The liver is the most frequently injured organ in blunt abdominal trauma. Patients who are hemodynamically unstable must undergo immediate surgical treatment. There are 2 surgical approaches for these patients: Anatomical Liver resection and non-anatomic liver resection. Around 80%–90% of patients are candidates for non-operative management. Several risk factors have been studied to select the patients most suited for a non-operative management.
Materials and methodsWe performed a retrospective study based on a prospective database. We searched for risk factors related to immediate surgical management and failed non-operative management. We also described the surgical procedures that were undertaken in this cohort of patients and their outcomes and complications.
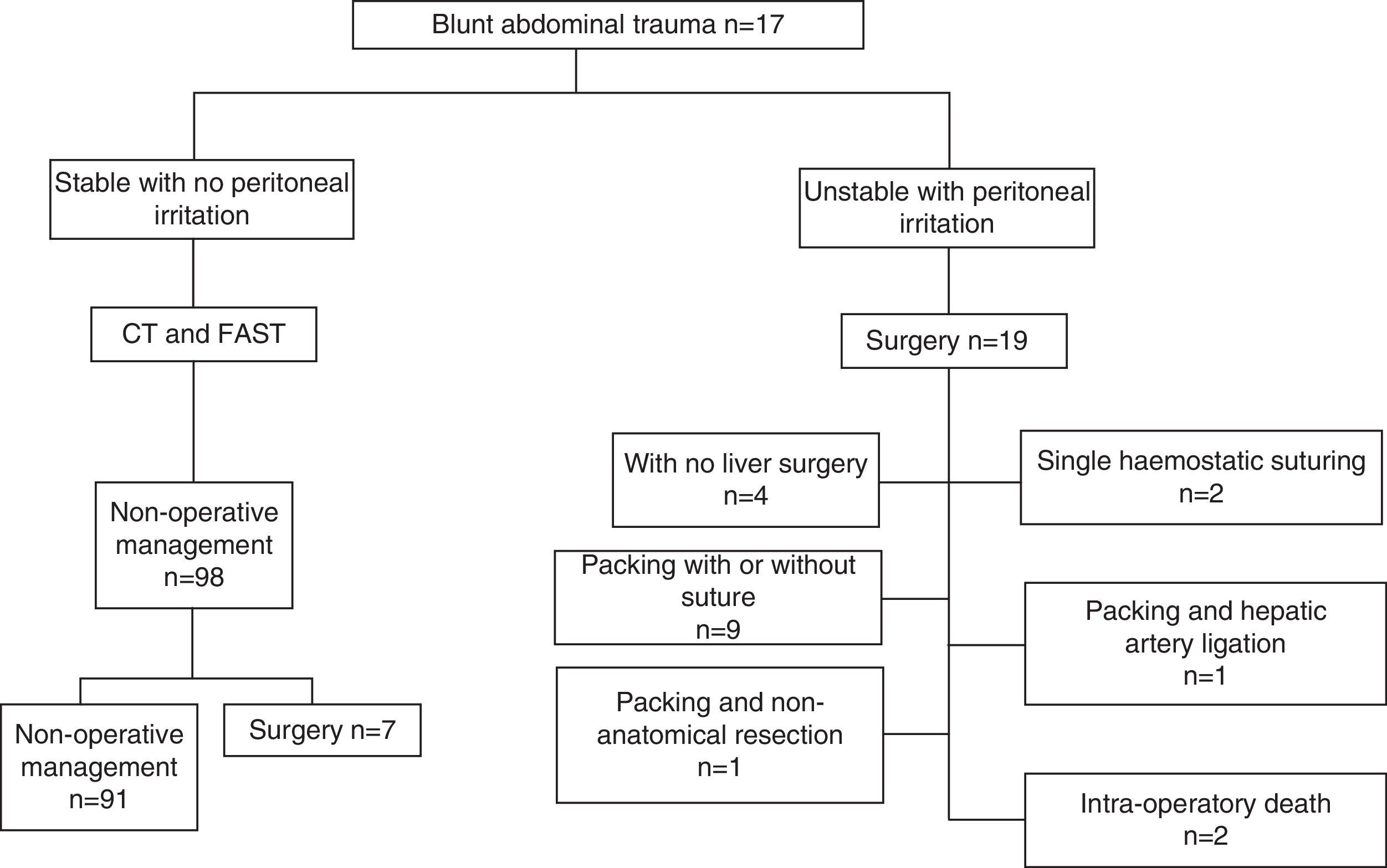
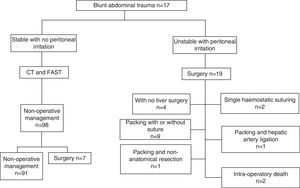
ResultsDuring the study period 117 patients presented with blunt liver trauma. 19 patients (16.2%) required a laparotomy during the initial 24h after their admission. There were eleven deaths (58%) amongst these patients. Peri-hepatic packing and suturing were the most common procedures performed. An RTS Score<7.8 (RR: 7.3; IC 95%: 1.8–30.1), and ISS Score >20 (RR 2,5 IC 95%: 1.0–6.7), and associated intra-abdominal injuries (RR: 2.95; IC 95%: 1.25–6.92) were risk factors for immediate surgery. In 98 (83.7%) patients a non-operative management was performed. 7 patients had a failed non-operative management.
ConclusionThe need for immediate surgical management is related to the presence of associated intra-abdominal injuries, and the ISS and RTS scores. In this series the most frequently performed procedure for blunt liver trauma was peri-hepatic packing.
El hígado es el órgano que se afecta más frecuentemente en el traumatismo cerrado de abdomen. Los pacientes que ingresan con inestabilidad hemodinámica deben ser intervenidos de inmediato. Existen 2 posturas en la literatura como aproximación quirúrgica: la resección anatómica y la resección no anatómica. El 80–90% de los pacientes son susceptibles de manejo no operatorio. Se han explorado diferentes factores de riesgo para seleccionar los pacientes candidatos a manejo no operatorio del traumatismo hepático.
Materiales y métodosEstudio retrospectivo a partir de una base de datos prospectiva. Exploramos los factores de riesgo relacionados con la indicación de cirugía inmediata y el fallo del manejo no operatorio. Se describen los procedimientos quirúrgicos realizados y sus desenlaces.
ResultadosSe presentaron 117 pacientes con traumatismo cerrado de hígado. Diecinueve pacientes (16,2%) de los admitidos con traumatismo cerrado de hígado requirieron laparotomía inmediata en las primeras 24h siguientes al ingreso en la institución. Hubo 11 muertes en este grupo (58%). El procedimiento quirúrgico más practicado fue sutura y empaquetamiento. Fueron factores de riesgo para requerir cirugía inmediata tener un RTS menor de 7,8 (RR: 7,3; IC 95%: 1,8–30,1), ISS mayor de 20 (RR: 2,5; IC 95%: 1,0–6,7) y la presencia de lesiones intraabdominales asociadas (RR: 2,95; IC 95%: 1,25–6,92). En 98 (83,7%) pacientes se optó por el manejo no operatorio. En 7 hubo fallo del manejo no operatorio.
ConclusiónLa necesidad de cirugía inmediata está directamente relacionada con la puntuación RTS, ISS y la presencia de lesiones intraabdominales asociadas. En esta serie el procedimiento quirúrgico más frecuentemente realizado fue el empaquetamiento perihepático.
The liver is the most frequently injured organ after open and blunt abdominal trauma.1 Until two decades ago peritoneal lavage was used to make a diagnosis and patients were regularly subjected to surgery without the extent of the trauma being known; the surgical procedure was often unecessary.2 Since then with the advent of computerised tomography, it has been possible to classify the extent of liver injury more accurately and the safety of the selective, non-operative management of patients with blunt trauma and even of some patients with penetrating liver trauma who are haemodynamically stable has been demonstrated.3,4 However, there are a number of patients who, due to the severity of their liver injury or because they have associated intra-abdominal injuries, do require operative management, and there are different surgical techniques which can be used. The decision as to which technique to use is controversial and it is often down to the attending surgeon to decide according to their experience and preference. Techniques include simple surgical suturing, anatomical and non-anatomical resection, packing and even liver transplant.1,5
We have reported earlier our experience with the non-operative management of liver trauma before6; this is the follow-up of the previous study with a special focus on the techniques used for managing patients who required surgery. The best surgical option is to preserve the parenchyma, however in the current literature there are two different opinions for patients requiring a hepatic resection; anatomical resection7 and non-anatomical resection.2,3,5
The aim of this study is to explore, in a cohort of patients with blunt liver trauma treated at a reference hospital, the risk factors which require operative management in the first 24h following admission, the risk factors for failure of non-operative management and to describe the surgical techniques used in the operated patients and their results.
Materials and MethodsA retrospective study was undertaken using a prospective database, from January 2005 to December 2011. Patients over the age of 15 were included with blunt abdominal trauma, admitted to the Emergency Department of the University Hospital San Vicente Fundación de Medellín, Colombia, a reference centre for trauma, where liver injury was confirmed by computerised tomography (CT) or intra-operative findings. Patients with trauma evolution of more than 24h, those who had been operated in a different hospital and those who did not wish to participate in the study were excluded.
Included in the study were: demographic variables, age, gender, history of abdominal surgery and the trauma mechanism, trauma severity indices, Revised Trauma Score (RTS), Injury Severity Score (ISS) and the use of abdominal ultrasound for trauma (FAST). The liver injury was classified using the organ injury scale (OIS) of the American Association for the Surgery of Trauma (AAST).8 The extent of injury in patients who were managed non-operatively was determined by CT. The extent of injury in patients who were managed operatively was established from the operation description.
The patients were attended according to Advanced Trauma Life Support (ATLS) guidelines. Resuscitation with crystalloids was initiated and if the patient remained haemodynamically unstable after that (SBP lower than 90mmHg with no response to resuscitation), it was the decision of the surgeon whether to undertake emergency surgery. In this case the patient entered the study under emergency operative management.
Patients with a good response to established resuscitation measures underwent an abdominal CT and non-operative management was started; in cases showing extravasation of the contrast, embolisation by interventional radiology was considered. If the patient became unstable or presented signs of peritoneal irritation, it was considered a failure of the non-operative treatment and an exploratory laparotomy was performed.
We explored the risk factors associated with the indication for emergency surgery and the failure of non-operative management was defined as the requirement for surgery after 24h stay in hospital. We described the surgical procedures undertaken and complications whether or not they were associated with the liver trauma.
The surgical approach route used was midline incision; then the liver was mobilised sectioning the falciform and lateral triangular ligaments (if necessary). The decision as to the type of surgery was made by the surgeon depending on the intra-operative findings (extent of injury).
The study was approved by the hospital's research and ethics committees.
Statistical AnalysisThe analysis included a descriptive phase and an analytical phase. The qualitative variables were studied in the descriptive phase and their frequencies presented. The means, standard deviation, medians and ranges of the quantitative variables were presented. A bivariate analysis was undertaken in the analytical phase which explored the risk factors associated with the outcomes of interest: indication for emergency surgery and failure of non-operative management by calculating the relative risk (RR) and the Chi square and Fisher test of independence. The statistical programme SPSS, version 18.0, was used for the analysis.
Results117 patients with blunt liver trauma presented during the period between January 2005 and December 2011; 90 men and 27 women. The average age was 32.3±14.58 (15–80).
The most common trauma mechanisms were traffic accidents involving the driver of the vehicle in 53 cases (45.3%) and 35 cases were pedestrian accidents (29.9%). The median value of the patient's RTS on admission was 7.55 (range: 2.62–7.84) and of the ISS 22.0 (range: 2.0–7.55). Seven patients (6.0%) had a history of previous abdominal surgery.
Extra-abdominal injuries associated with blunt liver trauma were craneoencephalic trauma in 41 patients (35%). There were 12 patients with spinal cord trauma (10.2%) and 19 with pelvic fractures (16.2%).
Emergency Surgical TreatmentNineteen patients (16.2%) of those admitted with blunt liver trauma required emergency laparotomy within the first 24h following admission to hospital. In all cases haemodynamic instability was an indication for surgery: 17 due to severe haemorrhage (13 cases secondary to liver trauma, three cases due to splenic bleeding and one due to liver and splenic bleeding) and two as a result of serious hollow visceral injury.
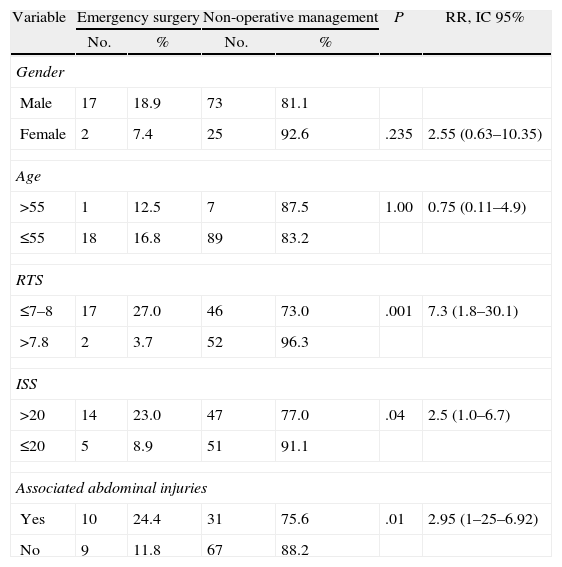
Some predictors of the need to undertake emergency operative management were explored (Table 1). A RTS lower than 7.8 (RR: 7.3; 95% CI: 1.8–30.1), ISS above 20 (RR: 2.5; 95% CI: 1.0–6.7) and the presence of associated intra-abdominal injuries (RR: 2.95; 95% CI: 1.25–6.92) were risk factors requiring emergency surgery for blunt liver trauma.
Bivariated Data for Predictor Factors of Emergency Operative Management.
| Variable | Emergency surgery | Non-operative management | P | RR, IC 95% | ||
| No. | % | No. | % | |||
| Gender | ||||||
| Male | 17 | 18.9 | 73 | 81.1 | ||
| Female | 2 | 7.4 | 25 | 92.6 | .235 | 2.55 (0.63–10.35) |
| Age | ||||||
| >55 | 1 | 12.5 | 7 | 87.5 | 1.00 | 0.75 (0.11–4.9) |
| ≤55 | 18 | 16.8 | 89 | 83.2 | ||
| RTS | ||||||
| ≤7–8 | 17 | 27.0 | 46 | 73.0 | .001 | 7.3 (1.8–30.1) |
| >7.8 | 2 | 3.7 | 52 | 96.3 | ||
| ISS | ||||||
| >20 | 14 | 23.0 | 47 | 77.0 | .04 | 2.5 (1.0–6.7) |
| ≤20 | 5 | 8.9 | 51 | 91.1 | ||
| Associated abdominal injuries | ||||||
| Yes | 10 | 24.4 | 31 | 75.6 | .01 | 2.95 (1–25–6.92) |
| No | 9 | 11.8 | 67 | 88.2 | ||
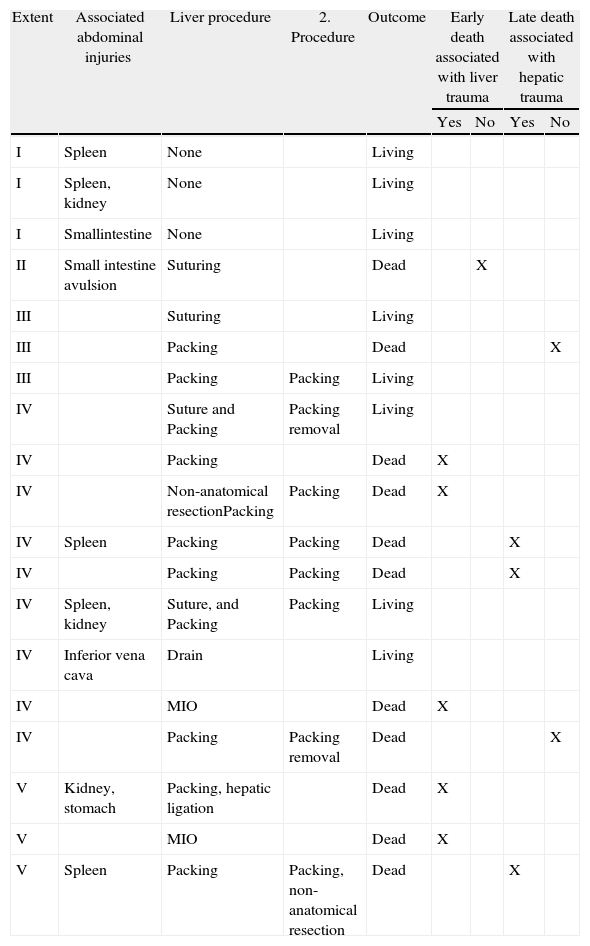
There were eleven deaths in this group (57.9%), six were perioperative, five associated with the severity of the liver trauma and one secondary to intestinal avulsion. There were five late deaths, three of which were associated with the liver trauma and the other two secondary to craneoencephalic trauma (Table 2).
Surgical Treatment of Liver Injury in Patients Undergoing Emergency Surgery According to Extent of Injury and Outcome.
| Extent | Associated abdominal injuries | Liver procedure | 2. Procedure | Outcome | Early death associated with liver trauma | Late death associated with hepatic trauma | ||
| Yes | No | Yes | No | |||||
| I | Spleen | None | Living | |||||
| I | Spleen, kidney | None | Living | |||||
| I | Smallintestine | None | Living | |||||
| II | Small intestine avulsion | Suturing | Dead | X | ||||
| III | Suturing | Living | ||||||
| III | Packing | Dead | X | |||||
| III | Packing | Packing | Living | |||||
| IV | Suture and Packing | Packing removal | Living | |||||
| IV | Packing | Dead | X | |||||
| IV | Non-anatomical resectionPacking | Packing | Dead | X | ||||
| IV | Spleen | Packing | Packing | Dead | X | |||
| IV | Packing | Packing | Dead | X | ||||
| IV | Spleen, kidney | Suture, and Packing | Packing | Living | ||||
| IV | Inferior vena cava | Drain | Living | |||||
| IV | MIO | Dead | X | |||||
| IV | Packing | Packing removal | Dead | X | ||||
| V | Kidney, stomach | Packing, hepatic ligation | Dead | X | ||||
| V | MIO | Dead | X | |||||
| V | Spleen | Packing | Packing, non-anatomical resection | Dead | X | |||
In this group of patients ten (52.6%) had liver trauma alone and nine (47.4%) had associated injuries (Table 2).
The surgical procedures performed on this group of patients are described in Table 2. Six patients required liver packing in a second operation for persistent bleeding; four of these patients died. Non-anatomical liver resections were performed on only two patients, one in the first procedure and the other in the reoperation; no anatomical resection was performed.
In the group of patients who underwent surgery on admission there were eleven complications (57.9%), three cases of peritonitis (27.3%), three intra-abdominal abscesses (27.3%), two cases of bleeding (18.2%), one empyema, one case of pancreatitis and one enteroatmospheric fistula.
Non-operative ManagementNon-operative management was selected for 98 (83.7%) of 117 patients with blunt liver trauma. Two patients required selective embolisation of the branches of the hepatic artery where there was active bleeding, with successful results.
Of the group of patients who were not managed surgically, 31 (31.6%) had one or more injured intra-abdominal organs: eleven (35.5%) had trauma to the spleen, eighteen (58.1%) trauma to the kidney and two (6.5%) trauma to the pancreas.
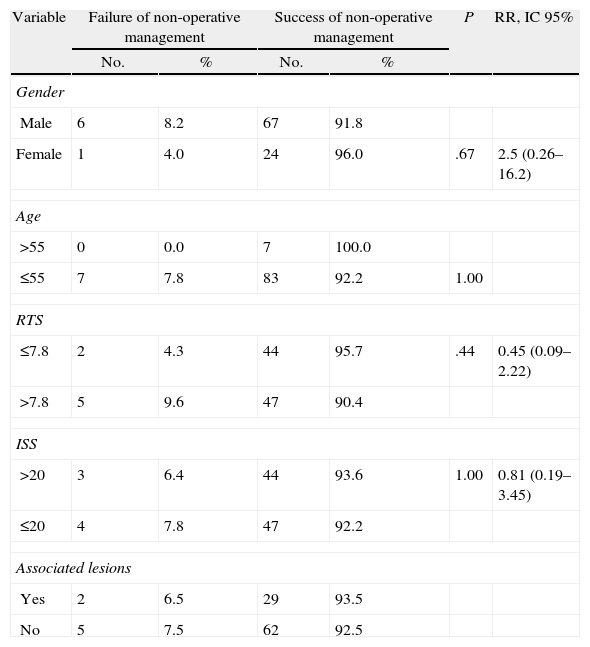
Non-operative management failed in seven (7.1%) patients. The relationship of some variables which might have been associated with the failure of non-operative management was examined (gender, age, ISS, RTS, presence of intra-abdominal organ injury, extent of liver injury). None of the factors studied was a risk factor for the failure of non-operative management (Table 3).
Bivariated Analysis of Predictor Factors of Failure of Non-operative Management.
| Variable | Failure of non-operative management | Success of non-operative management | P | RR, IC 95% | ||
| No. | % | No. | % | |||
| Gender | ||||||
| Male | 6 | 8.2 | 67 | 91.8 | ||
| Female | 1 | 4.0 | 24 | 96.0 | .67 | 2.5 (0.26–16.2) |
| Age | ||||||
| >55 | 0 | 0.0 | 7 | 100.0 | ||
| ≤55 | 7 | 7.8 | 83 | 92.2 | 1.00 | |
| RTS | ||||||
| ≤7.8 | 2 | 4.3 | 44 | 95.7 | .44 | 0.45 (0.09–2.22) |
| >7.8 | 5 | 9.6 | 47 | 90.4 | ||
| ISS | ||||||
| >20 | 3 | 6.4 | 44 | 93.6 | 1.00 | 0.81 (0.19–3.45) |
| ≤20 | 4 | 7.8 | 47 | 92.2 | ||
| Associated lesions | ||||||
| Yes | 2 | 6.5 | 29 | 93.5 | ||
| No | 5 | 7.5 | 62 | 92.5 | ||
The indication for surgery in two of these patients was associated with liver bleeding in the first 48h post trauma, who were treated with perihepatic packing; another two patients presented signs of peritoneal irritation due to bile peritonitis and in three cases the indications for surgery were associated injuries: one case of intraperitoneal bladder trauma, one case of pancreatic trauma and another case with trauma to the pancreas and kidney.
Ninety-one patients underwent successful non-operative treatment of their liver trauma. There were two late deaths in this group, one secondary to trauma to the thoracic aorta and the other due to associated craneoencephalic trauma.
Ten complications (11%) occurred in the 91 patients in whom non-operative treatment had been successful: three hepatic abscesses which required percutaneous drainage, one superinfected haematoma, one case of bleeding, two ventilator-related pneumonias, one endobronchitis and two cases of catheter-related bacteraemia.
The outcomes of the cohort are presented in Fig. 1.
DiscussionThe management of blunt liver trauma has changed drastically over recent decades and non-operative management is now accepted as standard.4,9,10 Advances in imaging studies have enabled the extent of liver trauma to be classified to such an extent that increasingly fewer non-therapeutic laparotomies need to be performed and thus there is a reduction in associated morbimortality.6,9–13 We have published a previous cohort on the non-operative management of liver trauma; this publication is an expansion of that previous cohort, but with the objective of determining the surgical strategy used and its results.
In addition to this, minimally invasive procedures, such as angioembolisation or percutaneous drainage of collections, have contributed towards the increased success rates of non-operative management.14 Nevertheless, there are a significant number of patients who need to undergo emergency surgery, principally due to haemodynamic instability secondary to severe haemorrhage or the presence of associated intra-abdominal injuries.6,15 In our study, nineteen patients (16.2%) required emergency surgery, the independent risk factors for this outcome were an RTS score below 7.8 (RR: 7.3; 95% CI: 1.8–30.1), ISS greater than 20 (RR: 2.5; 95% CI: 1.0–6.7) and the presence of associated intra-abdominal injuries (RR: 2.95; 95% CI: 1.25–6.92), which is to be expected given the complexity of the trauma. The cut-off point of the RTS score for indicating the risk of requiring emergency surgery should be interpreted as it not being necessary for the patients to be very seriously physiologically compromised for them to require operative treatment; this is probably also influenced by the size of the sample. 7.1% of the patients who underwent non-operative management required late surgery due to intra-abdominal complications, without finding significant risk factors in relation to this in the study. The 2% failure rate due to liver bleeding is comparable with published figures up to 3.5%.16
In our series, liver packing was performed in eleven out of nineteen patients (58%) who required emergency surgery and in two patients for whom non-operative treatment had failed, with a fatal outcome in eight out of eleven (72%) of the patients of the first group and none in the group of patients where non-operative treatment had failed. In the group of patients who underwent surgery, 42.3% of the deaths were directly associated with liver trauma, and all of them were patients with severe traumas (grade IV or V). The mortality for this extent of injury has remained high in reports in literature, varying from 46% to 80% in the most severe traumas and in most cases is secondary to uncontrollable bleeding.15,17–19
Perihepatic packing is a highly recommended method for the initial management of patients with severe liver trauma who require emergency operative management14,16,20–22 as it reduces blood loss, surgery time and mortality and makes appropriate resuscitation possible in the Intensive Care Unit.5,14 However, it is acknowledged in the literature that packing is not complication-free because if it is not correctly performed, the patient may require early reoperation or, if it is not removed after a suitable amount of time, there is an increased likelihood of complications of infection or rebleeding.16,20,23,24 The hospital protocol is to remove packing between 48 and 72h.
Liver resection has been criticised in the context of patients with severe liver trauma for its high morbimortality rates, however recent studies7 suggest that staff with specific training in hepatobiliary surgery can achieve greater success rates in this scenario. Non-anatomical resections are technically easier to perform than anatomical resections and seem to reduce the morbimortality associated with the septic and haemorrhagic complications linked with this procedure.18,25 The protocol of the University of Pittsburgh2 recommends as indications for hepatic resection: (a) hepatic venous injury; (b) massive destruction of liver tissue; and (c) biliary fistula of the main ducts. However if they are considered, this should be in selected patients and not necessarily in the first surgical intervention.5,16
Only two non-anatomical resections were performed in our group of patients and both died. The series of Polanco et al. published 216 patients with liver trauma, of whom 144 required operative management, the majority only procedures without resections and a third required hepatic resection.2 The difference in the percentage of resections comparing this study with our series could be attributable to the great difference in size of the sample.
Of the patients who required surgery on admission eleven of the nineteen (57.8%) presented complications; the most frequent was peritonitis in three out of eleven (27.3%), intra-peritoneal abscesses in three out of eleven (27.3%) and post-surgical bleeding in two out of eleven (18.2%). The percentage of complications of infection reported in the literature varies between 7% and 30%, however this increases to 44% if perihepatic packing had been performed.2,19,20,26 This is the most common situation in our series, being the most likely explanation for the high percentage of infectious complications.
In our experience there are no data establishing the benefit of performing anatomical or non-anatomical liver resections as part of the management of severe liver trauma. More studies are necessary to define the subgroups of patients who would benefit from this strategy and the time and conditions in which it should be implemented.
ConclusionIn conclusion, non-operative management of liver trauma in haemodynamically stable patients is the treatment of choice. The need for emergency surgery is directly linked to RTS and ISS scores and the presence of associated intra-abdominal injuries. The simplest procedure possible should be performed on these patients to control haemorrhage; in our series this was principally perihepatic packing. However, since it was used as a damage-control surgery strategy in seriously ill patients, the mortality of this procedure remains very high. In our experience, there are no data establishing the benefit of performing liver resections as the initial management of severe liver trauma.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Morales Uribe CH, Arenas López C, Correa Cote JC, Tobón Franco S, Saldarriaga MF, Mosquera J, et al. Tratamiento del traumatismo cerrado de hígado, indicaciones de cirugía y desenlaces. Cir Esp. 2014;92:23–29.