Vitamin D is a hot topic in clinical practice and research, as well as for the general public. Vitamin D intake is recommended in alternative medicine, allopathic medicine and even social circles. Today, general laboratory testing, for any reason, that lacks assessment of 25-hydroxycholecalciferol, 25-hydroxyvitamin D or calcifediol (25-OHD) to determine vitamin D status appears to be incomplete. The intake of vitamin D as a nutritional product or prescription drug and the use of reagents to determine blood 25-OHD levels have been expanding greatly for years.1,2 Its recommendation goes beyond bone disease. However, there is a great deal of scientific debate regarding many aspects of vitamin D: serum levels, clinical usefulness outside of bone disease, screening, monitoring, dosing and routes of administration.
Vitamin D has traditionally been considered a nutrient. However, this label does not capture its full potential. It is also a lipophilic secosteroid produced in the skin through sun exposure; no more than 20% of it is of dietary origin. It is first hydroxylated in the liver, by 25-hydroxylase, to produce 25-OHD, which is taken by consensus to be a marker of vitamin D status. Regulation of 25-hydroxylase enzyme activity is not well understood. The active metabolite of vitamin D is produced when it again undergoes 1α-hydroxylation, primarily in the kidneys but also in other tissues, to form 1-25 dihydroxycholecalciferol or calcitriol (1,25-OHD). This has paracrine and autocrine activity, hence the concept of vitamin D as a hormone. Unlike 25-hydroxylase, 1α–hydroxylase is very tightly regulated. Both 25-OHD and 1,25-OHD are once again hydroxylated by the D-24-hydroxylase present in multiple tissues to form the inactive metabolite 1,24,25-OHD.3
Receptors for vitamin D have been found in cytoplasm and cell nuclei in the bone, kidneys, parathyroid glands, adipocytes, muscles, gut, pancreas, retinas, brain, pituitary gland, lungs, breasts, cardiac muscle, vasculature and colon. It is directly or indirectly linked to 3% of the genome.4 1,25-OHD acts on the tissues by three mechanisms: rapid activity (binding to receptors in cell cytoplasm, thus increasing calcium levels with effects on hormone secretion); binding to nuclear retinoid X receptors (thus modulating gene expression); and, finally, regulating epigenetic changes in different stages of development.5
Numerous genetic, molecular, cellular and in vivo studies have suggested that vitamin D is pleiotropic, with effects on cell proliferation and immune-system, muscle, reproductive, vascular and metabolic function.6,7 Observational studies in humans have demonstrated an inverse relationship between 25-OHD levels and various non-bone diseases, all with the common denominator of inflammation to a greater or lesser degree.8,9 Therefore, although a link between the vitamin D endocrine system and the pathophysiology of some clinical conditions is highly plausible, randomised controlled trials (RCTs) are needed to confirm it. However, to date, RCTs and Mendelian randomisation studies have been inconclusive, inconsistent and in some cases contrary to causal association.5,10
In epidemiology, correlation is not proof of causation, and there is uncertainty as to whether the relationship between vitamin D and non-bone disease is causal or whether vitamin D deficiency results from an inflammatory state to a greater or lesser degree.11
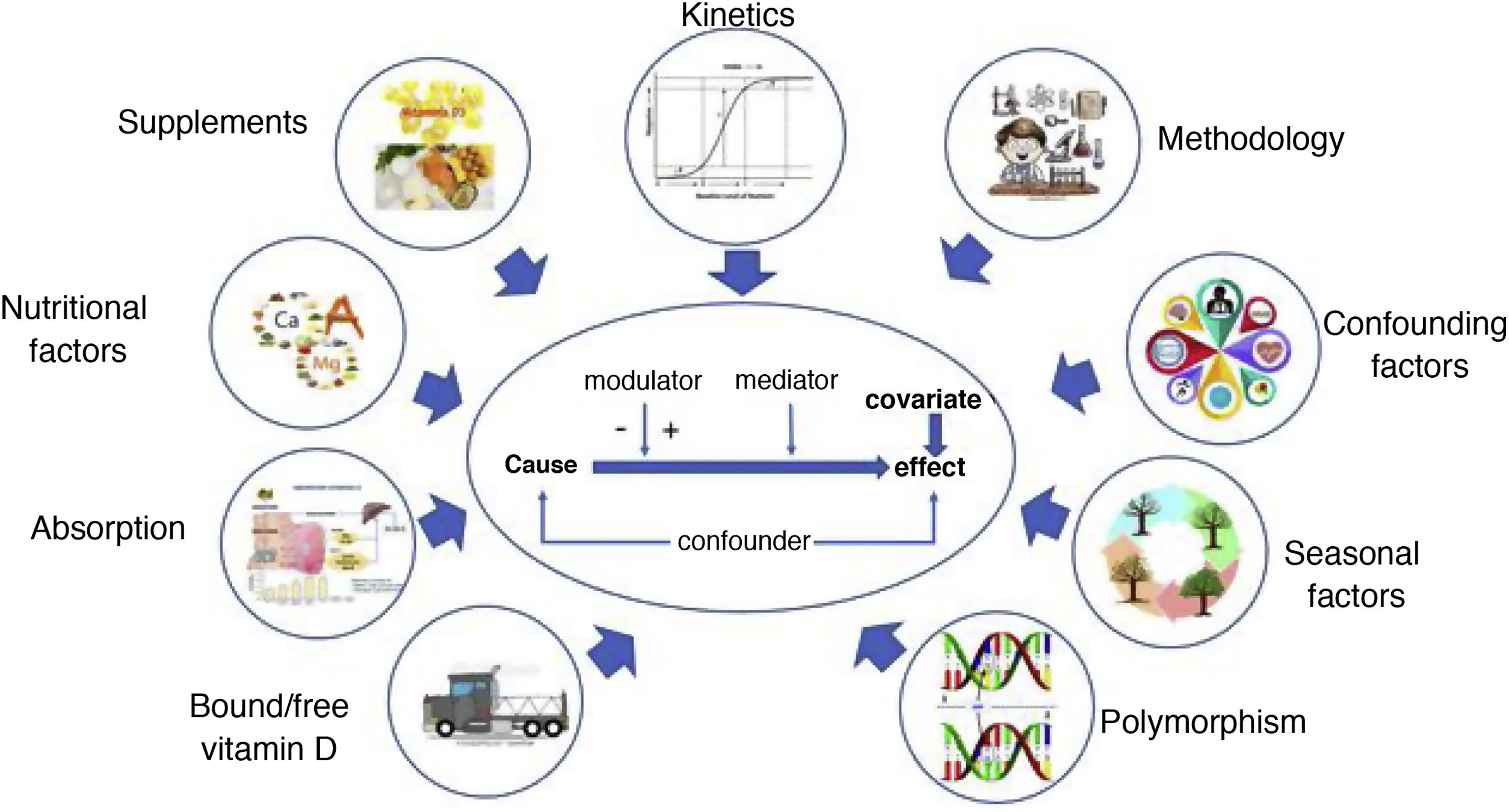
However, other intermediate situations can also occur. According to Autier et al.,8 several hypotheses can be made between the above extremes. One is that ageing is associated with inflammation, disease and lower 25-OHD levels. Another is that age, inflammation and disease decrease 25-OHD synthesis. Yet another is that local inflammation, systemic inflammation or both increase the risk of chronic disease and decrease 25-OHD synthesis, regardless of age. In all of the above situations, lifestyle changes triggered by disease promote decreased 25-OHD levels. Ultimately, vitamin D acts as a factor, confounder, mediator, modulator and covariate, either in isolation or combined in a single process. This behaviour is not at all unusual for a nutrient.
In addition to the above scenarios, other factors must be taken into consideration in debates on RCTs and epidemiological association studies. On the one hand, 25-OHD levels represent a potential confounder. Since the Institute of Medicine (IOM) and the Endocrine Society (ES) issued recommendations in 2011, there has been a struggle to identify the cut-off point. Both scientific institutions determine the value based exclusively on bone health metrics. The IOM established >20ng/ml as a target value based on Dietary Reference Intakes (DRIs) in place of Recommended Dietary Allowance (RDA), both of which are guidelines for nutritional intake in the healthy population. In contrast, the ES established a value of >30ng/ml to ensure 100% bone health. The criteria are not mutually exclusive. The former is useful in population epidemiology studies, and the latter is a clinical criterion; both refer to bone health, not non-bone disease.12,13
On the other hand, meta-analyses and intervention studies have not always used standardised methods of vitamin D measurement, which have shown 7%–19% variability in immunoassay and variability up to 33% higher than the previous method in high-performance liquid chromatography–tandem mass spectrometry (HPLC-TMS). They also have not taken seasonal 25-OHD variations into account, nor have they offered prior data establishing a subject’s actual baseline status.
Vitamin D can be considered a hormone, but its kinetic behaviour is that of a nutrient and, as such, the blood kinetics of its dose-response relationship follow an S-curve (repletion, increase and saturation). Genetic polymorphism modifies absorption, protein binding and vitamin D activation, thus altering the expected dose-response curve for 25-OHD levels with oral administration of vitamin D, with even greater variability than that inherent to measuring methodologies.5
In addition, RCTs do not clearly report intake of other nutrients, such as calcium and magnesium (these are required for proper enzyme activity) as well as vitamin A (this is needed for vitamin D pathway activity, but excess intake antagonises its effects). Furthermore, vitamin D supplement absorption depends on the amount of concomitant fat ingestion and also decreases with age.
Finally, some data have shown that, in obesity and diabetes, liver hydroxylation is decreased and catabolism of 1,25-OHD by 24-OH hydroxylase is increased.5
Taken together, all of the above means that, for a single administered dose, the 25-OHD level reached will be different depending on the baseline value and the subject’s characteristics and lifestyle. Therefore, achieving a similar final 25-OHD level in RCTs is complex with the classic pharmacological method used in clinical trials. To partly get around this problem, the use of calcifediol and calcitriol is recommended, although outcomes of this strategy are also debated at present.5
Are giving a daily dose and giving the same amount of vitamin D in a bolus every one to three months the same for non-bone health? At least in relation to bone health, there is evidence supporting the differences.3
Taken together, data from intervention studies do not suggest that vitamin D intake improves non-bone health in subjects with sufficient vitamin D levels according to bone metrics, while data on deficiencies are limited.14
In conclusion, although it is biologically plausible, at present there is no evidence that vitamin D supplementation has benefits outside of bone health.14 At this time, the gaps in knowledge outweigh and outnumber the evidence. Vitamin D is a complex nutrient with activity similar to that of a hormone as it interacts with numerous factors. The complexity of vitamin D metabolism, polymorphism, its relationship to lifestyle and abnormalities with acute or chronic disease in part account for inconsistencies in RCT results (Fig. 1). The absolute value of an element is important in nutrition, but so too is its relative proportion when referring to overall homeostasis. In this context, distinguishing causality, reverse causality, modulators and mediators is no easy task.
It is not possible to go from hypothesis to conclusion and action without evidence supporting the scientific method, if only to back the notion that supplementation is not harmful and can have major non-bone benefits. If evidence is weighted over experience, then it should be weighted even more heavily over belief.
Please cite this article as: Rodriguez IC, Ballesteros-Pomar MD. Controversia vitamina D y enfermedad: un problema de factores, mediadores, moduladores, marcadores, confusores y covariables. Endocrinol Diabetes Nutr. 2022;69:389–391.