Central diabetes insipidus (DI) results from complete or partial dysfunction of the neurons of the hypothalamus or the posterior pituitary gland.1 DI carries a risk of hypernatraemic dehydration if untreated1 and of iatrogenic hyponatraemia when treated with desmopressin (DDAVP).2
Adipsic diabetes insipidus (ADI) is a rare disease associated with morbidity and mortality whose management represents a therapeutic challenge,1,3 with rates of hypernatraemia as high as 50% and rates of hyponatraemia of 25% observed during its treatment.2 We report the inpatient management protocol for ADI of the Endocrinology Department of Hospital Universitario La Paz [La Paz University Hospital] (Madrid), as well as its scientific basis and its outcome in a patient managed from November 2018 to April 2019.
The patient was a previously healthy 33-year-old woman who developed complete ADI after a surgical procedure for a neurocytoma of the third ventricle, along with central hypogonadism and hypocortisolism, cognitive impairment and urinary incontinence. She needed to be hospitalised for 244 days owing to her need for complex management of plasma sodium levels as well as acute complications of her surgical procedure. From day three to day 193 of hospitalisation, the patient had 11 episodes of a lowered level of consciousness associated with major changes in plasma sodium levels (ΔNaS) of up to 42 mmol/l/48 h. Four of those 11 episodes required critical care unit admission and 10 of the episodes occurred without the use of the protocol.
The patient’s ADI was initially managed according to current clinical consensus recommendations; it was managed without the protocol (s¯P) for 110 of the 244 days (45%) of her admission. The protocol was initially implemented for 30 days (12.4%) and subsequently used for 104 days (42.6%) of the patient’s stay. In the s¯P management period, mean plasma sodium levels were 141.3 ± 9.2 mmol/l (p5-p95: 126−153 mmol/l), and in the c¯P management period, they were 140.2 ± 5.8 mmol/l (p5-p95: 134–148); the difference was statistically significant (p = 0.004). Higher rates of normal plasma sodium levels (135−145 mmol/l) were seen during c¯P management compared to s¯P management (79% versus 49.7%, p < 0.001). Similarly, rates of hyponatraemia (<135 mmol/l) and hypernatraemia (>145 mmol/l) during c¯P management were lower than those observed during s¯P management (8.3% versus 21%, p = 0.001, and 12.7% versus 29.3%, p < 0.001, respectively). As a result of improved management of the patient’s plasma sodium levels, the range of ΔNaS decreased and she was discharged.
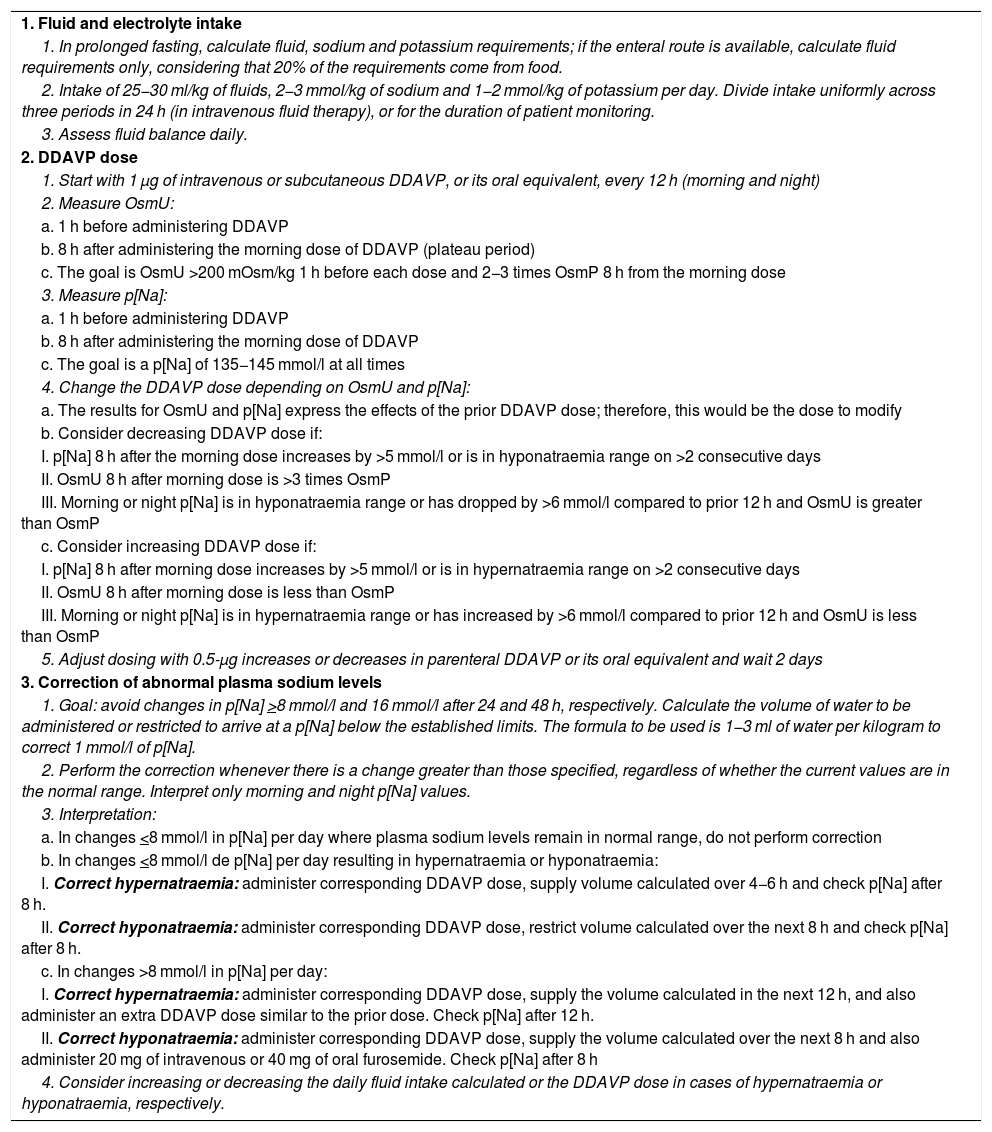
The protocol was based on publications of physiology studies and clinical studies aimed at controlling water/sodium homoeostasis, which guided three essential aspects of ADI management: (1) fluid and electrolyte intake, (2) DDAVP dose and (3) correction of abnormal plasma sodium levels (Table 1).
Inpatient management protocol for diabetes insipidus associated with adipsia.
| 1. Fluid and electrolyte intake |
| 1. In prolonged fasting, calculate fluid, sodium and potassium requirements; if the enteral route is available, calculate fluid requirements only, considering that 20% of the requirements come from food. |
| 2. Intake of 25−30 ml/kg of fluids, 2−3 mmol/kg of sodium and 1−2 mmol/kg of potassium per day. Divide intake uniformly across three periods in 24 h (in intravenous fluid therapy), or for the duration of patient monitoring. |
| 3. Assess fluid balance daily. |
| 2. DDAVP dose |
| 1. Start with 1 μg of intravenous or subcutaneous DDAVP, or its oral equivalent, every 12 h (morning and night) |
| 2. Measure OsmU: |
| a. 1 h before administering DDAVP |
| b. 8 h after administering the morning dose of DDAVP (plateau period) |
| c. The goal is OsmU >200 mOsm/kg 1 h before each dose and 2−3 times OsmP 8 h from the morning dose |
| 3. Measure p[Na]: |
| a. 1 h before administering DDAVP |
| b. 8 h after administering the morning dose of DDAVP |
| c. The goal is a p[Na] of 135−145 mmol/l at all times |
| 4. Change the DDAVP dose depending on OsmU and p[Na]: |
| a. The results for OsmU and p[Na] express the effects of the prior DDAVP dose; therefore, this would be the dose to modify |
| b. Consider decreasing DDAVP dose if: |
| I. p[Na] 8 h after the morning dose increases by >5 mmol/l or is in hyponatraemia range on >2 consecutive days |
| II. OsmU 8 h after morning dose is >3 times OsmP |
| III. Morning or night p[Na] is in hyponatraemia range or has dropped by >6 mmol/l compared to prior 12 h and OsmU is greater than OsmP |
| c. Consider increasing DDAVP dose if: |
| I. p[Na] 8 h after morning dose increases by >5 mmol/l or is in hypernatraemia range on >2 consecutive days |
| II. OsmU 8 h after morning dose is less than OsmP |
| III. Morning or night p[Na] is in hypernatraemia range or has increased by >6 mmol/l compared to prior 12 h and OsmU is less than OsmP |
| 5. Adjust dosing with 0.5-μg increases or decreases in parenteral DDAVP or its oral equivalent and wait 2 days |
| 3. Correction of abnormal plasma sodium levels |
| 1. Goal: avoid changes in p[Na] >8 mmol/l and 16 mmol/l after 24 and 48 h, respectively. Calculate the volume of water to be administered or restricted to arrive at a p[Na] below the established limits. The formula to be used is 1−3 ml of water per kilogram to correct 1 mmol/l of p[Na]. |
| 2. Perform the correction whenever there is a change greater than those specified, regardless of whether the current values are in the normal range. Interpret only morning and night p[Na] values. |
| 3. Interpretation: |
| a. In changes <8 mmol/l in p[Na] per day where plasma sodium levels remain in normal range, do not perform correction |
| b. In changes <8 mmol/l de p[Na] per day resulting in hypernatraemia or hyponatraemia: |
| I. Correct hypernatraemia: administer corresponding DDAVP dose, supply volume calculated over 4−6 h and check p[Na] after 8 h. |
| II. Correct hyponatraemia: administer corresponding DDAVP dose, restrict volume calculated over the next 8 h and check p[Na] after 8 h. |
| c. In changes >8 mmol/l in p[Na] per day: |
| I. Correct hypernatraemia: administer corresponding DDAVP dose, supply the volume calculated in the next 12 h, and also administer an extra DDAVP dose similar to the prior dose. Check p[Na] after 12 h. |
| II. Correct hyponatraemia: administer corresponding DDAVP dose, supply the volume calculated over the next 8 h and also administer 20 mg of intravenous or 40 mg of oral furosemide. Check p[Na] after 8 h |
| 4. Consider increasing or decreasing the daily fluid intake calculated or the DDAVP dose in cases of hypernatraemia or hyponatraemia, respectively. |
Note: Once stable plasma sodium levels are achieved, it is recommended that p[Na] checks be performed at least once every 24 h, at the same time each day, in order to prevent ΔNaS associated with neurological damage.
DDAVP: desmopressin; p[Na]: plasma sodium levels; OsmU: urine osmolality; OsmP: plasma osmolality; ΔNaS: changes in plasma sodium levels.
Daily water requirements are lower in women and higher in environments with a temperatures ≥30 °C,4 and depend on metabolic expenditure (∼1 ml/kcal/kg4) and solute load.5 To achieve normal hydration, defined as plasma sodium levels of 135−144 mmol/l with urine osmolality (OsmU) <500 mOsm/l, 40−45 ml/kg/day of fluids are needed.6 However, the usual fluid intake, extrapolated to a healthy person weighing 70 kg, is ∼28−35 ml/kg/day.5 We use a maintenance fluid intake of 25−30 ml/kg/day, since temperatures in hospital settings are usually <30 °C and metabolic expenditure in hospitalised patients is typically minimal, except in inflammatory conditions. We also use a potassium intake of 1−2 mmol/kg and a sodium intake of 2−3 mmol/kg per day, as several studies have found intake of 1.3–1.7 mmol/kg/day of potassium and 0.9−3 mmol/kg/day of sodium to yield maximum benefits in healthy people.7
2DDAVP doseThe effects of DDAVP peak two to four hours after administration, then plateau over the next four to eight hours, gradually decreasing in the last hour and then disappearing.8 Given its half-life of six to eight hours, it should be administered every eight to 12 h in complete DI.3
The DDAVP regimen should imitate the normal dynamics of arginine vasopressin in the hypothalamus. In dehydration, release of arginine vasopressin from the hypothalamus is seen to peak when plasma osmolality (OsmP) is >290 mOsm/kg,8 translating to an OsmU of >900 mOsm/kg. In overhydration, with an OsmP <280 mOsm/kg, plasma arginine vasopressin is nearly undetectable and OsmU is seen to be lower than OsmP.8 In complete ADI treated with DDAVP, the relationship between OsmU and OsmP will enable interpretation of dose suitability.
We titre the DDAVP dose based on measurements of OsmU, OsmP and plasma sodium levels in the plateau period for the dose administered and one hour before the next dose. We consider the dose suitable when we observe OsmU values two to three times greater than OsmP values during the plateau period and >200 mOsm/kg in the hour prior to the next dose, in the presence of normal plasma sodium levels. In our case, we found that OsmU >200 mOsm/kg before the morning dose was associated with ΔNaS <6 mmol/l in 12 h (p = 0.013), which we believe to be ideal.
3Correction of abnormal plasma sodium levelsIn hypernatraemia, we use DDAVP or supply fluids, and in hyponatraemia, we administer furosemide to counteract the action of active DDAVP or we reduce fluid intake.
The quantity of fluids that result in ΔNaS of 1 mmol/l is unknown. According to the Adrogué-Madias formula,9 intake of ∼3.5−4 ml of water per kilogram of weight would reduce plasma sodium levels by 1 mmol/l. Calculations from dehydration studies10 indicate that a loss of ∼2.5−4 ml of water per kilogram would increase plasma sodium levels by 1 mmol/l. In our case, we found that a decrease in fluid intake by 0.5−1 ml/kg increased plasma sodium levels by 1 mmol/l. Therefore, we used 1−3 ml of water per kilogram to correct plasma sodium levels by 1 mmol/l.
Ultimately, in the absence of more clinically rigorous studies, we hope that our experience aids in the management of other patients with ADI, with due attention paid to the importance of personalised treatment.
Confidentiality and ethicsThe authors declare that this study was conducted in accordance with accepted good clinical practice standards, the Declaration of Helsinki and Spanish regulations, following the current recommendations of the local independent ethics committee. Informed consent was not required for this study, given its retrospective design and data anonymisation.
FundingJGRS has a contract as a researcher with the Fundación para la Investigación Biomédica [Foundation for Biomedical Research] at Hospital Clínico San Carlos [San Carlos Clinical Hospital] (Reference: INV-15-2019). However, no funds were received to help with the preparation of this manuscript.
Conflicts of interestThe authors declare that they have no conflicts of interest for the conduct of this study.
Please cite this article as: Ruiz-Sánchez JG, Parra Ramírez P, Martín Rojas-Marcos P, Lecumberri Santamaría B, Álvarez Escolá C. Protocolo de manejo hospitalario de la diabetes insípida asociada a adipsia. Desarrollado a partir de un caso clínico. Endocrinol Diabetes Nutr. 2021;68:668–670.