Transient osteoporosis of the hip (TOH) during pregnancy is a rare form of osteoporosis that is sometimes underdiagnosed. The disorder is of a multifactorial origin and should be included in the differential diagnosis of pregnant women with hip pain of sudden onset in the third trimester of pregnancy and occasionally after delivery.
A 36-year-old woman with no relevant personal history reported in week 24 of her first pregnancy due to right inguinal pain with no apparent triggering factor. The pain progressed, becoming bilateral, resulting in functional impotence and making it impossible for the patient to walk. It was exacerbated by movements and responded favorably to rest and to acetaminophen and metamizol. She reported no pain in any other joints.
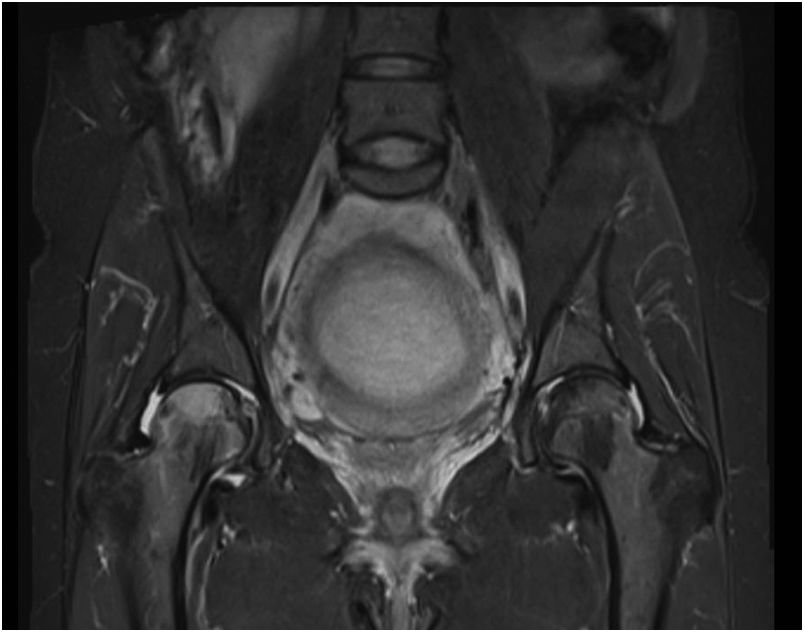
The laboratory tests showed normal calcemia (9.1 mg/dl) and low 25-hydroxy vitamin D levels (7.21 ng/ml). Magnetic resonance imaging (MRI) of the pelvis (Fig. 1) revealed intramedullary edema affecting the head (50 %) and neck of the right femur and the head of the left femur (20 %), with no subchondral changes suggestive of avascular necrosis or fracture. The findings were consistent with TOH.
Conservative management was recommended in this clinical context, with analgesia, weight offloading measures, and calcifediol supplements.
Delivery was induced at term (38 + 5 weeks of pregnancy), with the birth of a male weighing 3600 g by cesarean section (prior cervical dilatation arrest at 8 cm). Puerperium was uneventful.
Breastfeeding started adequately, and the symptoms gradually improved, with complete functional recovery over the following weeks.
Two months after delivery, while continuing treatment with the calcifediol supplements, the blood tests revealed normal calcium metabolism (PTH: 24.6 pg/ml, phosphate: 4 mg/dl, ionic calcium: 4.8 mg/dl, hydroxycholecalciferol: 30.9 ng/ml). On the other hand, the bone remodeling markers were seen to be elevated (beta crosslaps [CTX]: 0.9 ng/ml [<0.57] and procollagen type 1 N-terminal propeptide [P1NP]: 114.3 ng/ml [15.13–58.59]). Bone densitometry indicated “low bone mass” (Z-score: −2.7) in the hip. Complementing the treatment with 1 g of calcium a day was advised.
Five months after delivery, the patient was free of symptoms. The markers had decreased yet remained elevated, particularly those indicative of bone formation (CTX: 0.6 ng/ml; P1NP: 89 ng/ml). Magnetic resonance imaging confirmed the complete resolution of the bone edema. Since breastfeeding was maintained, the patient was advised to continue with the calcium and calcifediol supplements.
After one year the condition had completely resolved.
Transient osteoporosis of the hip (TOH), also known as bone marrow edema syndrome, is a rare form of osteoporosis that affects some women in the third trimester of pregnancy, and less commonly after delivery.1 The estimated incidence of TOH is 4 cases per million pregnant women.2 Its etiology is multifactorial, and the different described causes include trabecular microfractures secondary to decreased bone mass in pregnancy, circulatory changes, and compression of the obturator nerve or of the pelvic sympathetic nerves caused by the gravid uterus, immobility, dental problems in childhood, and a lack of exercise before and after puberty.3,4 The absorption of calcium in the intestine doubles during pregnancy to meet fetal calcium demands. However, if calcium intake is insufficient, the maternal skeleton will suffer bone resorption during the third trimester of pregnancy. During lactation, various hormonal changes independent of calcium intake result in a 5–10% loss of bone mineralization in order to supply calcium in breast milk. Bone mineralization and strength are restored after the cessation of lactation.3
Transient osteoporosis of the hip usually starts as sudden pain in a hip (usually on the left side due to fetal cephalic presentation, but occasionally in both hips), with no apparent cause.5 The pain is secondary to edema of the femoral head.
Magnetic resonance imaging is the diagnostic gold standard, and is able to detect changes within 48 h of the onset of symptoms.6 The typical finding is edema of the femoral head,7 with decreased signal intensity in T1- and increased intensity in T2-weighted sequencing. Bone densitometry in turn shows a decrease in bone mineral density in the femoral heads.
Treatment is based on weight offloading measures, rehabilitation and analgesia.
Both the symptoms and the radiographic findings usually resolve with no sequelae in the first year after delivery, with no need for antiresorptive drug treatment, though some cases may be complicated by avascular necrosis or fracture of the femoral head.8 The risk of recurrence in subsequent pregnancies increases after a first episode. However, since TOH is not a systemic disorder, antiresorptive treatments are not recommended, due to the effects they may have upon the fetus or newborn infant, such as altered bone mineralization, premature delivery, low birth weight, transient hypocalcemia or even fetal death. Nevertheless, it has been reported that such treatments could shorten the duration of the symptoms.3,6,9–11
Obstetric management should be individualized, with an expectant approach to term generally being adopted, but with induction being warranted in those cases where conservative management proves insufficient. As regards the delivery route, vaginal delivery is not contraindicated, but the risk of fracture may increase, particularly when associated with epidural anesthesia.12
Regarding subsequent follow-up, while few data are available in the literature, recurrence may occur in subsequent pregnancies, though parity does not appear to increase the fracture risk.13 Magnetic resonance imaging and bone densitometry are recommended after 12–18 months to assess the resolution of the condition,3 with a continuation of vitamin D supplements until blood values return to normal.14,15
Although TOH a rare condition, it should be included in the differential diagnosis of patients with sudden pain in one or both hips during the third trimester of pregnancy or after delivery. Magnetic resonance imaging is the gold standard for establishing the diagnosis. Transient osteoporosis of the hip is a self-limiting disorder, and its treatment is based on weight offloading measures, rehabilitation and analgesia.
Please cite this article as: Carriles Rivero I, Aubá Guedea M, Chacón Cruz E, Sifontes NM, Galofré JC. Osteoporosis transitoria de cadera en el embarazo. Endocrinol Diabetes Nutr. 2019;66:590–591.