Bowel cancer is increasing in prevalence in geriatrics (older than 65 years). The influence of comorbidities on the post-surgical results of bowel cancer is not well known. Our aim was to assess the comorbidities using the Charlson index in a geriatric population subjected to bowel cancer surgery, and analyze their influence on the postoperative results and the mortality rate.
Material and methodsThe study included 115 patients (over 65 years old and with 5 years follow-up) subjected to bowel cancer surgery in the Vic General Hospital (Barcelona) between the years 2003 and 2005. Three comorbidity groups were established using the Charlson index: absent (0 points), low (1–2 points), and high (≥3 points). The postoperative medical and surgical complications, as well as mortality, were determined in each of the groups.
ResultsThe relative risk of a medical complication adjusted for age and stage was 2.7 (95% CI; 1.07–7) and 4.3 (95% CI; 1.3–14) times higher in the low and high comorbidity groups, respectively. There were no differences in post-surgical complications between the comorbidity groups. The length of hospital stay was higher in the in the high comorbidity group compared to the group with no comorbidity (17 days compared to 26 days, P=.02). The relative risk of mortality adjusted for age and stage was 1.7 (95% CI; 1.04–3) and 2.5 (95% CI; 1.3–4.6) in the low and high comorbidity groups, respectively.
ConclusionThe presence of any level of comorbidity measured by the Charlson index is an independent predictive factor of medical complications and of an increase in overall mortality in geriatric patients subjected to bowel cancer surgery.
La neoplasia de colon es cada vez más prevalente en la edad geriátrica (mayores de 65 años). La influencia de las comorbilidades en los resultados postquirúrgicos de la neoplasia de colon es poco conocida. Nuestro objetivo fue valorar las comorbilidades a través del índice de Charlson en una población geriátrica intervenida por neoplasia de colon, y estudiar su influencia en los resultados postoperatorios y la mortalidad.
Material y métodosSe incluyó a 115 pacientes intervenidos de neoplasia de colon en el Hospital General de Vic entre los años 2003 y 2005 con más de 65 años y 5 años de control evolutivo. Mediante el índice de comorbilidad de Charlson se establecieron 3 grupos de comorbilidad: ausencia (0 puntos), baja (1–2 puntos) y alta (≥ 3 puntos). Para cada uno de los grupos se determinaron complicaciones postoperatorias médicas, quirúrgicas y mortalidad.
ResultadosEl riesgo relativo de complicación médica ajustado por edad y estadio fue 2,7 (IC 1,07–7) y 4,3 (IC 1,3–14) veces superior en los grupos de baja y alta comorbilidad respectivamente. Las complicaciones quirúrgicas postoperatorias no fueron diferentes entre los grupos de comorbilidad. El tiempo de estancia hospitalaria fue mayor en el grupo de alta comorbilidad respecto al de nula comorbilidad (17 días respecto a 26, p=0,02). El riesgo relativo de mortalidad ajustado por edad y estadio fue de 1.7 (IC 1,04–3) y 2,5 (IC 1,3–4,6) en los grupos de baja y alta comorbilidad respectivamente.
ConclusiónLa presencia de algún grado de comorbilidad medida por el índice de Charlson es un factor predictor independiente de complicaciones médicas y de aumento de mortalidad global en pacientes geriátricos intervenidos por neoplasia de colon.
Colon cancer is one of the most prevalent types of cancer in the western world. Its incidence increases with age, and 70% of cases are diagnosed in senior citizens (those over the age of 65). The expected increase in the population age in coming years will likely bring about a significant rise in the number of senior patients with colorectal cancer.
One of the problems in neoplastic diseases diagnosed in senior citizens is the proper selection of candidates for treatment (which would be surgical in this case); there is a general tendency toward undertreatment. The main reason for this is the inherent association between older age and mortality, clearly supported by data from surgically treated colon neoplasms, where mortality increases nearly three-fold in patients older than 65–70.1 Another reason is a lack of proper scientific evidence because studies do not usually include patients from all age groups within the geriatric spectrum, and subjects from older age groups are often not included. According to one study,2 undertreatment may objectively result in 30%–50% less surgical interventions, chemotherapy or radiotherapy in geriatric patients.
We therefore asked ourselves if age should be an absolute value to limit surgical treatment in colon cancer, or whether we should take into account other variables for selecting ideal patients for treatment within the senior age range. We believe that comorbidity could be one of these variables. Comorbidity is a concept that encompasses the baseline diseases of patients, which usually increase with age,3–7 although this is not a constant. We know that the presence of comorbidities contributes to the situation of undertreatment in geriatric patients2 and that decisions are often made without an objective, quantitative assessment. It is thus necessary to objectively quantify the risk caused by comorbidities, and one of the scales used to determine this risk is the Charlson Index.8
The objectives of our study were to assess comorbidities with the Charlson Index in a population of senior patients who were surgically treated for colon cancer and to assess their influence on the postoperative results and survival of the patients.
Materials and MethodsWe carried out a retrospective study analyzing a patient sample that had undergone surgery for colon cancer at the General Surgery Unit of the Consorcio Hospitalario in Vic, Spain. The inclusion criteria for the study were being diagnosed with colon cancer at our center, age over 65, having had surgical treatment and adjuvant chemotherapy according to the established protocol, and having had medical follow-up for a minimum of 5 years after surgery. Excluded from the study were those patients with rectal cancer and those with colon cancer who had not been treated surgically. Finally, 115 patients who met these selection criteria were included from a total of 250 patients evaluated from the database. All patients had been diagnosed between 2003 and 2005, and the end date of the study was January 2010.
Calculating ComorbiditiesThe Charlson comorbidity index assesses baseline diseases and provides a prognosis index for patient survival. Each disease scores from 1 to 6 in the index, and the total sum determines a score that estimates the annual survival for the following 5 years. Since colon cancer defined our study cohort, we excluded this diagnosis from the index calculations.
For the comorbidity study, the patients’ prior clinical histories were extracted from their medical files. Three groups were defined according to the score of the index: no comorbidity score (0), low comorbidity score (1 or 2) and high comorbidity score (equal to or greater than 3).
Surgery and DiseaseThe patients were classified as having had either elective or emergency surgery. Emergency interventions were mostly performed for acute bowel obstruction. Colostomy and ileotransverse anastomoses were considered palliative techniques. The patients were staged with the TNM classification according to the final pathology report, findings during surgical intervention and test results.
Clinical EvolutionPostoperative variables were collected during hospitalization. Medical complications included respiratory (pneumonia, thromboembolism, and pneumothorax), cardiovascular (heart attack and acute pulmonary edema), nephrological (renal failure, retention, and urinary infection), bleeding ulcer and catheter sepsis. Surgical complications included wound infection, organ/space infection, evisceration, anastomotic leak, fistula, ileus and postoperative hemorrhage. Short-term (1-year) and long-term (5-year) mortalities were recorded from the outpatient follow-up data from office visits and regular telephone contact until the end of the study.
StatisticsAll patient variables are shown as means with standard deviation. The categorical variables were compared using the Chi-squared or Fisher's exact test. For the continuous variables, Student's t-test or ANOVA analysis was used. Kaplan–Meier survival curves were calculated for the comorbidity groups. Cox regression was used to calculate mortality ratios, and the group without comorbidities was the reference group. The crude ratios were adjusted for age and colon cancer stage. A P value of less than 0.05 was considered statistically significant. The SPSS version 15.0 was used for statistical analysis.
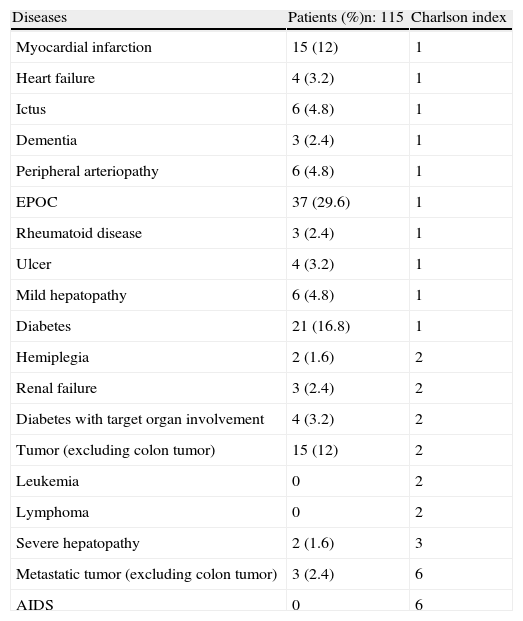
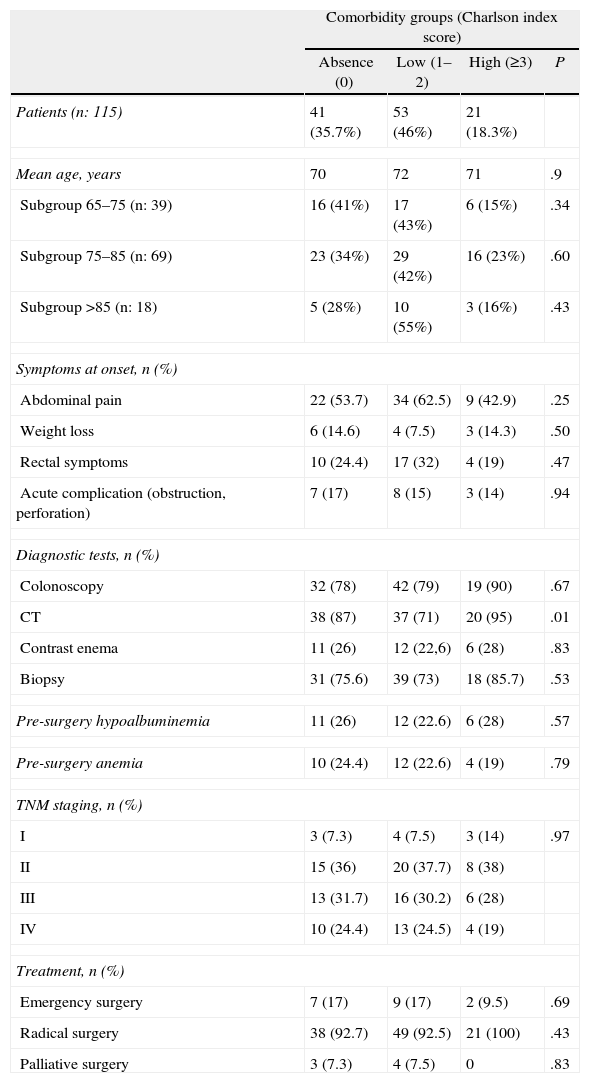
ResultsGeneral and by Comorbidity GroupOut of the 115 patients studied, 60% were men. Mean age was 78 (range 65–94). The most prevalent comorbidity was COPD (29.6%) (Table 1). The comparative characteristics of the comorbidity groups (Table 2) indicate that most patients were included in the group of low (46%) or no (35.7%) comorbidity. We found no correlation between age and comorbidity, with a similar distribution in the comorbidity groups among the different age ranges. Abdominal CT was used less frequently in the low comorbidity score group compared with the no- or high comorbidity score groups (71 vs 87 and 95% P=.01). No differences in distribution were observed regarding the presence of anemia (hematocrit <30%) or hypoalbuminemia (albumin <3). The overall distribution of the patients by cancer stage (I: 8.7%, II: 37.4%, III: 30.4%, IV: 23.5%) was similar between comorbidity groups.
Comorbidities of the Patients With Colon Cancer.
| Diseases | Patients (%)n: 115 | Charlson index |
| Myocardial infarction | 15 (12) | 1 |
| Heart failure | 4 (3.2) | 1 |
| Ictus | 6 (4.8) | 1 |
| Dementia | 3 (2.4) | 1 |
| Peripheral arteriopathy | 6 (4.8) | 1 |
| EPOC | 37 (29.6) | 1 |
| Rheumatoid disease | 3 (2.4) | 1 |
| Ulcer | 4 (3.2) | 1 |
| Mild hepatopathy | 6 (4.8) | 1 |
| Diabetes | 21 (16.8) | 1 |
| Hemiplegia | 2 (1.6) | 2 |
| Renal failure | 3 (2.4) | 2 |
| Diabetes with target organ involvement | 4 (3.2) | 2 |
| Tumor (excluding colon tumor) | 15 (12) | 2 |
| Leukemia | 0 | 2 |
| Lymphoma | 0 | 2 |
| Severe hepatopathy | 2 (1.6) | 3 |
| Metastatic tumor (excluding colon tumor) | 3 (2.4) | 6 |
| AIDS | 0 | 6 |
Comparative Characteristics of the Patients With Colonic Neoplasia According to Comorbidity Groups.
| Comorbidity groups (Charlson index score) | ||||
| Absence (0) | Low (1–2) | High (≥3) | P | |
| Patients (n: 115) | 41 (35.7%) | 53 (46%) | 21 (18.3%) | |
| Mean age, years | 70 | 72 | 71 | .9 |
| Subgroup 65–75 (n: 39) | 16 (41%) | 17 (43%) | 6 (15%) | .34 |
| Subgroup 75–85 (n: 69) | 23 (34%) | 29 (42%) | 16 (23%) | .60 |
| Subgroup >85 (n: 18) | 5 (28%) | 10 (55%) | 3 (16%) | .43 |
| Symptoms at onset, n (%) | ||||
| Abdominal pain | 22 (53.7) | 34 (62.5) | 9 (42.9) | .25 |
| Weight loss | 6 (14.6) | 4 (7.5) | 3 (14.3) | .50 |
| Rectal symptoms | 10 (24.4) | 17 (32) | 4 (19) | .47 |
| Acute complication (obstruction, perforation) | 7 (17) | 8 (15) | 3 (14) | .94 |
| Diagnostic tests, n (%) | ||||
| Colonoscopy | 32 (78) | 42 (79) | 19 (90) | .67 |
| CT | 38 (87) | 37 (71) | 20 (95) | .01 |
| Contrast enema | 11 (26) | 12 (22,6) | 6 (28) | .83 |
| Biopsy | 31 (75.6) | 39 (73) | 18 (85.7) | .53 |
| Pre-surgery hypoalbuminemia | 11 (26) | 12 (22.6) | 6 (28) | .57 |
| Pre-surgery anemia | 10 (24.4) | 12 (22.6) | 4 (19) | .79 |
| TNM staging, n (%) | ||||
| I | 3 (7.3) | 4 (7.5) | 3 (14) | .97 |
| II | 15 (36) | 20 (37.7) | 8 (38) | |
| III | 13 (31.7) | 16 (30.2) | 6 (28) | |
| IV | 10 (24.4) | 13 (24.5) | 4 (19) | |
| Treatment, n (%) | ||||
| Emergency surgery | 7 (17) | 9 (17) | 2 (9.5) | .69 |
| Radical surgery | 38 (92.7) | 49 (92.5) | 21 (100) | .43 |
| Palliative surgery | 3 (7.3) | 4 (7.5) | 0 | .83 |
As for surgical treatment, 108 patients (93.9%) underwent surgery with intended radical resection, and in 7 (6.1%) a palliative technique was performed. No differences were found with regards to baseline comorbidities. In all patients, open surgery by laparotomy was performed. Overall, 45 (39%) patients had right colon surgery, 51 (44.3%) left colon surgery, 13 (11.3%) Hartmann’ procedure and 6 (5.2%) palliative colostomy. A small percentage of patients (15%) were hospitalized for emergency surgery due to complications; no differences were observed between the comorbidity groups.
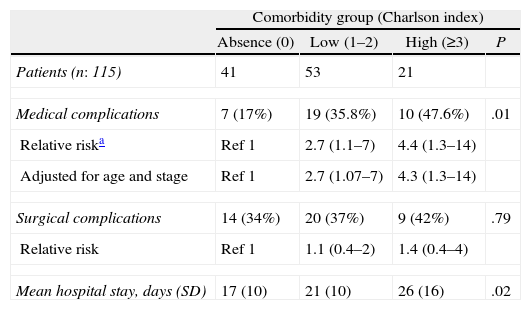
Postoperative ComplicationsThe results are shown in Table 3. Patients with some degree of comorbidity according to the Charlson Index (groups with low and high comorbidity scores) presented a higher rate of postoperative medical complications compared with patients without comorbidities (35.8 and 47.6 vs 17%, P=.01). The risk for medical complications was 2.7 and 4.4 times greater in the groups with low and high comorbidity scores, respectively. The most frequent medical complications were respiratory complications. To determine the influence of age and tumor stage on this risk, logistic regression was adjusted for these variables. We found that age and stage of the neoplasia were not confounding factors and that similar relative risks were maintained. No differences in postoperative surgical complications were found between the comorbidity groups (P=.6). The length of hospital stay was significantly longer in the group with high comorbidity scores compared with the no comorbidity group (17 days vs 26, P=.02).
Risk of Surgical and Medical Postoperative Complications in Patients With Colonic Neoplasia According to Comorbidity Groups.
| Comorbidity group (Charlson index) | ||||
| Absence (0) | Low (1–2) | High (≥3) | P | |
| Patients (n: 115) | 41 | 53 | 21 | |
| Medical complications | 7 (17%) | 19 (35.8%) | 10 (47.6%) | .01 |
| Relative riska | Ref 1 | 2.7 (1.1–7) | 4.4 (1.3–14) | |
| Adjusted for age and stage | Ref 1 | 2.7 (1.07–7) | 4.3 (1.3–14) | |
| Surgical complications | 14 (34%) | 20 (37%) | 9 (42%) | .79 |
| Relative risk | Ref 1 | 1.1 (0.4–2) | 1.4 (0.4–4) | |
| Mean hospital stay, days (SD) | 17 (10) | 21 (10) | 26 (16) | .02 |
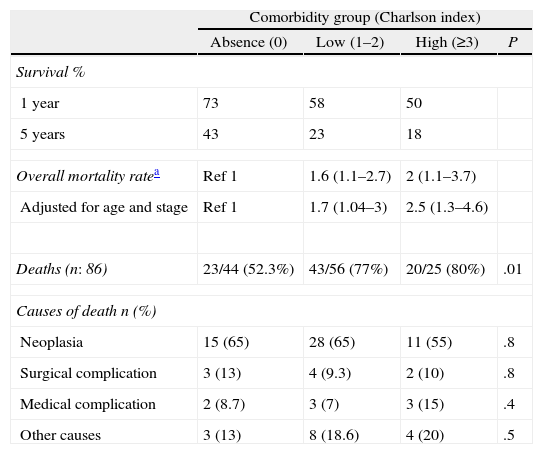
Regarding the overall mortality of the patient cohort, by the end of the study 86 patients had died (68.8%). There was a longer patient survival observed in the group with no comorbidities compared with the low and high comorbidity score groups, both in the first year (73 vs 58 and 50%, respectively; P=.01) as well as after 5 years of follow-up (43 vs 23 and 18%, respectively; P=.01) (Table 4). Higher mortality rates were found for patients with some degree of comorbidity compared with the patients with no comorbidities (RR 1.6 and 2, low and high comorbidity groups). Risk was adjusted for age and tumor stage, and significance of the elevated risk for mortality associated with the presence of comorbidities was maintained (RR 1.7 and 2.5, low and high comorbidity score groups) compared with the non-adjusted analysis. In the analysis of the causes of mortality, neoplasia was the most prevalent factor (62.7% of deaths). The second most frequent causes were unrelated to the neoplasia or postsurgical complications (30%); of these, re-exacerbation or evolution of chronic diseases as well as the natural aging process were the most common. The presence of comorbidities was not associated with a specific increase of any of the causes for mortality in our series of patients (Table 4).
Mortality in Patients With Colon Cancer According to Comorbidity Groups.
| Comorbidity group (Charlson index) | ||||
| Absence (0) | Low (1–2) | High (≥3) | P | |
| Survival % | ||||
| 1 year | 73 | 58 | 50 | |
| 5 years | 43 | 23 | 18 | |
| Overall mortality ratea | Ref 1 | 1.6 (1.1–2.7) | 2 (1.1–3.7) | |
| Adjusted for age and stage | Ref 1 | 1.7 (1.04–3) | 2.5 (1.3–4.6) | |
| Deaths (n: 86) | 23/44 (52.3%) | 43/56 (77%) | 20/25 (80%) | .01 |
| Causes of death n (%) | ||||
| Neoplasia | 15 (65) | 28 (65) | 11 (55) | .8 |
| Surgical complication | 3 (13) | 4 (9.3) | 2 (10) | .8 |
| Medical complication | 2 (8.7) | 3 (7) | 3 (15) | .4 |
| Other causes | 3 (13) | 8 (18.6) | 4 (20) | .5 |
First of all, we should comment that we have not observed high comorbidity scores among the patients of our geriatric cohort. Previously reported studies with a high number of patients show that comorbidities increase with age.3–7 In our cohort, however, we have not found this relationship. To explain this, we admit a probable selection bias because the senior patients who have been diagnosed in other departments of our hospital and referred to us for surgical treatment are already partially selected as being considered operable and having few comorbidities. Similar to the age factor, no stage of neoplasm has been related with higher comorbidity scores, although there was a tendency of the group of patients with high comorbidity scores (group 3) to be diagnosed in initial stages (14% of patients in stage i); the reason for this may be the closer relationship of these patients with the healthcare system, which would increase the possibility of diagnosis. As for the need for emergency surgery, some studies demonstrate that this increases hand in hand with an increase in comorbidities6,7; there would logically be complications of acute colon cancer in situations with infection, perforation, in patients with digestive atheromatous vascular disease or immunosuppression. In any case, this relationship was not observed in our patients, taking into account that the most frequent comorbidities were respiratory. Palliative surgical treatment was also not higher in the group with greater comorbidity scores (Charlson 3). We believe that this fact is more closely related to the equal distribution of advanced neoplastic stages between comorbidity groups. Therefore, we have not found any clinical variables in our sample of geriatric patients who had undergone surgery for colon cancer that are related with a higher comorbidity score according to the Charlson Index.
We will now comment on the influence of comorbidities on the postsurgical period and survival. The presence of one or more points on the Charlson Index practically triples the probabilities for postoperative medical complications. These results are in line with what has been published in the literature. Some authors have shown evidence that the types of morbidities that are most often independent risk factors are vascular, respiratory and neurological.1 The first consequence of the increase in postsurgical medical complications is the prolonged hospitalization that we have observed in patients with a Charlson Index above 3 points. The group at high-risk for medical complications has a hospitalization period that is practically double the hospitalization period for patients without preoperative comorbidities. Correct pre- and post-surgery medical support (centered on the chronic medical diseases of the patient), clinical monitoring, and the correct administration of baseline pharmacological treatments (established according to the specific protocols for each entity) are essential to avoid decompensation as well as to theoretically influence hospital stay duration.
As for the overall mortality of the patients, we have observed how the presence of a degree of comorbidity measured by the Charlson Index entails an increase in mortality in the short and long term that is practically double that of patients without comorbidities. In a recent study with almost 90000 patients,1 respiratory comorbidities increased short-term perioperative mortality (OR=3.1). Other studies9–12 that objectively evaluate comorbidity with the Charlson Index also confirm its validity as a short- and long-term predictor for mortality in patients who undergo colon cancer surgery. We currently know that the other variables that influence and increase mortality after colon cancer surgery are age above 65–70 (OR=3.2),1 malnutrition prior to surgery (OR=1.3), presence of metastasis (OR=3), the need for emergency surgery (OR=2.6) and the use of laparotomy over laparoscopy.13
We should insist on the importance of nutritional state and surgical technique, because laparoscopic colectomy reduces perioperative mortality (OR=0.5).13 Furthermore, the use of a comorbidity index such as Charlson's independently stratifies the risk for complications of patients with colon cancer, which helps make a more objective decision when contemplating surgical treatment in senior patients. We believe that this would have an impact on the undertreatment of some patients, especially those in the geriatric group, who are rejected due to age even when they present no associated comorbidities. We will also be able to better identify patients who are not ideal candidates for surgical treatment due to their very high risk; these patients could be those in the high comorbidity subgroup (Charlson Index, 3 or more points). With the current lack of prospective studies, future clinical studies on colon cancer treatment in geriatric patients should include an objective evaluation of comorbidities.
The main limitation of the present study is that the patient series is small and larger cohort studies may not support our results.
In summary, the presence of some degree of comorbidity as measured by the Charlson Index is an independent predictor for medical complications and increased overall mortality in senior patients who undergo surgery for colon cancer.
Conflict of InterestsThe authors declare having no conflict of interests.
Please cite this article as: Medarde-Ferrer M, Serra-Genís C, Roca J, Quer X, Sala F, Palau MA, et al. Evaluación objetiva del grado de comorbilidad en pacientes geriátricos con neoplasia de colon: relación con los resultados quirúrgicos y la supervivencia. Cir Esp. 2013;91:231–236.