14) to amoxicillin (AMX). No other monoresistances were identified. In total, 65% (26/40) were resistant to more than one antimicrobial. Overall, 69.2% (18/26) were resistant to two antimicrobials. The most common combination was CLH-MZ at 72.2% (13/18), followed by CLH-RD at 11.1% (2/18), CLH-LE at 11.1% (2/18) and LE-MZ at 5.5% (1/18). In total, 23% (6/26) were resistant to three antimicrobials, all of which to the combination CLH-MZ-LE. Overall, 7.6% (2/26) were resistant to four antimicrobials, all of which to the combination CLH-MZ-LE-RD. The evolution of resistance over time shows a spike in the last three years. From 2012 to 2017, out of a total of 18 isolates, 55.5% (10/18) were resistant to at least one antimicrobial. From 2018 to 2020, out of a total of 31 isolates, 96.7% (30/31) were resistant to at least one antimicrobial. This represents an increase of 41.2% (P = .0003; χ2). Table 1 shows the evolution of resistance over time. In terms of combinations of antimicrobial resistance from 2012 to 2017, CLH-MZ accounted for 20% (2/10) and CLH-MZ-LE for 10% (1/10). From 2018 to 2020, the combination CLH-MZ accounted for 36.6% (11/30) and CLH-MZ-LE for 16.6% (5/30), while resistance to CLH-MZ-LE-RD was detected for the first time in 2020 in 6.6% (2/30) of the isolates. In short, the treatment alternatives whose susceptibility data make them the most active against H. pylori in this health area are tetracycline (100%), AMX (95.9%) and RD (91.8%). For this research, it was not possible to ascertain whether patients in whom H. pylori was isolated had been previously treated, which is a limitation of the study. Despite this, given the high rates of H. pylori antimicrobial resistance, we consider it vital to determine antimicrobial susceptibility by gastric biopsy and H. pylori culture prior to starting treatment7.
Increased H. pylori antimicrobial resistance could be associated with the use of non-invasive diagnostic techniques such as the breath test and stool antigen tests. The microorganism is not isolated in either case, making it impossible to perform an antimicrobial susceptibility test. As a result, the use of untargeted antimicrobial therapy not determined by an antimicrobial susceptibility test could select resistant strains. To support this theory, variability of antimicrobial resistance has been observed in a single strain of H. pylori obtained after culturing gastric biopsies from the gastric antrum and body of a single patient and collected in a single procedure. According to Selgrad et al., this variability in resistance has been identified in 15.2% of patients8. All these factors could help to explain the rise in H. pylori antimicrobial resistance.
FundingNo funding was received for this study.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Moreno-Flores A, Potel-Alvarellos C, Álvarez-Fernández M. Helicobacter pylori, evolución de la resistencia a antimicrobianos 2012–2020 en el área sanitaria de Vigo, Pontevedra, España. Enferm Infecc Microbiol Clin. 2021;39:523–524.