Pheochromocytoma is a catecholamine-producing neuroendocrine tumor derived from the chromaffin cells of the adrenal gland. The annual incidence is between 0.005 and 0.1%,1 though diagnostic difficulties result in an underestimation of the true incidence.2 Infrequently, pheochromocytoma manifests as Takotsubo-like cardiomyopathy,3 which is characterized by transient apical myocardial dysfunction simulating acute coronary syndrome, but with healthy coronary arteries. To date, a total of 84 cases of Takotsubo cardiomyopathy associated with pheochromocytoma have been reported.1,4,5 We report the case of a patient requiring multiple admissions due to a myocardial dysfunction classified as recurrent Takotsubo cardiomyopathy secondary to pheochromocytoma.
A 70-year-old woman with no known family or personal history of disease presented with self-limiting symptoms of chest pain, palpitations and perspiration. She reported to the emergency room with the aforementioned symptoms, associated with dyspnea, normal blood pressure, and SatO2 84%. The ECG tracing showed ST depression on the lateral surface, and the laboratory tests revealed troponin elevation to 1200ng/l (normal range: 0–13). The patient presented acute lung edema (ALE) requiring invasive mechanical ventilation (IMV) and diuretic and vasodilator medication. Echocardiography revealed severe contractile dysfunction with a left ventricular ejection fraction (LVEF) of 36% and posterolateral akinesis. With the suspicion of acute myocardial infarction (AMI), coronary artery catheterization was performed, but yielded no evidence of significant lesions. The condition was postulated to correspond to posterolateral AMI secondary to embolism. Control echocardiography 10 days after the acute event showed recovery of the LVEF (65%).
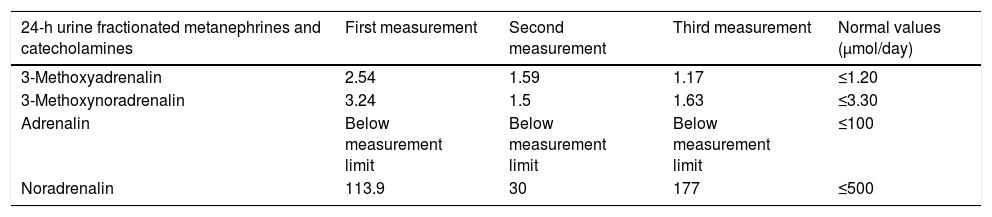
Two years later, under follow-up by her family physician, with good blood pressure control and no hyperadrenergic episodes, the patient returned to the emergency room in cardiogenic shock requiring noradrenalin, dobutamine, and IMV. The ECG tracing revealed marked negative T-waves on the anterolateral surface, with a positive troponin curve. Initial echocardiography showed a LVEF of 30–35%. The coronary catheterization findings were normal, and LVEF recovered two weeks later. A tentative diagnosis of Takotsubo cardiomyopathy was established. The patient reported again to the emergency room four months later due to ALE in the context of rapid atrial fibrillation, with a tendency toward hypotension. Vasoactive drugs were required. The acute phase echocardiographic study showed severe ventricular dysfunction. The Endocrinology department was consulted to rule out pheochromocytoma as the underlying cause. Twenty-four hour urine catecholamine measurements revealed no significant elevation (Table 1). The patient was under treatment with propranolol. Abdominal computed tomography (CT) with contrast injection identified an ovoid right adrenal mass measuring 30×20mm in size. The lesion was hypodense, with fine capsular enhancement in the arterial and portal phases, with no features typical of pheochromocytoma. By contrast, scintigraphy with metaiodobenzylguanidine showed radioiodine uptake consistent with pheochromocytoma in the right adrenal gland. A second urine catecholamine test performed three weeks after the first continued to yield negative results (Table 1). The patient was readmitted a few days later due to hypertensive ALE, and repeat catecholamine testing in urine, this time in the absence of drug treatment, again proved normal (Table 1). Magnetic resonance imaging (MRI) of the adrenal glands revealed a well-defined right adrenal nodule measuring 27×20mm in size, with no features typical of adenoma or pheochromocytoma. Despite the conflicting complementary test results, pheochromocytoma was suspected, and a right adrenalectomy was indicated following alpha block with doxazosin 4mg/day. The administration of nitroprusside was required during surgery. The pathology report indicated pheochromocytoma. The patient subsequently remained asymptomatic, with normal control blood pressure values, and doxazosin was discontinued. In accordance with the recommendations of the Clinical Practice Guidelines, a genetic study was requested, with pending results.6
Twenty-four hour catecholamine values.
| 24-h urine fractionated metanephrines and catecholamines | First measurement | Second measurement | Third measurement | Normal values (μmol/day) |
|---|---|---|---|---|
| 3-Methoxyadrenalin | 2.54 | 1.59 | 1.17 | ≤1.20 |
| 3-Methoxynoradrenalin | 3.24 | 1.5 | 1.63 | ≤3.30 |
| Adrenalin | Below measurement limit | Below measurement limit | Below measurement limit | ≤100 |
| Noradrenalin | 113.9 | 30 | 177 | ≤500 |
Pheochromocytoma has been described as “the great simulator”, because it can have multiple presentations from the clinical and imaging perspective, making diagnosis difficult. Occasionally, the first manifestation is a consequence of myocardial involvement, which may require heart transplantation or even prove fatal.3 Such myocardial manifestations may be due to multiple causes. Screening for pheochromocytoma therefore usually starts months after the first event has occurred. In cases of pheochromocytoma-induced Takotsubo cardiomyopathy, the complication rate is reportedly higher than in Takotsubo due to other causes: heart failure, ALE, cardiogenic shock and electromechanical dissociation.7 The association between pheochromocytoma and Takotsubo cardiomyopathy is uncommon, and the present case is the only one of its kind in our series of 76 pheochromocytomas and paragangliomas documented since 1981.8
The name Takotsubo (Tako-Tsubo) comes from the Japanese term for octopus trap, the shape of which resembles the myocardium affected by the disorder: the middle and apical left ventricular segments are hypokinetic, with basal hyperkinesia. This pattern could be explained by increased catecholamine susceptibility in the ventricular apical and middle segments, as a result of differences in beta-adrenergic receptor distribution.5 It was reported that 74.6% of all patients with this type of cardiomyopathy had elevated plasma catecholamine levels.9 In fact, according to the criteria of the Mayo Clinic, screening for pheochromocytoma should be performed if Takotsubo cardiomyopathy is suspected.
The initial screening test for pheochromocytoma involves the measurement of plasma or urine metanephrine levels. There is no agreement as to which is the sample of choice, since no direct comparative studies have been made. Some authors advocate the initial measurement of fractionated catecholamines and metanephrines in urine, due to its high sensitivity and specificity. False negative results may be seen due to incomplete sample collection, the presence of small tumors, or dopamine producing lesions.6 On the other hand, some studies suggest that the measurement of plasma metanephrines has a greater negative predictive value (96–100%).10 Such a measurement is the option of choice in cases in which the diagnosis is strongly suspected, and where a normal value would allow for ruling out the diagnosis, except in concrete cases such as strict dopamine secreting tumors. In these latter tumors, plasma 3-methoxytyramine determination is helpful. Given the greater specificity of plasma measurement, its quantification might have been useful for the diagnosis of our patient.
In our case, clinical stability and cure were achieved after tumor surgery. The exceptionality of the present case lies in the atypical presentation of the tumor and the discordant diagnostic test results, with normal urinary catecholamine levels, and the scantly suggestive CT and MRI findings. In conclusion, it is essential to suspect pheochromocytoma in Takotsubo cardiomyopathy, despite its low incidence and even with negative urine catecholamine findings.
Please cite this article as: Hernández-Montoliu L, Simó-Servat A, Villabona C. Cardiomiopatía de Tako-Tsubo inducida por feocromocitoma. Endocrinol Diabetes Nutr. 2018;65:549–551.