To assess the diagnostic performance of neck ultrasound examination performed by endocrinologists to locate parathyroid adenomas in patients with primary hyperparathyroidism (PHPT).
MethodologyA retrospective observational study in 135 patients (mean age, 60.0±12.3 years; 74.8% females) seen at endocrinology for PHPT (mean calcium level, 11.3±1.2mg/dl and mean PTH level, 240.4±346.8pg/ml) who underwent neck ultrasound examinations at the endocrinology department. 99mTc-MIBI parathyroid scintigraphy was performed before surgery in all patients. Sensitivity, specificity, positive predictive value, and negative predictive value were calculated in surgical patients.
ResultsNinety-eight patients underwent surgery for PHPT and 97.8% were cured at 6 months. Parathyroid ultrasound had a sensitivity of 85% (95% CI: 75.7%–91.2%) and a positive predictive value (PPV) of 95.2% (95% CI: 87.5%–98.4%) to locate parathyroid adenomas 1.7±0.9cm in maximum diameter (69.4% in smaller glands), showing a high correlation (r=0.661 and r=0.716) with maximum diameter and volume of the excised adenoma. Sixty percent of patients had nodular thyroid disease (64.2% bilateral nodules with mean maximum diameter of 1.5±0.9cm), and thyroidectomy was performed in 31.6%. The highest diagnostic performance was seen with a combination of neck ultrasound and 99mTc-MIBI scintigraphy (sensitivity: 96.8% and PPV: 95.8%).
ConclusionIn our area, parathyroid adenoma localization with ultrasound performed by endocrinologists has a high diagnostic yield and allows for detecting nodular thyroid disease in 60% of patients.
Evaluar el rendimiento diagnóstico de la ecografía de localización de adenomas de paratiroides realizada por endocrinólogos en pacientes con hiperparatiroidismo primario (HPTP).
MetodologíaEstudio observacional retrospectivo en 135 pacientes (74,8% mujeres; edad media: 60,0±12,3 años) atendidos en consultas de endocrinología por HPTP (calcemia media: 11,3±1,2mg/dl y PTH plasmática media: 240,4±346,8pg/ml) a los cuales se realiza eco cervical en consulta de endocrinología y se solicita gammagrafía 99mTc-MIBI previamente a la cirugía. Se calcula sensibilidad, especificidad y valor predictivo de ambas pruebas en el subgrupo de pacientes intervenidos.
ResultadosUn total de 98 pacientes fueron intervenidos de HPTP y se curaron el 97,8% a 6 meses. La ecografía de localización tuvo una sensibilidad del 85% (IC 95%: 75,7-91,2%) y un valor predictivo positivo (VPP) del 95,2% (IC 95%: 87,5-98,4%) para localizar adenomas de paratiroides de 1,7±0,9cm de diámetro medio máximo (69,4% en glándulas inferiores), presentando una elevada correlación (r=0,661 y r=0,716) con el diámetro máximo y el volumen del adenoma extirpado. El 60% presentaba patología nodular tiroidea (64,2% bilateral con un diámetro máximo medio nodular de 1,5±0,9cm) y se realizaron tiroidectomías en el 31,6%. El mayor rendimiento diagnóstico se observó con la combinación de eco cervical y gammagrafía 99mTc-MIBI (sensibilidad: 96,8% y VPP: 95,8%).
ConclusiónEn nuestro medio, la ecografía de localización de adenomas de paratiroides en pacientes con HPTP realizada por endocrinólogos tiene una elevada capacidad diagnóstica y permite detectar la presencia de patología tiroidea en el 60% de los pacientes.
Primary hyperparathyroidism (PHPT) is the most common cause of hypercalcemia and affects at least one in every 1000 people. Its incidence moreover increases with age.1,2 Although most patients with PHPT are asymptomatic at the time of diagnosis,1 in cases of moderate to severe PHPT an increased risk of death due to cardiovascular disease has been reported. This risk moreover remains high even years after successful parathyroidectomy, suggesting that the cardiovascular damage caused may be irreversible.3
Although imaging studies are not useful for confirming or excluding the diagnosis of PHPT, and imaging test positivity or negativity should not be used to select patients eligible for parathyroidectomy,1,4 most clinical practice guidelines currently recommend such tests before parathyroidectomy, with the purpose of locating anomalous parathyroid lesions (thereby facilitating minimally invasive surgery) and of assessing the possibility of concomitant thyroid disease.4–7 In this regard, the main preoperative abnormal parathyroid tissue localization tests are ultrasound, parathyroid scintigraphy and computed axial tomography (CAT) or four-dimensional CAT. The use of one technique or another depends on both the availability and the diagnostic performance of these tools in each healthcare center.1,2,5 However, most studies report the diagnostic strategy with the greatest cost-effectiveness to be neck ultrasound, performed by an experienced examiner, combined with 99mTc-MIBI (sestamibi) scintigraphy.4,8–10
A recent systematic review has reported that the sensitivity of ultrasound in locating anomalous parathyroid lesions ranges from 55 to 88%, with a positive predictive value (PPV) of 93–97% and a diagnostic accuracy of 88%.11 These results depend on the experience of the examiner, the number of ectopic lesions, the coexistence of multinodular goiter or autoimmune thyroiditis, and the presence of lymph nodes or other neck lesions that could be confused with parathyroid adenomas.6,11 Although neck ultrasound in patients with PHPT is usually performed by radiologists, recent studies have shown high success rates in locating parathyroid adenomas when ultrasound is performed by surgeons12–15 and endocrinologists,16,17 though none of these studies were carried out in Spain. For this reason, the primary objective of the present study was to assess the diagnostic performance of neck ultrasound performed in our center by endocrinologists in patients with PHPT.
Material and methodsA retrospective observational study was carried out at the Endocrinology Unit of Hospital Universitario Puerto Real (Cádiz, Spain), involving the analysis of biochemical, ultrasound, surgical and histological data from 135 patients examined for PHPT between January 2013 and December 2018. The study was approved by the Research Ethics Committee of Cádiz in April 2018, and no informed consent was required to access the study data.
All patients with biochemical criteria of PHPT (hypercalcemia with high or inappropriately normal parathyroid hormone (PTH) levels, usually associated with hypophosphatemia and hypercalciuria) subjected to neck ultrasound in endocrinology clinics, and regardless of whether they underwent subsequent surgery or not, were considered eligible to participate in the study. Patients previously operated upon due to PHPT, those with tertiary PHPT criteria, and patients in whom neck ultrasound was not performed in endocrinology clinics, were excluded from the study.
Laboratory testsCalcium, phosphorus, total proteins, urea, creatinine, PTH, 25-OH-vitamin D and calciuria were documented in all patients. The serum calcium concentration was adjusted for the plasma protein level. Calcium, phosphorus, total proteins, urea and creatinine levels were measured using a Cobas Integra 800 autoanalyzer (Roche Diagnostics, Basel, Switzerland), while PTH levels were measured using in vitro immunological analysis based on electrochemoluminescence with an Elecsys E 170 automated analyzer (Roche Diagnostics) (reference levels: 15–65pg/ml).
Neck ultrasoundAll patients underwent neck ultrasound exploration in the endocrinology clinic by the same examiner in a single intervention, using Sonosite Micromax and Hitachi Aloka F37 ultrasound devices with 10–18MHz transducers, with the intention of locating lesions suggesting parathyroid adenomas. Such lesions usually present as well-defined and hypoechoic oval, polygonal or triangular nodules located posterior to the upper or lower pole of both thyroid lobes, though larger adenomas may be multilobulated, present calcifications, or show cystic degeneration.5,18 If no lesions were found in these locations, ultrasound examination was extended to the rest of the neck to the upper mediastinum. Ultrasound lesions consistent with parathyroid adenomas were classified as single or multiple and located as follows: upper right, lower right, upper left, lower left, intrathyroidal (right/left) or ectopic (description). The longitudinal (L), transverse (T), and anteroposterior (AP) diameters of all the adenomas were measured (cm), and ultrasound volume was calculated (cm3) using the formula: [(L×T×AP)×3.1416/6].
Technetium-99m MIBI (methoxyisobutylisonitrile) scintigraphyIn cases of confirmed PHPT, a 99mTc-MIBI (sestamibi) scan was requested from the Nuclear Medicine Unit of Hospital Puerta del Mar (Cádiz, Spain), because this technique is not available at our center. In all cases, 15mCi of 99mTc-MIBI was administered via the intravenous route to obtain early (15min) and late images (2–3h) of the neck and thorax. The reports of results with images consistent with parathyroid adenomas were classified as single or multiple lesions and located on an excluding basis in the following locations: upper right, lower right, upper left, lower left, intrathyroidal (right/left) or ectopic. In three patients with negative MIBI findings, the study was expanded with SPECT-CT, resulting in positivity in one case and negativity in the other two patients. All three cases were considered to be “MIBI-negative”.
Surgical indication and cureIn all cases, the indication of parathyroid surgery was individualized and decided upon at a joint session with general surgery. The following general criteria were taken into account: age <50 years, calcemia >1mg/dl of the upper range of normal, the presence of associated complications (renal lithiasis, osteoporosis, a glomerular filtration rate [GFR] <60ml/min) or patient surgical preference. The parathyroid surgical approach was established preoperatively based on the imaging findings. Focal minimally invasive surgery was indicated for single adenomas, while a wider surgical approach was used for hemithyroidectomy or total thyroidectomy due to the presence of associated nodular thyroid disease. All patients underwent surgery at the Department of General Surgery of our hospital, except those with intrathoracic ectopic adenomas, who underwent surgery at the Thoracic Surgery Unit of Hospital Puerta del Mar (Cádiz, Spain). In no cases was an intraoperative PTH measurement made. The surgical specimens were analyzed by the Pathology Unit at both centers, with the histological results, maximum diameter (cm) and volume (cm3) being recorded. The operated patients continued follow-up until there was a biochemical cure, as defined by the American Association of Endocrine Surgeons (normalization of corrected serum calcium levels at least 6 months after parathyroidectomy).4 Single parathyroid adenoma was defined by the surgical removal of a single parathyroid lesion, and when the patient was cured. Multiple parathyroid disease was established either from histological confirmation of the presence of more than one parathyroid gland (adenoma or hyperplasia) or when the patient was not cured following the removal of a single lesion.
Evaluation of the imaging studiesThe ultrasound and MIBI findings were considered to be concordant if they located a parathyroid adenoma in the same location, or if both tests proved negative. Based on the results of the imaging studies, surgical exploration, histology and laboratory test findings, all patients subjected to surgery were classified as follows19,20: (1) true positive (TP) result: a single adenoma located by ultrasound, scintigraphy or both, with a location confirmed at surgery and the histology study, and with cure criteria after surgery. In the case of more than one adenoma, a true positive result was considered if two or more anomalous locations were identified in the imaging studies and were confirmed at surgical exploration; (2) false positive (FP) result: a single adenoma located by ultrasound, scintigraphy or both, but not located at surgery or found in a location different from that specified, or when the imaging studies revealed two or more anomalous locations and the patient was cured after the removal of a single parathyroid lesion; (3) true negative (TN) result: an absence of pathological images at ultrasound, scintigraphy or both, and no identification of pathological parathyroid lesions at surgery; (4) false negative (FN) result: an absence of pathological images at ultrasound, scintigraphy or both, but with one or more adenomas identified at surgery and confirmed by the histopathological study. Alternatively, imaging study identification of a single lesion, but with the detection at surgery of more than one altered gland, or results in which the imaging studies detected a single adenoma that was surgically removed, but the patient failed to cure, thus implying the presence of one or more still not located anomalous glands.
Statistical analysisThe statistical analysis was carried out using the SPSS version 12.0 statistical package for MS Windows. The Shapiro–Wilk test was used to determine whether continuous variables were normally distributed or not. Results of continuous variables were reported as the mean±standard deviation (SD), and of qualitative variables as absolute numbers and percentages. After verifying normal distribution, the Student t-test or analysis of variance (ANOVA) was used for the comparison of quantitative variables, and the chi-squared test or Fisher's exact test was used for the comparison of qualitative or categorical variables. Correlation studies were performed using the Pearson or Spearman test. Statistical significance was considered for p<0.05. Sensitivity, specificity, PPV and negative predictive value (NPV) were calculated for each imaging study modality, separately or in combination. Sensitivity was calculated with the formula TP/(TP+FN), specificity as TN/(TN+FP), PPV was calculated with the formula TP/(TP+FP), and NPV with the formula TN/(TN+FN). The corresponding 95% confidence interval (95% CI) was assessed in all estimates.
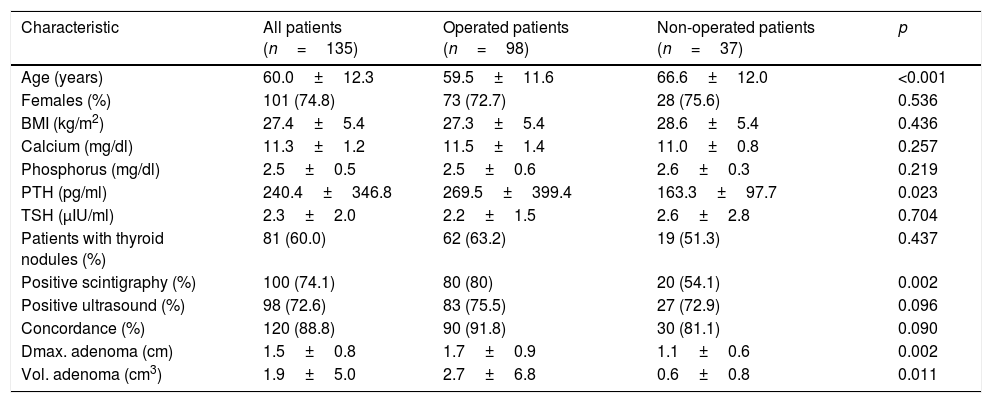
ResultsOf the 135 patients with biochemical criteria of PHPT, 37 (27.4%) have not been operated upon to date: 7 patients are on the waiting list, 11 have been rejected because they do not meet surgical criteria, 8 have been rejected because of advanced age (over 80 years), three due to high surgical risk, 6 due to negative imaging study results, and two patients died during follow-up. As seen in Table 1, a total of 72.6% and 74.1% of all the studied patients had positive ultrasound and scintigraphy location findings, respectively, and there was 88.8% agreement between the two tests. Patients with non-operated PHPT were older, had lower PTH levels, smaller parathyroid adenomas, and were less likely to have positive scintigraphy and ultrasound findings, though statistical significance was not reached in the latter case.
Clinical, biochemical and imaging characteristics of the patients with PHPT.
| Characteristic | All patients (n=135) | Operated patients (n=98) | Non-operated patients (n=37) | p |
|---|---|---|---|---|
| Age (years) | 60.0±12.3 | 59.5±11.6 | 66.6±12.0 | <0.001 |
| Females (%) | 101 (74.8) | 73 (72.7) | 28 (75.6) | 0.536 |
| BMI (kg/m2) | 27.4±5.4 | 27.3±5.4 | 28.6±5.4 | 0.436 |
| Calcium (mg/dl) | 11.3±1.2 | 11.5±1.4 | 11.0±0.8 | 0.257 |
| Phosphorus (mg/dl) | 2.5±0.5 | 2.5±0.6 | 2.6±0.3 | 0.219 |
| PTH (pg/ml) | 240.4±346.8 | 269.5±399.4 | 163.3±97.7 | 0.023 |
| TSH (μIU/ml) | 2.3±2.0 | 2.2±1.5 | 2.6±2.8 | 0.704 |
| Patients with thyroid nodules (%) | 81 (60.0) | 62 (63.2) | 19 (51.3) | 0.437 |
| Positive scintigraphy (%) | 100 (74.1) | 80 (80) | 20 (54.1) | 0.002 |
| Positive ultrasound (%) | 98 (72.6) | 83 (75.5) | 27 (72.9) | 0.096 |
| Concordance (%) | 120 (88.8) | 90 (91.8) | 30 (81.1) | 0.090 |
| Dmax. adenoma (cm) | 1.5±0.8 | 1.7±0.9 | 1.1±0.6 | 0.002 |
| Vol. adenoma (cm3) | 1.9±5.0 | 2.7±6.8 | 0.6±0.8 | 0.011 |
cm: centimeters; Dmax: maximum diameter; PHPT: primary hyperparathyroidism; BMI: body mass index; PTH: parathyroid hormone; TSH: thyroid-stimulating hormone; vol.: volume.
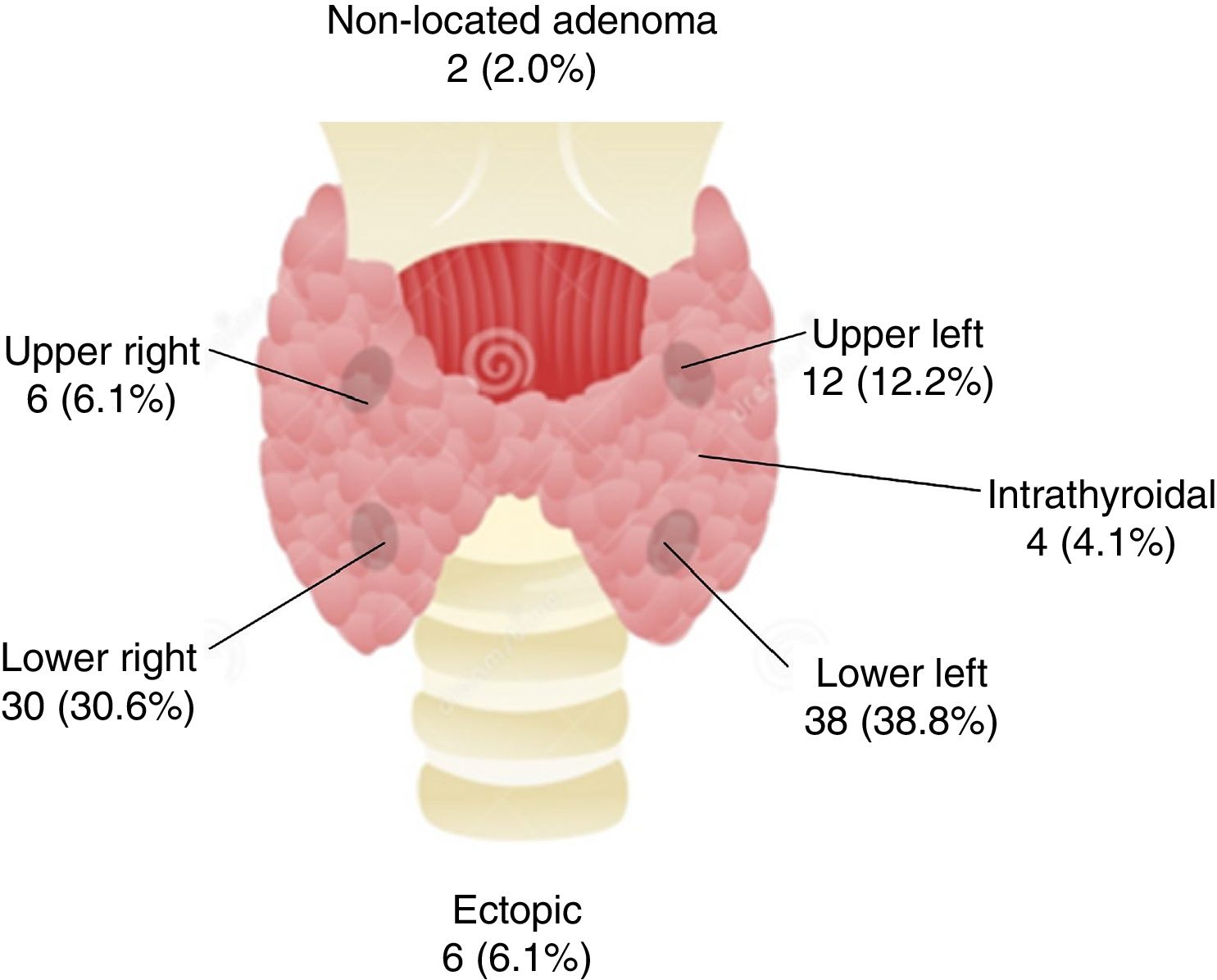
A total of 98 patients underwent surgery, and 100 parathyroid lesions were removed (91 parathyroid adenomas, 8 parathyroid hyperplasias, and one parathyroid lipoadenoma). Anomalous lesions were not located in two patients who currently remain classified as uncured PHPT. Among the operated patients, almost 70% of the parathyroid adenomas were located in the lower glands, with the removal of four intrathyroidal adenomas and 6 ectopic adenomas (Fig. 1). The removed adenomas presented a maximum diameter of 1.8±1.1cm (0.5–9.0cm) and a mean volume of 3.38±14.2cm3 (0.05–82.4cm3). A strong correlation was recorded between the ultrasound maximum diameter and ultrasound volume on the one hand and the histopathological maximum diameter (r=0.661 and r=0.582; both p<0.001) and volume of the removed adenoma on the other (r=0.716 and r=0.703; both p<0.001).
Sixty percent of the patients had thyroid nodules (26 patients with uninodular disease and 55 with multinodular disease). In most of the cases (64.2%; 54 patients) the nodules were found in both lobes, and the mean maximum diameter of the detected thyroid nodules was 1.5±0.9cm. Twenty-two patients (28.6%) had nodules measuring 2cm in size or more. Thyroidectomy was accordingly performed in 31 patients (31.6%) (12 total thyroidectomies and 19 hemi-thyroidectomies). Three patients (3%) were found to have papillary thyroid carcinoma measuring 1.3–1.9cm in size, as single lesions, with no adenopathies (stage I).
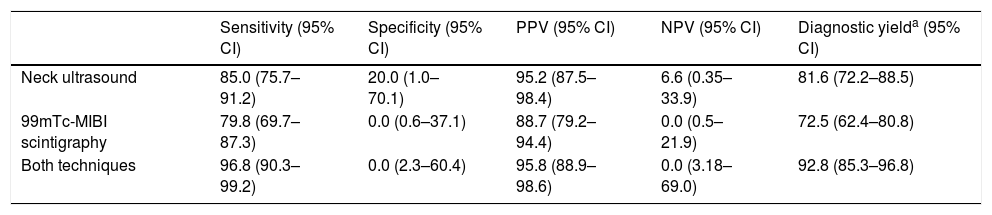
As seen in Table 2, both ultrasound and scintigraphy showed high sensitivity (85% and 79.8%, respectively) and PPV (95.2% and 88.75%). Diagnostic yield proved greater when both diagnostic procedures were used (sensitivity: 96.8% and PPV: 95.8%). Lastly, at 6 months after surgery, 97.8% of the patients had biochemical criteria of PHPT cure (90 out of 92 patients), and calcemia (11.5±1.5mg/dl vs. 9.4±0.6mg/dl; p<0.001), phosphatemia (2.5±0.7mg/dl vs. 3.3±0.5mg/dl; p<0.001) and plasma PTH (280.0±434.3pg/ml vs. 75.7±45.5pg/ml; p<0.001) had changed significantly.
Diagnostic performance of ultrasound, sestamibi scintigraphy, and both tests combined, in the operated patients (n=98).
| Sensitivity (95% CI) | Specificity (95% CI) | PPV (95% CI) | NPV (95% CI) | Diagnostic yielda (95% CI) | |
|---|---|---|---|---|---|
| Neck ultrasound | 85.0 (75.7–91.2) | 20.0 (1.0–70.1) | 95.2 (87.5–98.4) | 6.6 (0.35–33.9) | 81.6 (72.2–88.5) |
| 99mTc-MIBI scintigraphy | 79.8 (69.7–87.3) | 0.0 (0.6–37.1) | 88.7 (79.2–94.4) | 0.0 (0.5–21.9) | 72.5 (62.4–80.8) |
| Both techniques | 96.8 (90.3–99.2) | 0.0 (2.3–60.4) | 95.8 (88.9–98.6) | 0.0 (3.18–69.0) | 92.8 (85.3–96.8) |
99mTc-MIBI: sestamibi; 95% CI: 95% confidence interval; NPV: negative predictive value; PPV: positive predictive value.
The results of the present study show that in our setting, ultrasound location performed by endocrinologists shows a sensitivity and PPV for the detection of suspected parathyroid adenomas of 85% and 95%, respectively. This is in line with the performance figures documented in previous studies involving radiologists, with sensitivity and PPV data ranging from 70.4 to 88.0% and 90.7 to 97.0%, respectively.6,11,21–23 Ultrasound parathyroid adenoma location studies published by endocrinologists are currently anecdotal, with results similar to our own.16,17 In a retrospective study, a group of Turkish endocrinologists reported a sensitivity for the ultrasound location of parathyroid adenomas of 65%. This constituted an improvement upon the results of the radiologists at their center, in that they were able to correctly locate 19 cases of parathyroid adenomas not seen by the radiologists.17 Our study confirms the predominance of adenomas located in the lower parathyroid glands (69%) versus the upper parathyroid glands (18%), in agreement with other authors reporting that approximately 85% of all adenomas are located in the lower parathyroid glands, and more often at the left lower level.16,24 With regard to size, the operated parathyroid adenomas had a mean maximum diameter of 1.8±1.1cm, which is slightly greater than that reported in other similar studies.25 In our series, 4% of the patients presented intrathyroidal parathyroid adenomas. This figure is similar to that reported by other authors.26 Likewise, 6% were ectopic adenomas (50% in the mediastinum), which is in agreement with the results of other studies where the prevalence of ectopic adenomas ranged from 3.7 to 18.6%.16,19,20
Ultrasound location also allowed us to establish that 60% of our patients had thyroid nodules. This finding is consistent with the results of other studies reporting prevalence rates of nodular disease in patients with PHPT of 15–66%,21,27,28 which conditions an increase in thyroidectomy indications in patients with PHPT, reaching as high as 76% in the study published by Cuhaci et al.21 (versus 31.6% of thyroidectomies in our series). In our series we detected three cases of papillary thyroid carcinoma (3% of the patients). This figure is lower than that reported in similar studies,21,28 in which 13–20% of all patients subjected to joint parathyroidectomy and thyroidectomy presented malignant thyroid disease. This supports the need for ultrasound evaluation of the thyroid gland prior to PHPT surgery, since a delay in thyroid lesion surgery may result in increased morbidity associated with second surgical neck exploration.29
In agreement with most studies, our results show that ultrasound location and sestamibi scintigraphy exhibit similar effectiveness to first-line parathyroid location techniques, but that the combination of both techniques is the strategy offering the best results.4,8–10 Ultrasound has the advantages of low cost, widespread availability in clinics, and the absence of exposure to ionizing radiation. It is also more likely to offer a better location of the quadrant and side of the lesion, allowing the identification and categorization of thyroid nodules, adenopathies, and other neck structures, though it is true that ultrasound sensitivity is strongly dependent on the experience of the examiner.30 On the other hand, scintigraphy can detect parathyroid adenomas not identified by ultrasound, confirm ultrasound diagnostic suspicion (particularly in patients with multinodular goiters or with small parathyroid adenomas), and more likely detect ectopic adenomas.6 Thus, when the images provided by ultrasound and scintigraphy are concordant, the PPV for the correct location of a parathyroid adenoma is usually greater than 95%,6 as was seen in our series.
Our study has limitations. Firstly, mention must be made of its retrospective design. Secondly, since ultrasound was performed by the same operator, we avoided interobserver variability, though this could limit any generalization of the results, considering that there is a strong correlation between observer experience and ultrasound location positivity.4,11 Thirdly, analysis of the diagnostic capacity of the imaging tests was only performed in the subgroup of operated patients, who possibly have a greater chance of adenoma location at surgery because the lesions are larger than in non-operated patients. However, this may also be considered a strength of our study for two reasons: firstly, because we described the results of ultrasound location in patients with PHPT not subjected to surgery – this being exceptional in the literature – and secondly, because in our series the ability of ultrasound to identify suspect parathyroid adenomas did not differ between operated or non-operated patients. Lastly, our study did not analyze the factors that could influence the positivity or negativity of the imaging tests, such as the coexistence of nodular disease or thyroid autoimmunity, among others.
In conclusion, it should be possible to have parathyroid ultrasound performed on patients with PHPT in endocrinology clinics by experienced examiners. This would allow not only the reliable location of suspected parathyroid adenomas, but also the identification, categorization and needle biopsy of thyroid nodules (where indicated), in some cases facilitating the indication of thyroidectomy concomitant to parathyroid surgery.
Financial supportThis study was partially supported by unconditional research grants from Laboratorios Menarini, S.A. and the Andalusian Society of Endocrinology, Diabetes and Nutrition (Sociedad Andaluza de Endocrinología, Diabetes y Nutrición [SAEDYN]).
Conflicts of interestThe authors declare that they have no conflicts of interests in relation to the objective or the results of this article.
Please cite this article as: Carral F, Ayala MdC, Jiménez AI, García C, Robles MI, Vega V. Elevada capacidad de localización ecográfica de adenomas paratiroideos en endocrinología (estudio ETIEN 4). Endocrinol Diabetes Nutr. 2020;67:272–278.