Colorectal cancer (CRC) is the most frequently diagnosed malignant tumor in Spain in both sexes, while it is the second most frequent in women, after breast cancer, and the third in men, after prostate and lung cancer.1
More than one-third of patients will present distant metastasis. The most frequent locations are the liver and lungs,2 although metastases may occasionally present in less common locations.
Techniques for locating non-palpable tumors in breast cancer have been recently developed, including radioactive techniques like 125I seeds and the more recent non-radioactive paramagnetic iron oxide seeds. However, the use of these techniques for the localization and subsequent excision of non-palpable lesions is not exclusive to breast cancer, and their use has also been described for non-palpable lesions of other tumors.3
The objective of this article is to present a new technique for locating CRC lymph node metastasis using interpectoral magnetic markers.
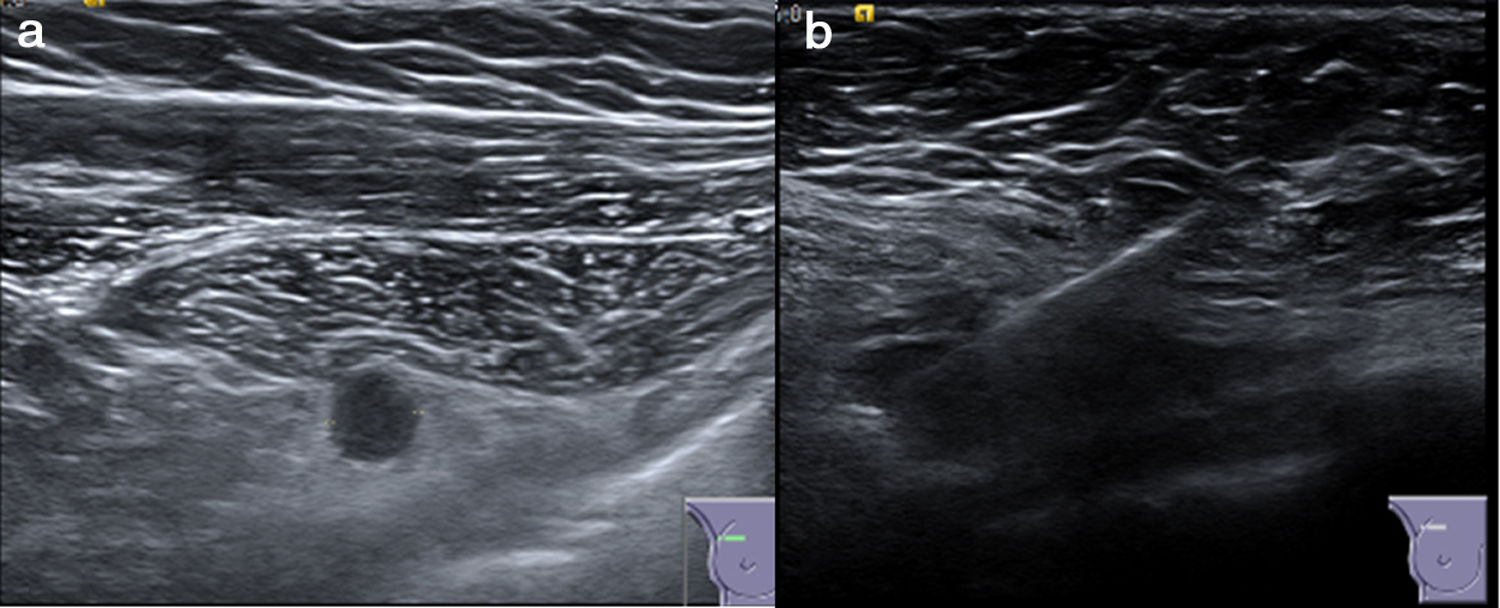
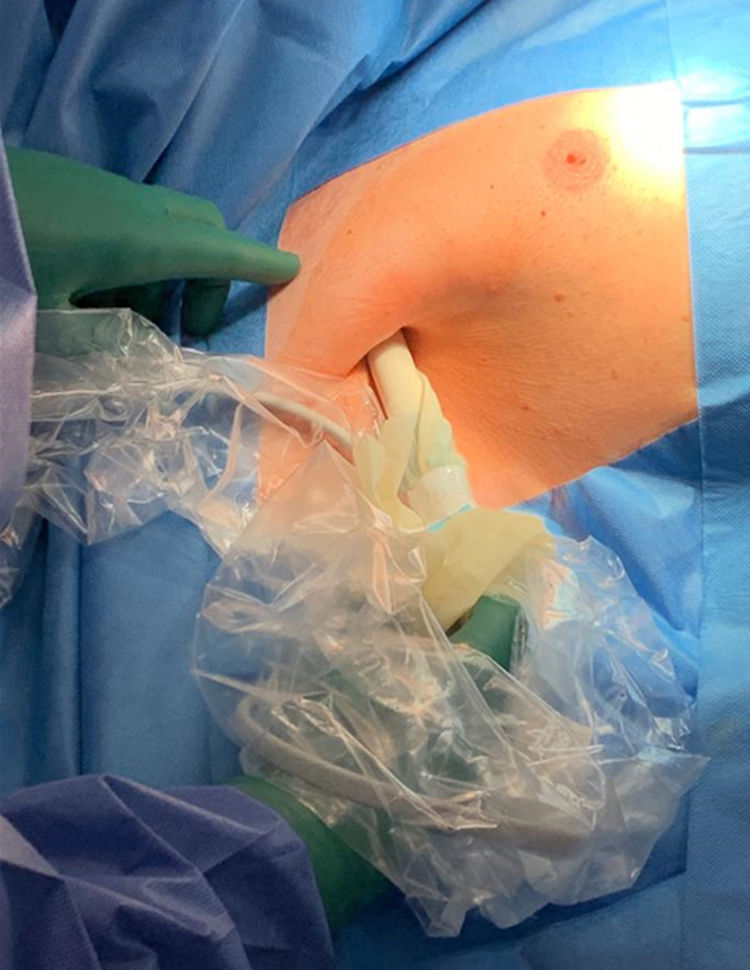
The patient is a 68-year-old man who had undergone surgery 8 years earlier for left CRC, stage IIB, which was treated with left hemicolectomy and adjuvant chemotherapy. Four years later, he presented liver recurrence, and segmentectomy of segment VI was performed. In subsequent check-ups, an interpectoral lymph node metastasis was diagnosed on the right side. Given that it was a solitary lesion, we decided to resect it, and the use of a marking method was proposed due to its size (<1cm) and anatomical location. We inserted a magnetic seed in the lymph node, which was done percutaneously under ultrasound guidance prior to surgery (Fig. 1). The procedure began with a 3cm right axillary incision through which the Sentimag®/Sienna+® probe was inserted. The lesion was detected between the pectoralis major and minor (Fig. 2) and was resected. The histological study confirmed the CRC lymph node metastasis. The patient is disease free after 5 months of follow-up.
Due to the advances made in detection techniques, tumors and recurrences are being diagnosed earlier. In many cases, the lesions are small or non-palpable, making it difficult to locate them in the surgical field.4 In recent years, new techniques have been developed for the localization of these tumors, such as ferromagnetic markers. The use of these techniques originated in non-palpable breast lesions. Historically, surgeons relied on non-invasive, but imprecise techniques, such as marking the skin with ink. Later, due to the increase in non-palpable lesions, wires were used as a localization technique. However, wire localization has some limitations: patients must carry the metal wire until the procedure, which may move, and involvement of the margins has been reported between 14% and 47%.5
In recent years, alternatives to wire localization have been developed for non-palpable breast tumors, such as radiopharmaceutical marking (125I seeds, albumin labeled with Tc99) for intraoperative gamma camera localization of the lesion,6 and more recently, the use of non-radioactive ferromagnetic seeds as markers in radio-guided surgery.7 These markers are composed of superparamagnetic iron oxide particles (SPIO) that are detected intraoperatively by the Sentimag®/Sienna+® probe used by the surgeon in the operating room. Numerous advantages have been reported about the use of ferromagnetic seeds compared to radioactive markers or wire localization. First of all, they can be used in hospitals that do not have nuclear medicine services, requiring fewer legal requirements than radioactive materials.8 Second, less margin involvement has been described compared to marking with a wire, allowing for more precise and smaller excisions, and reducing the number of reoperations. Another advantage is that they can be placed in the lesion weeks or even months before surgery, enabling patients to undergo neoadjuvant treatments with chemotherapy, if necessary, before surgery. Lastly, less healthy tissue must be removed because the lesion is accessed through more appropriate routes.9 In a retrospective study of 188 patients with 213 breast lesions, 100% localization of the lesions was reported at the time of excision, and 96.7% of the markers were placed within a radius of 1cm from the lesion.10
Although it is true that magnetic markers were originally developed for non-palpable breast cancer lesions, their use as a locator is being contemplated in other lesions, both malignant and benign.3 In the case we report, the patient had a CRC lymph node metastasis smaller than 1cm, and its deep location could have been an impediment for intraoperative identification. The use of the seed placed prior to surgery under ultrasound guidance facilitated excision and optimized surgical time as well as the approach, locating the lesion easily.
The use of magnetic seeds opens a wide range of possibilities beyond breast cancer lesions, which should be explored for the benefit of the patient and the improvement of the surgical technique of the surgeon.
Please cite this article as: Marín C, Piñero A, Marín P, Galindo P, Guzmán F. Uso de marcador ferromagnético para la detección intraoperatoria de metástasis ganglionar interpectoral de cáncer colorrectal. Cir Esp. 2020;98:632–634.