Non-surgical spontaneous pneumoperitoneum represents 10% of cases described in the literature.1–8 It is difficult to diagnose and responds to conservative management, which reduces iatrogenesis.1,2,4–7
We present the case of a 46-year-old male with no history of interest, who came to the emergency department due to dyspnea and a fever of 39 °C. He was diagnosed with bilateral viral pneumonia due to COVID-19 infection (positive nasopharyngeal polymerase chain reaction [PCR]). The patient was hospitalized, and in the first 48 h he developed severe global respiratory failure and was transferred to the ICU, requiring mechanical ventilation (MV) in IPPV mode with FiO2 0.6, PEEP 14 cmH2O, 480 mL × 24 bpm. On the 7th day of the ICU stay, he required tracheostomy. The patient received antibiotic treatment with azithromycin and hydroxychloroquine, later in association with meropenem and cefazoline due to suspected bacterial superinfection. High-dose corticosteroid therapy was also administered.
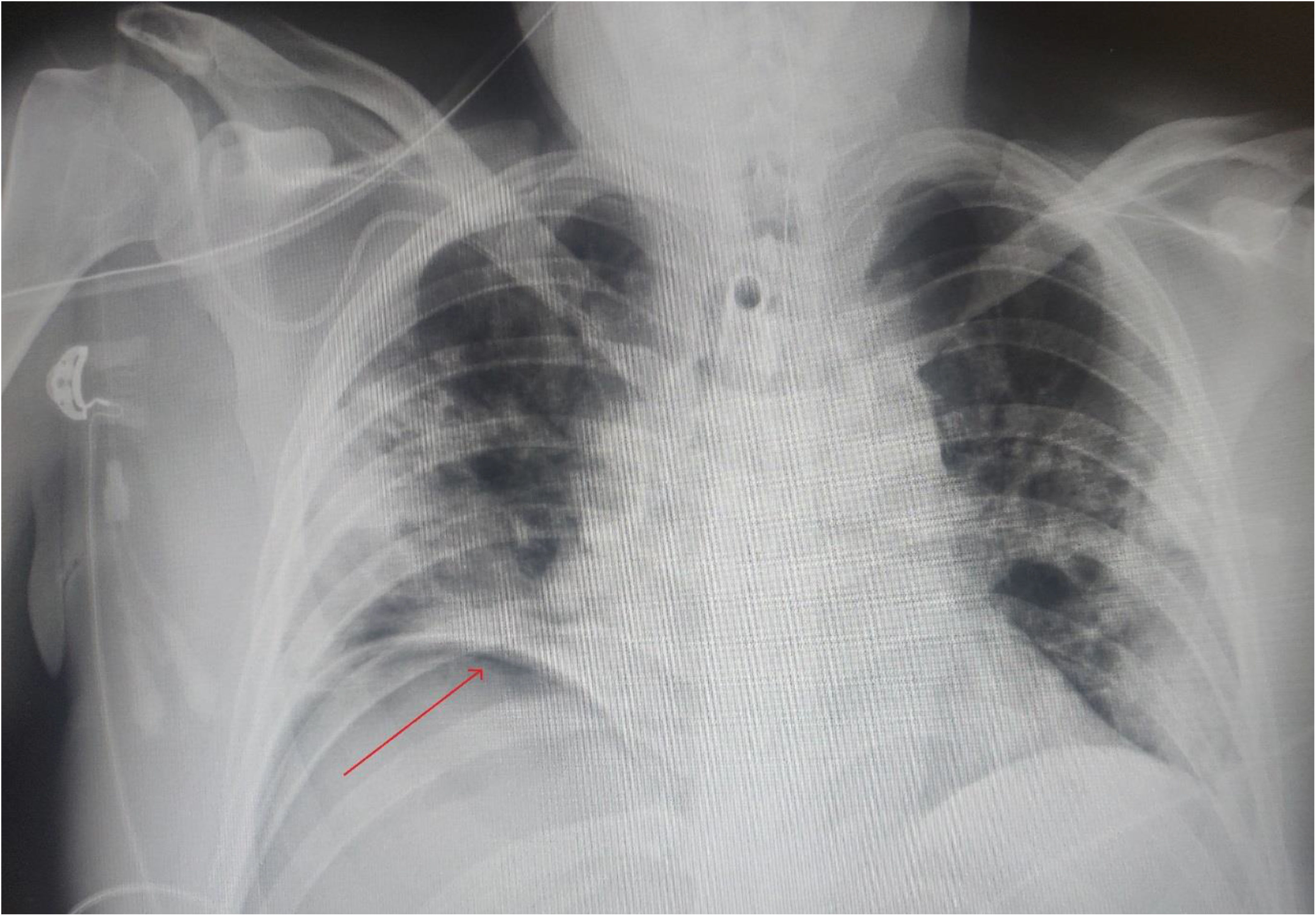
On the 16th day of the ICU stay, the patient was disconnected from MV after improved respiratory condition. The follow-up chest X-ray detected right subdiaphragmatic pneumoperitoneum (Fig. 1), at which time we were called in for consultation. Analytically, compared to the previous day, a significant drop in leucocytes was observed (from 27 000 to 17 000 μ/L), as well as in C-reactive protein (from 256 to 84 mg/L). Transaminases continued to be elevated, but with a clear descending pattern (ALT: 171 IU/L; AST: 52 IU/L). Procalcitonin: 0.04 ng/mL. The patient was asymptomatic from an abdominal standpoint. Intestinal transit was maintained, with no fever or associated symptoms.
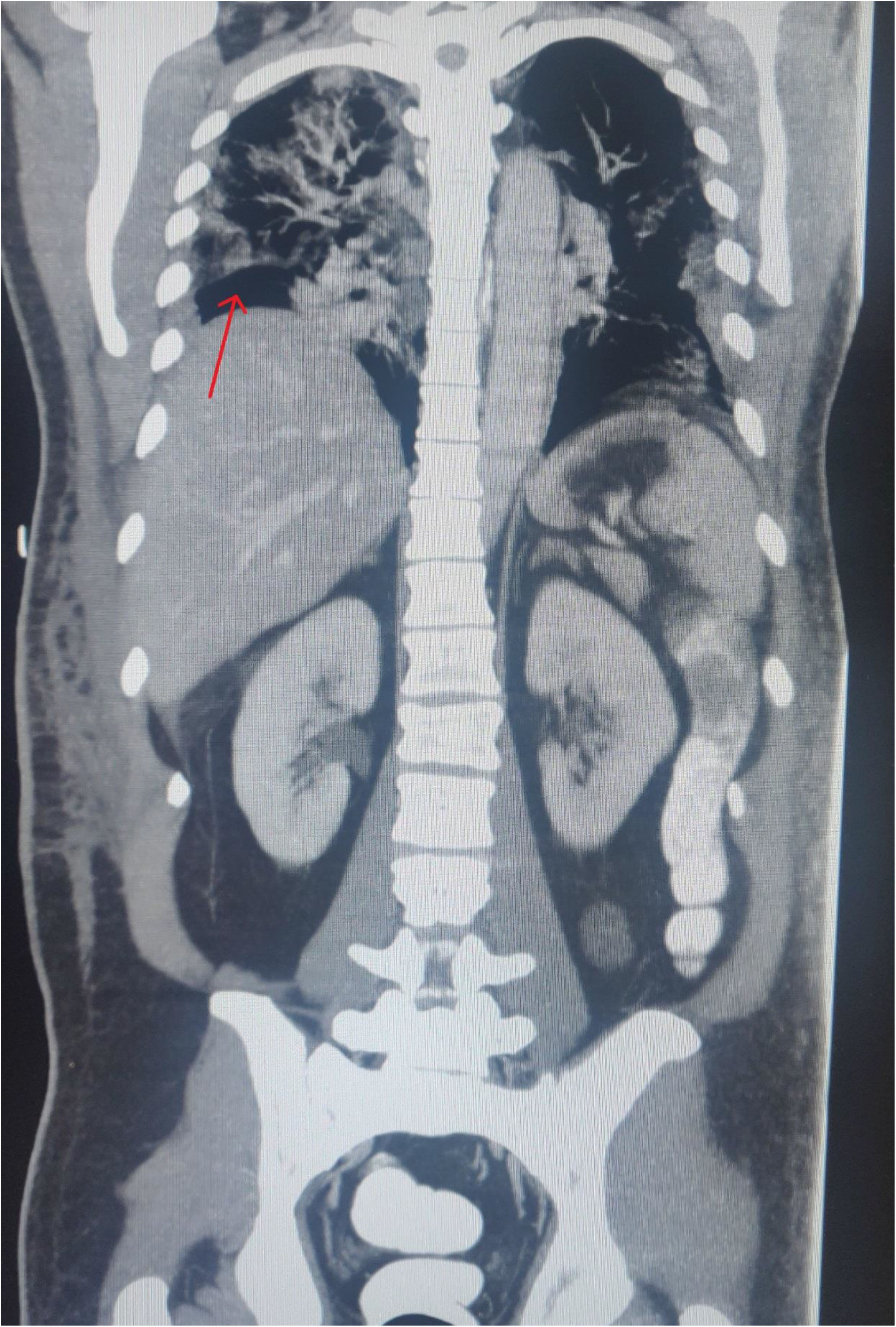
Thoracoabdominal CT scan was performed with intravenous contrast, with a nasogastric tube and rectally. Confluent patchy multifocal opacities were observed in both lungs, predominantly peripheral, as well as consolidations of posterior and baseline predominance with air bronchogram related to known viral pneumonia due to COVID-19. In the abdomen, abundant pneumoperitoneum with contrast filling was observed in the entire colon and small bowel loops, with no leakage. This was associated with a minimal amount of free abdominal fluid, but no areas of fat rarefaction suggesting inflammatory involvement, as well as multiple reactive abdominal lymphadenopathies (Fig. 2).
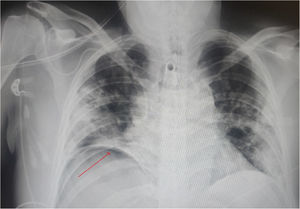
Given these findings, the diagnosis was non-surgical spontaneous pneumoperitoneum, and we decided to manage the patient conservatively. Twenty-four hours after diagnosis, the patient was still asymptomatic from an abdominal standpoint and showed progressive reduction in acute-phase reactants. Oral intake was therefore initiated, and the patient was moved to the ward 21 days after admission to the ICU. He continued to show progressive respiratory improvement and had no relevant abdominal symptoms during his stay in the hospital. The patient was discharged 43 days after admission.
We carried out a systematic search without limits in PubMed, using the following strategy: (Pneumoperitoneum) AND ((Covid 19) OR (Covid-19) OR (Coronavirus Covid-19) OR (Covid) OR (Coronavirus) OR (Covid 19 symptoms)), on April 15, 2020. Only one published article was found that was not the subject of the current study.
Intestinal perforation is the cause of 90% of cases of pneumoperitoneum.1–6,8 However, the remaining 10% encompass spontaneous pneumoperitoneum that could be managed conservatively, which represents a clear reduction in iatrogenesis.1–3 In 1977, Gantt et al. classified non-surgical pneumoperitoneum as having thoracic, abdominal, gynecological or iatrogenic origins.1,5 Thoracic causes rank second, behind abdominal causes (cystic intestinal pneumatosis and endoscopic procedures).3,6,8 One of the most frequent causes of thoracic origin is MV, due to the barotrauma that occurs as a consequence of positive pressure.2 This causes the subcortical and perivascular alveoli to rupture, so air passes into the abdominal cavity either through the diaphragm or mediastinum.1,6 For this reason, it is sometimes associated with pneumomediastinum, subcutaneous emphysema, and retropneumoperitoneum.6
The diagnosis of non-surgical spontaneous pneumoperitoneum is highly controversial and is a dilemma for the surgeon, especially when abdominal symptoms are uncertain. Therefore, the diagnosis of this entity requires adequate clinical, radiological and analytical evaluation.1,4,7 The patient is required to be asymptomatic or paucisymptomatic from an abdominal perspective, together with non-elevated or diminishing acute-phase reactants and radiological tests that rule out an associated complication. It is recommended to perform CT scan with oral and rectal contrast in order to complete the information. If there are discrepancies between these three factors, it is advisable to perform an exploratory laparotomy.1,2,7,9
The diagnostic suspicion of this entity is essential because it reduces the number of unnecessary laparotomies.6 As Lei et al.10 have recently published in China, scheduled surgery in positive COVID-19 patients considerably increased the exacerbation of symptoms, with the consequent increase in morbidity and mortality (20.5%). In our case of a serious patient in recent recovery from respiratory distress syndrome, urgent laparotomy could have been fatal without achieving any therapeutic progress. Because patients with COVID-19 infection may require prolonged periods of MV at high pressures, this is a situation that we may encounter more frequently in the coming months due to the increase in intubated patients in Spanish ICUs with COVID-19.
FundingThis case report has required no funding from any organization.
Conflict of interestThe authors have no conflict of interests to declare.
Please cite this article as: Gemio del Rey IA, de la Plaza Llamas R, Ramia JM, Medina Velasco AA, Díaz Candelas DA. Neumoperitoneo espontáneo no quirúrgico en paciente COVID-19 positivo con neumonía bilateral severa. Cir Esp. 2021;99:469–471.