In October 2020, the Spanish Society of Endocrinology and Nutrition (SEEN),1 in collaboration with the Spanish Diabetes Federation (FEDE),2 produced a consensus document establishing 15 keys to improve clinical care for diabetes in Spain.3
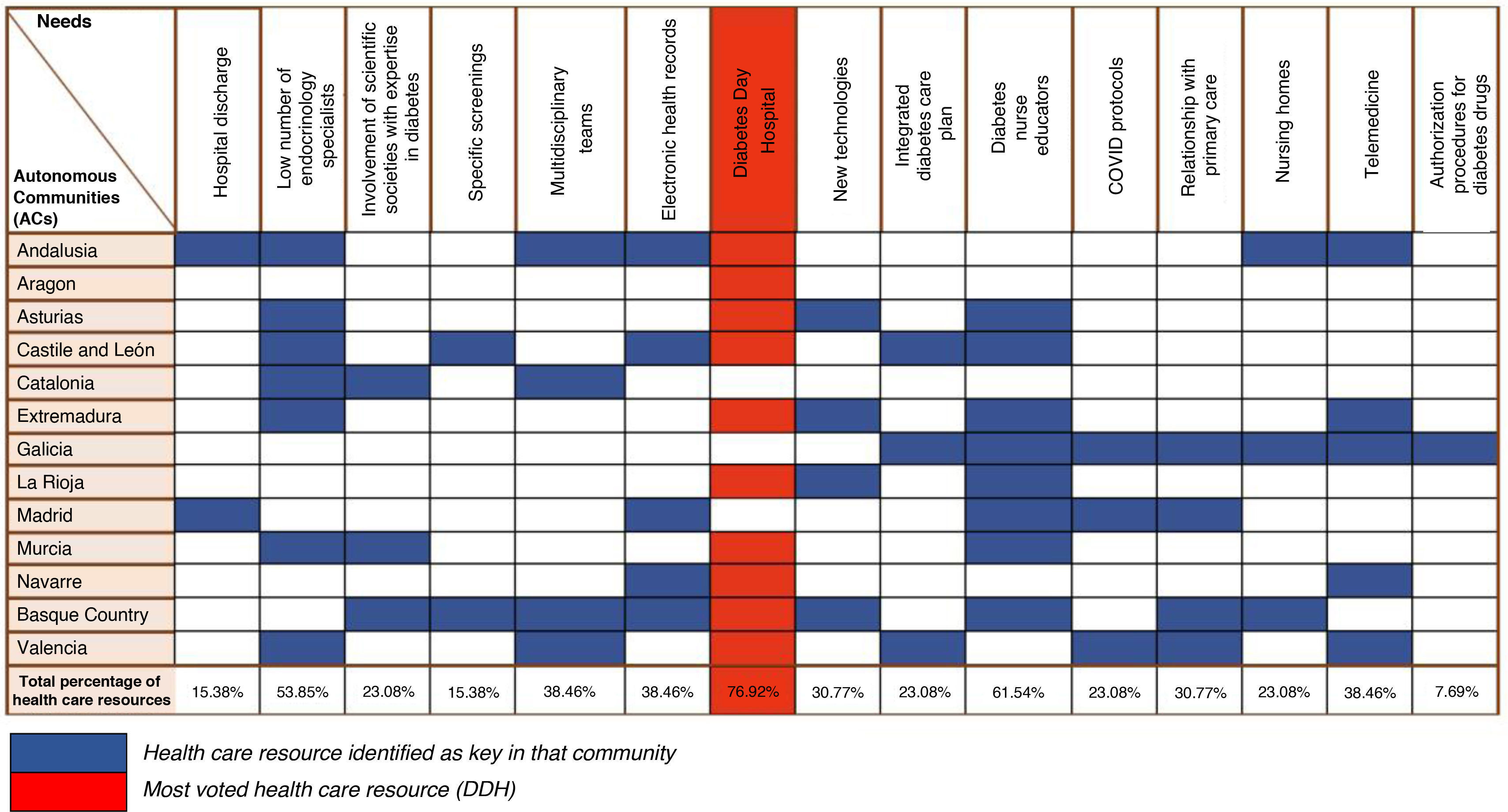
After presenting the project in 15 of Spain’s 17 autonomous communities, 76.9% identified the Diabetes Day Hospital (DDH) as a key resource in their region (Fig. 1).
The DDH arises as an alternative to inpatient admission for situations requiring a rapid response. Its primary objective is to offer patient-centered, high-quality care that is efficient, safe, and timely. Implementing DDHs is necessary and beneficial for the following reasons:
- •
Improve quality of life for people with diabetes. The DDH provides a rapid, highly specialized response to glycemic decompensations that are often referred to emergency departments and not infrequently result in prolonged hospitalization.
- •
Promote bidirectional communication with both users and other professional teams and specialties.
- •
Foster digital health innovation for diabetes care.
- •
Reduce costs associated with emergency care and hospitalization. DDHs save costs in the short, medium, and long term. The structured implementation of DDH units within a public health system is associated with a significant and sustained reduction in hospital admission rates for acute diabetes decompensations (Fig. 2).
Figure 2.Trend in admission rates for diabetic ketoacidosis in Andalusia (a health system equipped with DDHs) vs the rest of Spain.
Crude rates per 10,000 population of hospital discharges with a principal diagnosis (reason for admission) of DKA in hospitals of the National Health System of Andalusia and the rest of Spain, 1997–2022. DDH models were launched in Andalusia in 2006 (arrow).
Source: Statistical Portal – Ministry of Health (https://www.sanidad.gob.es/estadEstudios/estadisticas/sisInfSanSNS/aplicacionesConsulta/home.htm).
With this document, the scientific societies and FEDE present a coordinated value proposal among specialists in endocrinology and nutrition, family and community medicine, nursing, health management, and people with diabetes. Its mission is to serve as a useful tool to guide implementation of the DDH care model—considered key for an appropriate care response for people living with diabetes—and to support progressive integration of diabetes technology and digital health into diabetes care.
MethodologyA group of experts from scientific societies most directly involved in diabetes care (SEEN, SED, SEMERGEN, SEMG, CGE), together with SEDISA and FEDE, participated with technical support from the Omnicom group.4
SEEN and SED proposed an initial draft that was subsequently agreed upon and endorsed by the other signatory scientific societies (SEMERGEN, SEMG, CGE, and SEDISA) and by FEDE. The authors declared no conflicts of interest regarding this document, and no external funding was received.
This is an executive summary of a more complete document available on the signatory societies’ websites (https://www.seen.es/documentos/informe-hospital-de-dia-de-diabetes).
Mission and vision of the diabetes day hospitalThe definition of “Day Hospitalization” is hospital care for a maximum of 12 hours for diagnostics, clinical investigations and/or multiple assessments, and treatments that cannot be delivered in outpatient clinics but do not justify an inpatient stay (defined by the need to spend the night) in a hospital unit.
Experts agree on developing the DDH in the hospital setting as an intermediate device between inpatient care and scheduled ambulatory care, intended for non-deferrable care for people with diabetes, with specific mission and vision statements.
Mission: To provide comprehensive, accessible ambulatory care tailored to the needs of people with diabetes in situations of particular complexity across the lifespan.
Vision: To have an ambulatory care device that enables immediate access and bidirectional communication with emergency services, primary care, and hospital units, and close follow-up in situations of decompensation or other non-deferrable care needs for people with diabetes, as an alternative to hospitalization.
Fig. 3 illustrates the clinical and financial impact of implementing an DDH care model at various levels.
Proposal for effective implementation of a diabetes day hospital in the national health systemThe scientific societies involved in this project and FEDE consider that the axes necessary to properly define the model can be summarized in 6 points (A–F). We also present a proposed DDH Service Portfolio in the hospital setting (Fig. 4).
- A
Clinical Scenarios Suitable for DDH Care
- •
New-onset diabetes requiring immediate intensive insulin therapy.
- •
Acute diabetes decompensations or high risk thereof due to intercurrent illness and/or treatment that may provoke hyperglycemia.
- •
Women with pregestational or gestational diabetes requiring immediate insulin therapy and/or treatment adjustment.
- •
Post-discharge support for people with diabetes on insulin therapy who require short-term therapeutic adjustment.
Proposed DDH Service Portfolio. This portfolio can be expanded according to hospital resources and complexity, covering patients with acute hyper- or hypoglycemic decompensations who require continued medical or nursing attention under specialist supervision or prescription for several hours, but not hospitalization.
For patients accessing from emergency services, triage can help determine priority and resource allocation; it is important to note that the DDH is not designed to replace the hospital emergency department for triage prioritization levels (SEMES)5 I to III:
- •
Level I: absolute priority, immediate care without delay.
- •
Level II: very urgent, life-threatening situations. Delay up to 15 minutes.
- •
Level III: urgent but hemodynamically stable, with potential life risk. Maximum delay 60 minutes.
We propose that, using this triage system, inclusion in the DDH be defined for Levels IV and V:
- •
Level IV: minor urgency. Maximum delay 120 minutes.
- •
Level V: non-urgent. Delay up to 240 minutes.
Within Levels IV and V, we can distinguish:
Category 1:
- •
Requires continuous supervision (nurse and physician).
- •
Room with stretcher/recliner, companion chairs, and a cart with basic urgent-care drugs.
Includes:
- •
Stage 3 type 1 diabetes diagnosis (ketosis or non-severe DKA).
- •
Simple hyperglycemia with ketosis; non-severe DKA.
- •
Level 3 hypoglycemia.
- •
Diagnostic tests with hypoglycemia risk.
Category 2:
- •
Requires intermittent supervision (nurse and physician).
- •
Room with stretcher/recliner, companion chairs, and a cart with basic urgent-care drugs.
Includes:
- •
Persistent simple hyperglycemia, ketosis.
- •
Stage 3 type 1 diabetes diagnosis without ketosis.
- •
Pregnant individuals without prior diabetes with frank hyperglycemia.
Category 3:
- •
Requires only the directly involved staff (nurse or physician).
- •
Nurse/physician exam room or group-activity room.
Includes:
- •
Diabetic foot ulcers.
- •
Gestational diabetes requiring initiation of insulin.
- •
Therapeutic education modules, basic or advanced.
- •
Teleconsultations for decompensation or other non-deferrable needs.
- •
Advanced technology follow-up: continuous glucose monitoring (CGM), integrated systems, connected pens.
- B
Lists of Care Processes Offered by the DDH for Adolescents and Adults Referred to Endocrinology & Nutrition (Age cutoffs for pediatric vs adult units will follow each autonomous community’s standards.)
- •
Unscheduled in-person care, ideally within < 24 hours, for suspected type 1 diabetes.
- •
Unscheduled in-person care (24–< 72 hours) for people with diabetes with marked hyperglycemia (HbA1c >10% and/or plasma glucose > 300 mg/dL) with catabolic syndrome or ketonuria.6
- •
Early in-person care (< 72 hours) coordinated with obstetrics/gynecology for women with pregestational diabetes who need immediate insulin initiation or treatment adjustment.
- •
Early in-person care (< 72 hours) coordinated with obstetrics/gynecology for women with gestational diabetes who need immediate insulin initiation or treatment adjustment.
- •
Early in-person care (< 72 hours) coordinated with oncology/hematology/pulmonology/rheumatology/nephrology for patients with diabetes starting glucocorticoids or other hyperglycemia-inducing therapies with high risk of glycemic decompensation.
- •
Early in-person care (< 72 hours) coordinated with the diabetic foot unit for patients with inadequate glycemic control.
- •
Immediate follow-up (<12 hours, in-person or remote) of patients seen in the emergency department for acute hyperglycemic or hypoglycemic decompensations.
- •
Scheduled intermediate follow-up (in-person or remote) after hospital discharge from medical/surgical services for patients with diabetes at risk of decompensation or needing therapeutic adjustment, ensuring continuity with primary care (PC) or hospital care (HC).
- •
Resolution of diabetes-related questions arising in PC and HC via synchronous phone consultations or asynchronous secure email/center-specific channels.
- C
Care Programs an DDH can Incorporate in the Hospital Setting
- •
Initiation of insulin therapy and associated basic diabetes education for people with type 1 diabetes mellitus.
- •
Initiation of insulin therapy and associated basic diabetes education for people with hyperglycemic decompensation with type 2 diabetes mellitus or other types of diabetes not addressed by their PC (primary care) team.
- •
Initiation of insulin therapy and associated basic diabetes education for people with gestational or pregestational diabetes.
- •
Initiation of insulin therapy and associated basic diabetes education for people with hyperglycemic decompensation due to corticosteroids or other therapies not addressed by their PC team.
- •
Therapeutic management with IV fluids and IV insulin—until resolution—for people with simple hyperglycemic decompensation (isolated hyperglycemia, ketotic hyperglycemic decompensation, non-ketotic hyperglycemic decompensation) who do not require parenteral treatment for > 8 hours.7
- •
Early scheduled follow-up after hospital discharge for people with diabetes and inadequate control, until continuity with PC or endocrinology/nutrition clinics is ensured.
- •
Phone and/or telematic care for individuals requiring it due for glycemic instability.
- •
Phone and/or telematic follow-up for those initiating advanced diabetes technologies and/or requiring close monitoring: initiation of continuous subcutaneous insulin infusion or automated insulin delivery systems.
- D
Referral Sources to the DDH
- •
From PC:
- o
Suspected type 1 diabetes diagnosis.
- o
Type 2 diabetes with persistently marked hyperglycemia (HbA1c > 10% and/or plasma glucose > 300 mg/dL) with catabolic syndrome or ketonuria, not felt to require emergency-department management.
- •
From Outpatient Hospital Care (HC):
- o
Pregnant patients with pregestational or gestational diabetes requiring immediate insulin initiation or urgent treatment adjustment.
- o
People with diabetes starting glucocorticoids or other hyperglycemia-inducing treatments with high risk of decompensation.
- •
From any care setting (PC, HC, and emergency services):
- o
People with hyperglycemic decompensations not requiring hospital admission.
- o
People seen in the ED for acute hyper- or hypoglycemic decompensations, ensuring continuity with PC or endocrinology/nutrition clinics.
- o
People with diabetes and inadequate control after discharge from inpatient units, ensuring continuity with PC or endocrinology/nutrition clinics.
- •
From endocrinology/nutrition clinics and/or diabetic foot units:
- o
Followed patients with inadequate glycemic control who, due to instability, require DDH care.
- E
Functional Organization of an DDH in the Hospital Setting
Care requests will be made by phone consultation with the responsible physician when immediate care is required, or via interconsultation when care can be scheduled within < 24–48 hours. Appointments will be managed by administrative staff in endocrinology and nutrition responsible for this activity.
- F
Human and Structural Resources
Human resources:
- •
Hours should adapt to population needs; at minimum full morning coverage is appropriate, with desirable afternoon continuity, ideally reaching at least 12 hours (8:00–20:00).
- •
Endocrinology & Nutrition consultant specialist (CS). Dedicated time may range from 50–100% of regular hours; increased coverage will be needed across all working days.
- •
Diabetes nurse educator (DNE). Estimated dedication 100% of regular hours; increased coverage will be needed across all working days.
- •
Identification of liaison professionals in PC and HC-DDH to facilitate communication across levels.
- •
Nursing care technician (NCT) and an administrative assistant in endocrinology and nutrition.
- •
Contact via pager/phone/email.
- •
Although shareable with other units, at minimum: a clinical assistant, a porter, and an administrative officer.
A desirable additional aspect is staff stability to build team cohesion and patient trust.
Material resources (Table 1):
- •
The DDH should be located within the hospital environment with adequate physical access from the emergency department and inpatient wards.
- •
Structural needs include sufficient space for medical consultations, treatments, and health education. Configuration depends on each center’s availability and whether the space is dedicated to people with diabetes.
- •
An electronic health record (EHR) is essential. It is also advisable that all information generated by diagnostic/treatment devices be digitized so results are automatically incorporated into the EHR.
Recommended material resources for the diabetes day hospital.
| Spaces | Equipment |
|---|---|
| Medical consultation |
|
| Nursing consultation |
|
| Assessment and treatment room | Essential equipment
|
Desirable equipment
| |
| Group education room (desirable) |
|
| Office |
|
Non-in-person activity:
- •
Non-in-person modes should be incorporated to adapt the device to deliver services wherever the patient is, using telemedicine and digital health tools. A protocolized assessment is needed to ensure quality and safety.
- o
Patient competent to participate and who provides consent.
- o
Organizational structure: scheduled appointments and an appropriate platform.
- o
Integration with the EHR and interoperability with other diabetes-management applications.
- o
Clinical situations that may require conversion to conventional in-person care.
- o
Inclusion of structure, process, and outcome indicators.
- o
Ideally, teleconsultation should be conducted in accordance with the specific standard (UNE teleconsultation standard: CTN-UNE 179/GT 17 “Teleconsulta”).8
- o
SEEN’s Teleconsultation Manual provides structured information on applying this care modality in endocrinology and nutrition, including for people with diabetes.9
Current, more complex diabetes care models require adapting their service portfolios, care programs, and structural/staffing needs to patient needs.
New nursing care roles also need to be launched and recognized to ensure that professionals in these posts have the necessary training and competencies.
These care models are, by their nature, ideal settings for high-quality clinical research and for specialized and continuing education of different professionals.
Similarly, the physical space must also be appropriate to meet care needs.
In short, DDHs can contribute significantly to improving quality of life for people with diabetes, reducing acute and chronic complications, and decreasing emergency visits and hospital admissions.
They can also help generate long-term cost savings, promote digital-health innovation in diabetes care, and enhance bidirectional communication with both patients and professional teams.