Hospital readmission is used as a measure of quality healthcare. The aim of this study was to determine the incidence, causes, and risk factors related to emergency consultations and readmissions within 30 and 90 days in patients undergoing laparoscopic gastric bypass and laparoscopic sleeve gastrectomy.
MethodsRetrospective study of 429 patients operated on from January 2004 to July 2015 from a prospectively maintained database and electronic medical records. Demographic data, type of intervention, postoperative complications, length of hospital stay and records of emergency visits and readmissions were analyzed.
ResultsWithin the first 90 days postoperative, a total of 117 (27%) patients consulted the Emergency Department and 24 (6%) were readmitted. The most common reasons for emergency consultation were noninfectious problems related to the surgical wound (n=40, 34%) and abdominal pain (n=28, 24%), which was also the first cause of readmission (n=9, 37%). Postoperative complications, reintervention, associated surgery in the same operation and depression were risk factors for emergency consultation within the first 90 days of the postoperative period.
ConclusionsDespite the high number of patients who visit the Emergency Department in the first 90 days of the postoperative period, few require readmission and none surgical reoperation. It is important to know the reasons for emergency consultation to establish preventive measures and improve the quality of care.
Los reingresos son un indicador de calidad de la cirugía. El objetivo del estudio fue determinar la incidencia, las causas y los factores de riesgo relacionados con las consultas a Urgencias y los reingresos a 30 y 90 días en pacientes sometidos a bypass gástrico laparoscópico y gastrectomía vertical laparoscópica.
MétodosEstudio retrospectivo de 429 pacientes intervenidos desde enero de 2004 a julio de 2015 a partir de una base de datos prospectiva y de las historias clínicas electrónicas. Se analizaron datos demográficos, el tipo de intervención, las complicaciones postoperatorias, la duración de la estancia hospitalaria y el registro de las visitas a Urgencias y los reingresos durante el periodo de estudio.
ResultadosEn los primeros 90 días del postoperatorio, un total de 117 (27%) pacientes consultaron a Urgencias y 24 (6%) reingresaron. Los motivos más frecuentes de consulta a Urgencias fueron los problemas no infecciosos relacionados con la herida quirúrgica (n = 40, 34%) y el dolor abdominal (n = 28, 24%), que además fue la primera causa de reingreso (n = 9, 37%). Las complicaciones postoperatorias, la reintervención, una cirugía asociada en el mismo acto quirúrgico y la depresión fueron factores de riesgo para consultar a Urgencias en los primeros 90 días del periodo postoperatorio.
ConclusionesA pesar del elevado número de pacientes que consulta a Urgencias en los primeros 90 días del periodo postoperatorio, pocos precisan reingreso y ninguno reintervención quirúrgica. Es importante conocer los motivos de las consultas a Urgencias para establecer medidas preventivas y mejorar la calidad asistencial.
Morbid obesity is a chronic disease and a well-known public health problem, with a prevalence of 1.2% of the adult population of Spain (ENRICA study, 2011), a rate that tends to double every 5–10 years.1 The treatment of choice is surgery, which is the only procedure that has been proven to be effective in the long term in terms of weight loss and resolution of comorbidities.2 Therefore, each year the number of surgical interventions increases3 and, consequently, so does the absolute number of complications.
Occasionally, complications arise when the patient has already been discharged and may go unnoticed. Meanwhile, studies conducted in the USA have determined that re-admission after bariatric surgery increases the procedure costs from $27000 to $65000.4 In recent years, several studies have analyzed the frequency and reasons for re-admission.5,6 According to these studies, approximately 56% of all Emergency Room visits are potentially avoidable and, more specifically, 75% of patients undergoing bariatric surgery who come to the Emergency Department do not require hospitalization. Currently, there are few studies in the literature that analyze the causes of ER visits that do not result in admission but increase hospital costs nevertheless. Most of these studies are carried out in private medical centers,7,8 and practically no studies have been carried out in a setting similar to ours, where the public health system is the norm and a greater influx of patients to the Emergency Department is predictable. The aim of our study was to determine the frequency and causes of emergency room visits and re-admissions within 30 and 90 days of patients treated with bariatric surgery, and to analyze associated factors and risk factors for emergency room visits.
MethodsWe conducted a retrospective study based on a perspective database and the electronic medical files of all the patients who had consecutively undergone bariatric surgery at the Hospital del Mar in Barcelona between January 2004 and July 2015. All patients were operated on by the same surgical team, and the procedures performed were Roux-en-Y gastric bypass or laparoscopic sleeve gastrectomy, using standardized techniques9 and in accordance with the National Institute of Health criteria from 1991.10 Clinical follow-up after the intervention followed the previously published protocol,9 which basically consisted of postoperative office visits one week post-op and then after one, 3, 6 and 12 months. Data were collected for demographic variables, comorbidities, type of procedure performed, associated surgeries during the same operation, postoperative complications classified according to Clavien-Dindo,11 hospital stay, visits to the ER within 30 and 90 days, re-admissions and treatments required.
An emergency visit was defined as a stay in the Emergency Department for less than 24h; a re-admission was a stay in the Emergency area for more than 24h and/or re-admission to any hospitalization unit. This study was approved by the Clinical Research Ethics Committee (Comité de Ética de Investigaciones Clínicas, CEIC) at the Institut Hospital del Mar d’Investigacions Mèdiques (IMIM).
Statistical AnalysisThe statistical analysis was performed using the SPSS® program (IBM Inc., Rochester, MN, USA). The association between demographic data, surgical procedure, comorbidities, in-hospital complications and visits to the Emergency Department was analyzed by means of a bivariate analysis, using the Fisher/Chi-squared test for categorical data and the Student's t test for continuous data. Subsequently, a multivariate analysis was applied to identify risk factors for ER consultation, expressing the results as odds ratio with 95% confidence intervals (CI). A P level <.005 was considered statistically significant.
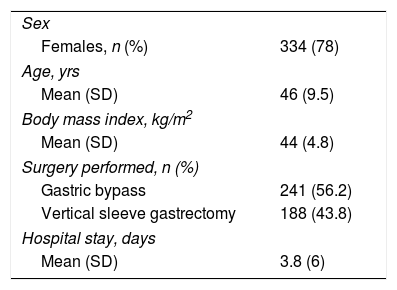
ResultsDuring the study period, 429 patients underwent bariatric surgery. Demographic and clinical data are shown in Table 1. A total of 136 ER visits were registered for 117 (27%) patients, with a mean of 1.2 visits per patient. Out of this group of patients, 24 (6%) were readmitted for the first 90 days after surgery.
Patient Demographic and Clinical Characteristics (No.=429) of the Study.
| Sex | |
| Females, n (%) | 334 (78) |
| Age, yrs | |
| Mean (SD) | 46 (9.5) |
| Body mass index, kg/m2 | |
| Mean (SD) | 44 (4.8) |
| Surgery performed, n (%) | |
| Gastric bypass | 241 (56.2) |
| Vertical sleeve gastrectomy | 188 (43.8) |
| Hospital stay, days | |
| Mean (SD) | 3.8 (6) |
SD: standard deviation.
Data are expressed as number and percentage in parentheses, except when indicated.
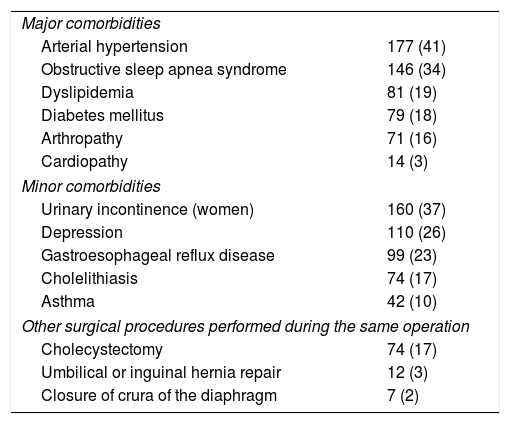
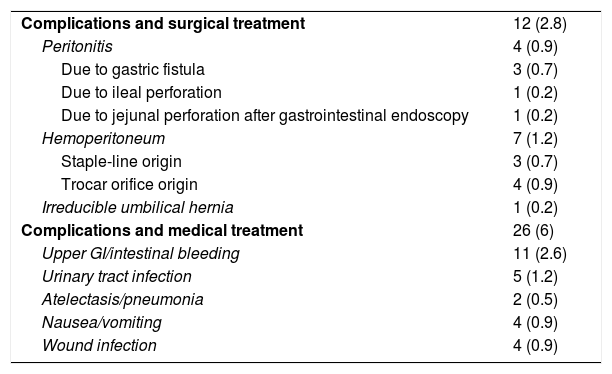
The comorbidities and associated surgeries of the patients in this series are shown in Table 2. There were a total of 38 (8.8%) postoperative complications: 2 grade I, 24 grade II and 12 grade IIIb, which are shown in Table 3.
Comorbidities and Associated Surgeries in the Study Population (No.=429).
| Major comorbidities | |
| Arterial hypertension | 177 (41) |
| Obstructive sleep apnea syndrome | 146 (34) |
| Dyslipidemia | 81 (19) |
| Diabetes mellitus | 79 (18) |
| Arthropathy | 71 (16) |
| Cardiopathy | 14 (3) |
| Minor comorbidities | |
| Urinary incontinence (women) | 160 (37) |
| Depression | 110 (26) |
| Gastroesophageal reflux disease | 99 (23) |
| Cholelithiasis | 74 (17) |
| Asthma | 42 (10) |
| Other surgical procedures performed during the same operation | |
| Cholecystectomy | 74 (17) |
| Umbilical or inguinal hernia repair | 12 (3) |
| Closure of crura of the diaphragm | 7 (2) |
Data are presented as number and percentage in parentheses.
Intra and Postoperative Complications Before Hospital Discharge (No.=38) and Causes.
| Complications and surgical treatment | 12 (2.8) |
| Peritonitis | 4 (0.9) |
| Due to gastric fistula | 3 (0.7) |
| Due to ileal perforation | 1 (0.2) |
| Due to jejunal perforation after gastrointestinal endoscopy | 1 (0.2) |
| Hemoperitoneum | 7 (1.2) |
| Staple-line origin | 3 (0.7) |
| Trocar orifice origin | 4 (0.9) |
| Irreducible umbilical hernia | 1 (0.2) |
| Complications and medical treatment | 26 (6) |
| Upper GI/intestinal bleeding | 11 (2.6) |
| Urinary tract infection | 5 (1.2) |
| Atelectasis/pneumonia | 2 (0.5) |
| Nausea/vomiting | 4 (0.9) |
| Wound infection | 4 (0.9) |
Data are presented as number and percentage in parentheses.
Within the first 90 days of the postoperative period, 117 (27%) patients came to the ER, 76 (65%) within the first 30 days and 41 (35%) between days 30 and 90. Out of these 117 patients, 24 (6%) required hospital readmission, 16 (67%) within the first 30 days and 8 (33%) between days 30 and 90 of the postoperative period.
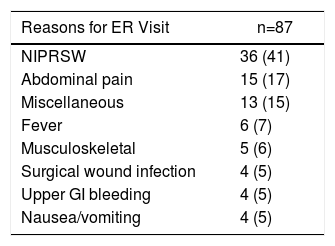
30 DaysThe 76 patients who visited the ER during the first 30 days of the postoperative period made a total of 87 visits, with an average of 1.2 visits per patient. The most frequent reasons were non-infectious surgical wound-related problems (n=36, 41%), abdominal pain (n=15, 17%) and fever (n=6, 7%), and 90% of these visits occurred in the first 15 days after the patient was discharged from hospital. As for readmissions during this period, out of the 16 patients who re-admitted, 7 (44%) complained of abdominal pain, 6 (37%) due to fever, 2 (12%) due to gastrointestinal bleeding and 1 (6%) due to infection of the surgical wound (Table 4).
Reasons for ER Visit and Readmission During the First 30 Days.
| Reasons for ER Visit | n=87 |
|---|---|
| NIPRSW | 36 (41) |
| Abdominal pain | 15 (17) |
| Miscellaneous | 13 (15) |
| Fever | 6 (7) |
| Musculoskeletal | 5 (6) |
| Surgical wound infection | 4 (5) |
| Upper GI bleeding | 4 (5) |
| Nausea/vomiting | 4 (5) |
| Reasons for Readmission | n=16 |
|---|---|
| Abdominal pain | 7 (44) |
| Fever | 6 (38) |
| Upper GI bleeding | 2 (12) |
| Infection of the surgical wound | 1 (6) |
NIPRSW: non-infectious problems related with the surgical wound.
Data are presented as number and percentage in parentheses.
It should be noted that 100% of the patients who came to the ER with fever were readmitted, as were 7 of the 15 (47%) who reported abdominal pain. None of these patients required surgery.
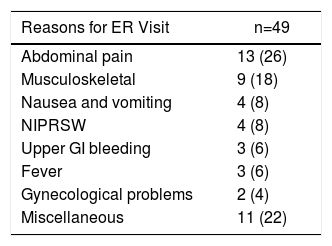
Between 30 and 90 DaysDuring this period, 41 (10%) patients visited the Emergency Department a total of 49 times, with an average of 1.2 visits per patient. The most frequent reason was abdominal pain (n=13, 26%), followed by musculoskeletal pain (n=9, 18%), and nausea and vomiting (n=4, 8%). In this group, 8 (20%) patients required readmission: 2 (25%) due to abdominal pain, 2 (25%) due to fever, 2 (25%) due to gastrointestinal bleeding and 2 (25%) due to nausea and vomiting. Surgical reoperation was also not required by any of the patients in this period (Table 5).
Reasons for ER Visit and Readmission in the 30- to 90-day Period.
| Reasons for ER Visit | n=49 |
|---|---|
| Abdominal pain | 13 (26) |
| Musculoskeletal | 9 (18) |
| Nausea and vomiting | 4 (8) |
| NIPRSW | 4 (8) |
| Upper GI bleeding | 3 (6) |
| Fever | 3 (6) |
| Gynecological problems | 2 (4) |
| Miscellaneous | 11 (22) |
| Reasons for Readmission | n=8 |
|---|---|
| Abdominal pain | 2 (25) |
| Fever | 2 (25) |
| Upper GI bleeding | 2 (25) |
| Nausea and vomiting | 2 (25) |
NIPRSW: non-infectious problems related with the surgical wound.
Data are presented as number and percentage in parentheses.
The analyzed factors were: age, sex, body mass index, arterial hypertension, diabetes mellitus, obstructive sleep apnea, osteoarthritis, associated surgery in the same operation, depression, surgical reintervention, surgical technique used, days of hospital stay and postoperative complication.
The bivariate analysis analyzed factors associated with visits to the ER within the first 30 days: the performance of gastric bypass (P=.03), hospital stay≥4 days (P=.01) and the presence of postoperative complications (P<.005). Between 30 and 90 days, factors were: the performance of an associated surgical procedure (P<.005), depression (P=.008) and reoperation (P<.005). In the multivariate analysis, the only risk factor related to the emergency visit during the first 30 days post-op was postoperative complications (OR 2.383, 95% CI 1.242–4.571), while during the 30–90 day period it was reoperation (OR 4.565, 95% CI 1.410–14.779), depression (OR 2.263, 95% CI 1.142–4.485) and the performance of associated surgery (OR 2.562, 95% CI 1.267–5.183).
DiscussionIn our study, 27% of the patients who were treated with bariatric surgery came to the Emergency Department within the first 90 days of the postoperative period, and most of these (65%) within the first 30 days. In spite of the elevated number of patients who visited the ER, only 6% were readmitted and none required reoperation.
Regarding the percentage of Emergency Room visits, our data are higher than those obtained by other groups in similar studies, where the percentage of visits varies from 11% to 18%.7,8,12 Macht et al.8 analyzed 36673 patients who underwent bariatric surgery and reported 14.6% ER visits in the first 90 days, and 52% of these in the first 30 days.8 Telem et al.,12 on the other hand, obtained 11.3%, and Mora-Pinzon et al.7 reported 10.7% within 30 days. This disparity of results could be explained by 2 factors. On the one hand, the 3 studies have included patients with private medical coverage (up to 58% in the case of Mora-Pinzon et al.7), which may reduce the number of ER visits in the case of minor complications.13,14 On the other hand, there are differences in the definition of ER visits, as Mora-Pinzon et al.,7 for instance, did not include patients requiring readmission.
In our study, 100% of patients came from the public healthcare system. In addition, the patients who underwent the surgical procedure at our hospital, for organizational reasons, reside in the surrounding area, which may favor visits to the Emergency Department for minor reasons. Regarding the reasons for visiting the ER, the most frequent in the first 90 days were non-infectious problems related to surgical wounds, which represent one-third of visits, especially in the first 30 days. The second reason in order of frequency was abdominal pain (24% of the total in the first 90 days), which was the most frequent in the 30–90 day period. These data are similar to those obtained by the previously mentioned studies. In the case of Macht et al.,8 the most common reason for the visit was abdominal pain (24.4%), followed by nausea and vomiting (20.8%), although other reasons are not reported. In the case of Chen et al.,14 the most frequent reasons were nausea and vomiting (17.5%), abdominal pain (13.2%) and problems with surgical wounds (10.9); they also documented that up to 88% of the total visits for these reasons were preventable. In our case, we have not analyzed how many of the emergency visits that occurred in the period analyzed were preventable, but we do know the percentage of readmission for the main reasons for consultation, which was 0% in the case of non-infectious wound-related problems and 32% in the case of abdominal pain.
With regards to risk factors for visiting the Emergency Department during the first 90 days of the postoperative period, there is a disparity of results between the different studies. In our case, postoperative complications, reoperation, depression and associated surgical procedure during the same operation were risk factors for the emergency visit. In other studies, such as that by Macht et al.,8 the risk factors detected were: age (young), sex (female), ≥4 comorbidities, ≥2 previous visits to the Emergency Room, open surgery and prolonged postoperative stay8; however, due to characteristics of their database, factors such as postoperative complications or reoperation were not analyzed. In the study by Telem et al.,12 the following risk factors were identified: the type of medical insurance (greater risk if the insurance was Medicare) and the distance from the hospital to the home (higher risk at greater proximity); these factors were not analyzed in our study but, as already mentioned, could explain our higher percentage of visits to the Emergency Department.
Based on our results, we believe that it is essential to transmit at the time of discharge, both orally and in writing, detailed information about the possible signs and symptoms that the patient may present, including instructions on how to determine whether they should go to the Emergency Department, or provide them with a direct telephone contact. In conclusion, emergency room visits in our setting are frequent, especially during the first 30 days, although the number of patients requiring re-admission is small. Once the associated and risk factors have been identified, preventive measures can be established to reduce the number of visits.
Authors’ ContributionMaría P. Iskra and José M. Ramón: study design, data collection, analysis and interpretation of the results, article composition, critical review and approval of the final version.
Andrés Martínez-Serrano: study design, data collection, analysis and interpretation of the results and approval of the final version.
Manuel Pera and Luis Grande: analysis and interpretation of the results, critical review and approval of the final version.
Albert Goday, Carmen Serra, Enrique Lanzarini and Lourdes Trillo: data collection, interpretation of the results and approval of the final version.
Conflict of InterestThe authors have no conflict of interests to declare.
Please cite this article as: Iskra MP, Ramón JM, Martínez-Serrano A, Serra C, Goday A, Trillo L, et al. Consultas a Urgencias y reingresos a 30 y 90 días tras cirugía bariátrica. Cir Esp. 2018;96:221–225.