The COVID-19 pandemic has had a significant impact on Spanish hospitals, which have had to allocate all available resources to treat these patients, reducing the ability to attend other common pathologies. The aim of this study is to analyze how the treatment of acute appendicitis has been affected.
MethodA national descriptive study was carried out by an online voluntary specific questionnaire with Google Drive™ distributed by email by the Spanish Association of Surgeons (AEC) to all affiliated surgeons currently working in Spain (5203), opened from April 14th to April 24th.
ResultsWe received 337 responses from 170 centers. During the first month of the pandemic, the incidence of acute appendicitis decreased. Although conservative management increased, the surgical option has been the most used in both simple and complicated appendicitis. Despite the fact that the laparoscopic approach continues to be the most widely used in our services, the open approach has increased during this pandemic period.
ConclusionHighlight the contribution of this study in terms of knowledge of the status of the treatment of acute appendicitis during this first month of the pandemic, being able to serve for a better possible organization in future waves of the pandemic and a reorganization of current protocols and management of acute appendicitis in a pandemic situation.
La pandemia por COVID-19 ha tenido una importante repercusión en los hospitales españoles, que han tenido que destinar todos los recursos disponibles al tratamiento de estos pacientes, reduciendo la capacidad de atender otras enfermedades habituales. Este estudio pretende analizar cómo se ha visto afectado el tratamiento de la apendicitis aguda.
MétodoSe ha realizado un estudio nacional descriptivo mediante una encuesta online voluntaria, realizada en Google Drive™ distribuida por correo electrónico por la Asociación Española de Cirujanos (AEC) a todos los cirujanos miembros en activo (5.203) del 14 de abril al 24 de abril del 2020.
ResultadosSe han recibido 337 respuestas de 170 centros nacionales. Durante el primer mes de la pandemia, ha disminuido la incidencia de apendicitis aguda. La opción quirúrgica ha sido la más utilizada tanto en cuadros simples como en complicados, aunque el manejo conservador se ha incrementado. A pesar de que el abordaje laparoscópico sigue siendo el más utilizado en nuestros hospitales, la vía abierta ha presentado un incremento durante esta pandemia.
ConclusiónResaltar la aportación este estudio en cuanto conocimiento del estado del tratamiento de la apendicitis aguda durante este primer mes de pandemia, pudiendo servir para una posible mejor organización en próximas olas de la pandemia y a un replanteamiento de los protocolos actuales y manejo de la apendicitis aguda en caso de pandemia.
In 2019, coronavirus-19 disease (COVID-19) emerged as an outbreak caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). As of April 20, 2020, the disease had spread to 213 countries around the world, with 2 285 210 confirmed cases and more than 155 124 deaths.1 In surgical patients, it has been argued that surgery can accelerate and exacerbate the progression of COVID-19,2 which is why several surgical societies around the world have made a series of recommendations, including for urgent surgery.3,4 In this pandemic situation, surgeons have faced the dilemma of treating urgent surgical diseases, optimizing available resources, and assuming the possible consequences of delayed treatment.4,5
In Spain, according to the registry of the Ministry of Health, Consumption and Social Welfare, 44 168 patients were treated for acute appendicitis in 2017, which represents a crude rate of 9.51/10 000 inhabitants (10.78 when adjusted for age) and an average of 3681 cases of appendicitis per month.5 From these data, we can extrapolate that the incidence of appendicitis during the 2 months of home confinement would be about 7362 cases nationwide that should have been seen in emergency departments. Based on these estimations, we feel that it essential to know how the state of alarm has affected decision-making in the treatment of patients with acute appendicitis. The main objective of this study is to identify the treatment strategies used for patients with acute appendicitis in Spain during the first month of the COVID-19 pandemic.
MethodsWe have conducted a descriptive study with data from 337 surveys, completed by surgeons from 170 Spanish hospitals, regarding the diagnostic and therapeutic management of acute appendicitis during the first month of the COVID-19 pandemic in Spain. The first month of the pandemic started when the ‘state of alarm’ was declared on March 14, 2020 and ended April 14, 2020. That very same day (April 14, 2020), the Spanish Association of Surgeons (AEC) e-mailed a voluntary online survey to all its members (5203) at Spanish medical centers, which remained accessible until April 24th. One reminder was sent per week. The questionnaire consisted of 25 questions and was designed on the online Google Drive™ platform (Alphabet Co, Mountain View, CA). The questions were aimed at evaluating demographic data, settings, safety in the operating room, and changes in the treatment of patients with acute appendicitis during the pandemic versus pre-pandemic management (Appendix 2).
Data managementQuestions and answers were downloaded, then analyzed and discussed by all members of the group. Once the response period had ended, we reviewed the surveys manually in order to filter out multiple entries from the same individual and responses from foreign hospitals. Responses from the same medical center were also analyzed to rule out possible disparate responses.
Statistical analysisCategorical variables were reported by total counts and percentages. Responses to survey questions both before and during the pandemic were compared using the McNemar test. Differences were considered statistically significant when the P-value was <.05. The statistical package used to perform the analyses was the R 3.6.2 (R Core Team, 2019. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/. https://www.R-project.org/) together with the ‘R companion’ library (R package version 2.3.25.).
ResultsGeneral dataThe survey was sent to the 5203 members of the AEC, and 357 completed responses were received. When we applied the exclusion criteria, 8 responses were eliminated due to double responses, and 12 were excluded because the members practiced outside the scope of the national healthcare system. The analyzed responses were received from 337 surgeons from 170 Spanish national medical centers. Fig. 1 demonstrates the national distribution of the responses by hospitals and regions of Spain. The demographic data of the surgeons analyzed are included in Table 1.
General characteristics of the sample.
| Questions | Options | Distribution (%) |
|---|---|---|
| Professional category | Resident | 22.5 |
| Surgeon | 77.5 | |
| Years since you finished residency | <5 | 24.3 |
| 5−10 | 22.8 | |
| >10 | 52.9 | |
| How many times have you been on call in the last month (March 13 – April 13, 2020) during the pandemic? | <2 | 5,4 |
| 3−5 | 51.9 | |
| >5 | 42.7 | |
| Type of hospital | Public university | 66.7 |
| Private university | 4.2 | |
| Public | 17.5 | |
| Public, under private management | 6.2 | |
| Private | 4,5 | |
| Other | 0,9 | |
| During the COVID-19 pandemic, how has the organization of your hospital changed? | Restricted areas dedicated to patients with COVID-19 | 92 |
| Exclusively COVID-19 patients | 7.4 | |
| My hospital does not treat COVID-19 patients | 0.6 | |
| AEC scenarios | I | 1.5 |
| II | 16.8 | |
| III | 37.8 | |
| IV | 29.7 | |
| V | 14.2 | |
The Surgery-AEC-COVID-19 working group has recently described a series of alert phases that reflect possible scenarios during the COVID-19 epidemic.6 The responses to our survey reflect that the hospitals where the surgeons who answered the survey practice worked mainly in a medium-alert scenario (III) (37.8%), followed by a high-alert scenario (IV) (29.7%). It should be noted that 16.8% of the participants worked in a low-alert epidemiological scenario, but 14.2% worked in an emergency-type scenario (V) (Table 1).
Incidence and treatment: surgical management (SM) versus conservative management (CM) and approach typeWhen we analyzed the monthly incidence of acute appendicitis, we observed that, before the pandemic, 10−20 cases of appendicitis were treated in 43% of the responses, and more than 20 cases in 27.4%. This pressure decreased during the first month of the pandemic, and most participants reported 5−10 cases per month (37.4%), while 31% reported less than 5 cases (P < .0001). Before the pandemic, CM was only used in 10.5% of patients with uncomplicated acute appendicitis (range 1%–25%). With the arrival of the virus, an increase in CM is observed, although the majority continue to opt for SM (75.1% of the responses). 19.2% opted for CM of 1%–25% of these cases treated. In the case of uncomplicated acute appendicitis, 2.7% of respondents opted for CM of most appendicitis (76%–100% of cases). Regarding complicated acute appendicitis with abscess, this increase in CM has also become evident (11.8% during the pandemic versus 4.8% previously), although the SM option was most commonly chosen in both (74% during the pandemic versus 83.5% prior to it). In the treatment of uncomplicated and complicated acute appendicitis before and after the epidemic situation, statistically significant differences were observed (P < .0001).
As for the appendectomy approach, we observed that the open approach was used in less than 25% of the cases treated in 85.4% prior to the pandemic, compared to 64.8% during confinement. Although the open approach was a minority option during the pandemic, it has been used more than previously (P < .0001) (Table 2).
Presentation and management of acute appendicitis before and during the COVID-19 pandemic.
| Question | Options | Before COVID-19 | During COVID-19 | McNemar |
|---|---|---|---|---|
| P value | ||||
| How many patients with acute appendicitis were treated in one month? | < 5 | 4.5% | 31% | |
| P < .0001 | ||||
| 5−10 | 25.1% | 37.4% | ||
| 10−20 | 43% | 25% | ||
| >20 | 27.4% | 6.6% | ||
| What percentage of patients with non-complicated acute appendicitis (no abscess) were treated conservatively with antibiotics at your hospital? | 0% | 88.3% | 75.1% | |
| P < .0001 | ||||
| 1−25% | 10.5% | 19.2% | ||
| 26−50% | 0.6% | 2.1% | ||
| 51−75% | 0.3% | 0.9% | ||
| >75% | 0.3% | |||
| 2.7% | ||||
| What percentage of patients with complicated acute appendicitis (with abscess) were treated conservatively with antibiotics ± percutaneous drainage at your hospital? | <25%% | 83.5% | 74% | |
| P < .0001 | ||||
| 26−50% | 6.6% | 10.9% | ||
| 51−75% | 5.1% | 3.3% | ||
| >75% | 4.8% | 11.8% | ||
| What percentage of patients with acute appendicitis treated surgically underwent open appendicectomy at your hospital? | <25% | 85.4% | 64.8% | |
| P < .0001 | ||||
| 26−50% | 10.5% | 11.3% | ||
| 51−75% | 2.6% | 12.2% | ||
| >75% | 1.5% | 11.7% | ||
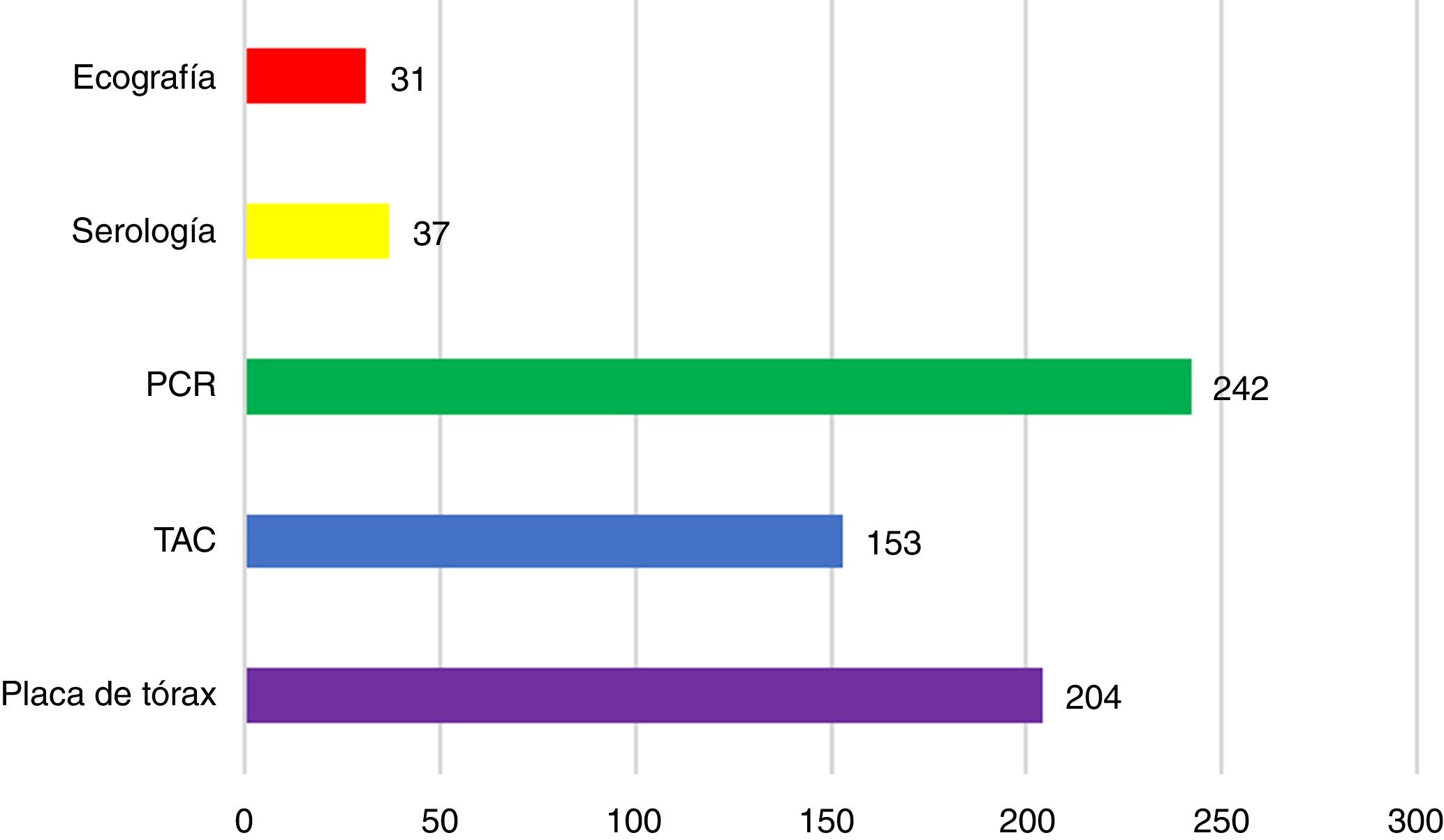
Half of the respondents (50.6%) answered that all patients with acute appendicitis were evaluated for SARS-CoV-2 infection prior to surgery. However, 42.1% only ordered preoperative tests in patients with respiratory symptoms or suspected infection, and 7.3% of survey participants stated that they did not order any type of test. Most surgeons who reported using some type of preoperative test for SARS-CoV-2 infection in patients with acute appendicitis before surgery opted for PCR (242 responses; Fig. 2).
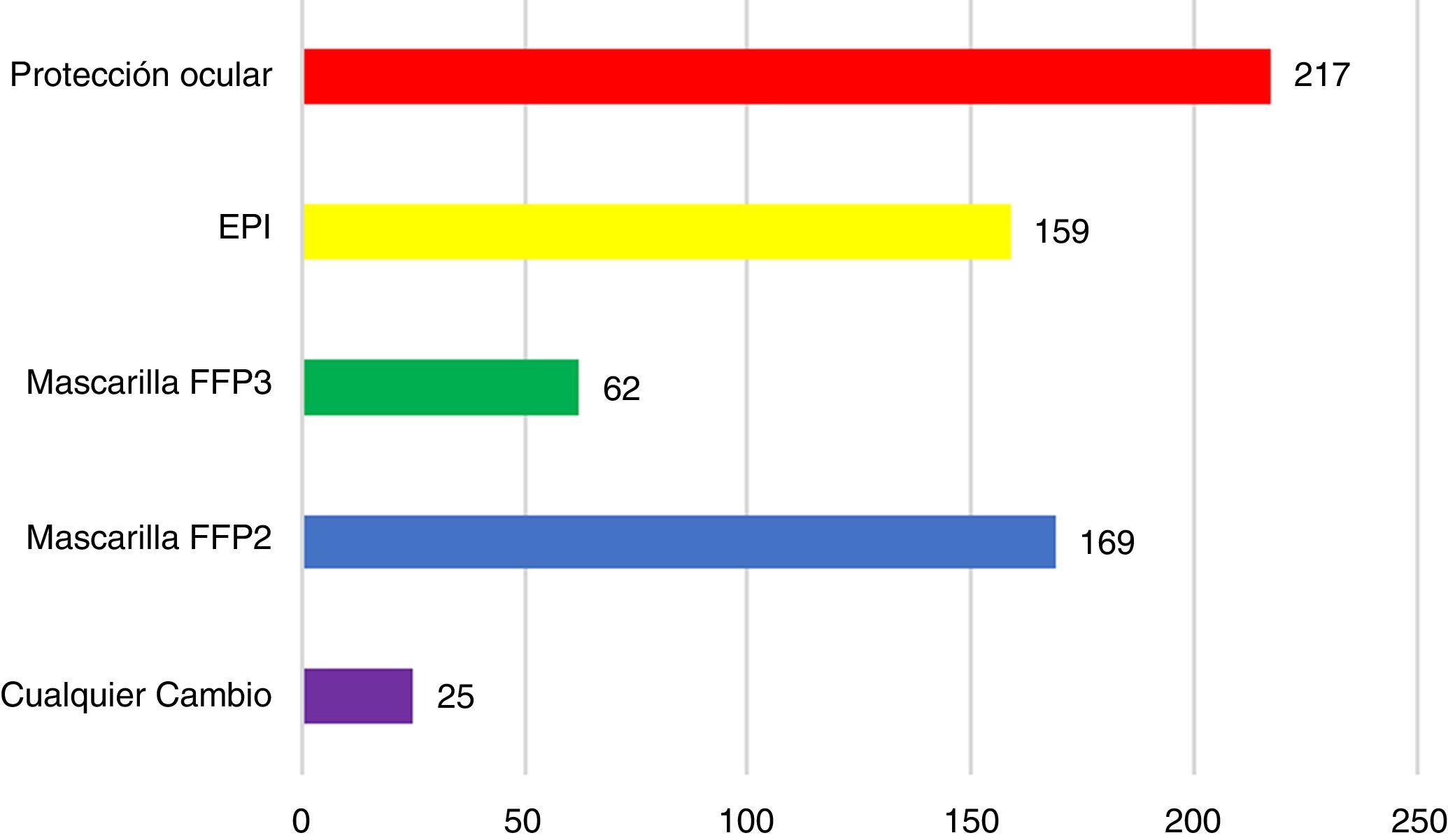
SafetyIn terms of establishing safe pathways for patients, one operating room was used exclusively for patients with suspected or confirmed COVID-19 infection in 79.6% of the responses. Meanwhile, 89.6% of the surgeons had modified their personal protection equipment. Eye protection systems were the most used in 217 responses, followed by FFP2 masks in 169 responses (Fig. 3).
According to our survey, 40.6% of surgeons do not believe that the laparoscopic approach poses a greater risk for infection. Specific devices for filtering surgical aerosols/smoke were used in 74.3% of laparoscopic surgeries performed during the pandemic. In most cases where a smoke filtration system is used, it consists of a respiratory filter connected to a water seal in 44.4%, followed by an air seal in 22.2% (Table 3).
Operating room safety.
| Questions | Options | Distribution (%) |
|---|---|---|
| Is there an independent operating room used exclusively for patients with suspected or confirmed COVID-19? | Yes | 79.6 |
| No | 20.4 | |
| Did you modify your personal protective equipment during any surgery? | Yes | 89.6 |
| No | 10.4 | |
| Do you believe that the laparoscopic approach entails higher risk of infection of operating room staff? | Yes | 30.8 |
| No | 40.6 | |
| No lo sé | 28.6 | |
| Did you use any type of filtration system for surgical smoke/gas? | Yes | 74.3 |
| No | 25.7 | |
| What type of device was used? | AirSeal | 22.2 |
| Respiratory filter | 21.8 | |
| Respiratory filter connected to a water-seal | 44.4 | |
| Other | 11.6 | |
In 23 responses (7%), postoperative COVID-19 infection was confirmed as a complication after appendectomy.
DiscussionSurgeons have faced many challenges during the SARS-CoV-2 pandemic. Foremost, they have continued to treat patients with urgent illnesses whose gold standard of treatment continues to be surgery. It is important to highlight that the recently published WSES Guidelines for the treatment of acute appendicitis7 indicates that antibiotic treatment can be considered an effective and safe strategy in selected patients with uncomplicated disease, although the risk of recurrence in the following 5 years may reach 39%. The presence of an appendicolith was also shown to be an independent predictor of perforation and failure of conservative treatment in uncomplicated appendicitis.8 Furthermore, the risk of failure of antibiotic treatment during the first hospitalization is 8%, and an additional 20% may require re-hospitalization for appendicitis within the first year.8
In the current epidemiological context, a patient with acute appendicitis may have a diagnosis of SARS-CoV-2 infection, may have already recovered from the disease, or may be in the incubation period or be an asymptomatic carrier. Likewise, it is possible that the patient consulting for appendicitis has not had contact with the virus and that going to the hospital poses a risk of exposure. This, coupled with the fear of hospital infection and the state of lockdown, may mean that a patient with abdominal pain decides to wait before coming to the emergency room, and we may therefore be facing advanced surgical disease. This would explain the results obtained, which show that the majority of Spanish hospitals treated more than 10 cases of appendicitis per month (and nearly 28% of these treated more than 20 cases), but this number has decreased significantly during the first month of the pandemic, during which more than 68% of hospitals have treated fewer than 10 cases and almost half of them less than 5.
Second, before deciding whether to operate, surgeons must consider that the risk of complications and perioperative mortality in a patient infected by SARS-CoV-2 may be high.3 Moreover, operating on an infected patient entails the potential exposure of the entire surgical team.
Meanwhile, conservative treatment usually involves longer hospital stay and could pose a greater risk of in-hospital infection. This is reflected in the results, since, before the declaration of a pandemic, the majority of participating surgeons (88.3%) did not use CM in uncomplicated appendicular disease. Even though the majority still opted for surgical treatment in uncomplicated appendicitis during the first month of the COVID-19 pandemic, this percentage has dropped to 75.1%, perhaps due to patients being infected, or to reduce the inherent risk of major complications or possible infections. This would also explain why, in acute appendicitis complicated with abscesses, the use of conservative management (previously 4.8%) has increased to 11.8%. However, it should be noted that surgical treatment has been predominant in both scenarios, possibly because it tends to involve earlier resolution of the condition and earlier discharge from hospital, which is why it has been the preferred option in both epidemiological contexts.
In terms of the surgical approach, a possible increased risk of infection has been suggested9 with the use of laparoscopy due to the pneumoperitoneum and the potential aerosolization of the virus, although this risk has not been later documented.10–13 Perhaps due to the theoretical potential for aerosolization, an increase in open surgery has been observed, although most participating surgeons continued to use the laparoscopic approach (Table 2). In a previous scenario, the recommendation for the approach of complicated and uncomplicated appendicitis was laparoscopic surgery, since it represents advantages over open appendectomy in several aspects, including hospital stay,7 which is of great importance when we consider the current high hospital occupancy rates. Also, 40.6% of the surgeons who completed the survey do not believe that the laparoscopic approach poses a greater risk of infection for the operating room staff. Regardless, 74% use a smoke filtering system during laparoscopy, the most common of which is a respiratory filter connected to a water seal. The recommendations of the AEC for laparoscopic surgery include: filter the released CO2 with filtration devices; work with the lowest possible pneumoperitoneum pressure; avoid prolonged Trendelenburg position; limit the use of continuous energy sources; minimize the interchange of laparoscopic instruments; and, thoroughly suction the pneumoperitoneum before removing the trocars.12
In the absence of evidence, the preoperative diagnostic guidelines have varied depending on the region, the setting where the treatment was carried out, and even among hospitals within each geographical area, although there seems to be general agreement in considering all patients as suspicious of infection.14 This would explain the differences between responses, where only half of the surgeons (50.6%) declared that they systematically ordered COVID-19 testing for all patients prior to surgery, which in most cases involved PCR. Of the remainder, it is striking that more than 7% have ordered no preoperative tests. The importance of preoperative screening in patients requiring surgery was evident in our series, as 7% of patients operated on for appendicitis developed postoperative complications related with COVID-19 infection. Currently, the AEC recommends preoperative screening for all patients with urgent surgical disease.12 This may explain why the approach of surgeons at the time of surgery has been modified in terms of personal protection in almost 90% of cases, in which the use of eye protections and high-filtration FFP2 masks has increased. Special attention should be given to patients who become infected while hospitalized, as these patients are initially identified as negative and therefore remain on ‘clean’ floors for a time, thereby exposing others to possible infection until the respiratory symptoms become evident. Hence the importance of defining and identifying safe hospital circuits and minimizing in-hospital infection.13 After analyzing our results, we have observed that these circuits exist in most cases (79.6%). National (COVID-19 AEC) and international (COVIDSURG) multicenter studies will provide the actual risk of complications in cases of postoperative COVID-19 infection.
Our study has limitations because the data have been drawn from a survey and must be interpreted with caution. Another possible limitation is that some responses came from surgeons working at the same hospital, but, as previously explained, these responses were specifically analyzed to rule out disparate responses. Lastly, another possible limitation of our study is that we do not know the exact number of hospitals to which this survey was sent.
In conclusion, during the first month of the pandemic, the number of patients treated for acute appendicitis decreased. Regarding treatment, the surgical option was most frequently used in both simple and complicated cases, although conservative management has increased during this period. Although the laparoscopic approach continues to be the most commonly used in Spanish surgical units, the use of the open approach increased during the pandemic compared to the period prior to COVID-19. We emphasize the contribution of this study in terms of knowledge of the status of acute appendicitis treatment during the first month of the pandemic, which may possibly serve to better organize our approach to future waves of the pandemic and to rethink current protocols for the management of acute appendicitis in a pandemic event.
Conflict of interestsThe authors have no conflict of interests to declare in the preparation of this manuscript.
The names of all collaborators are listed in Addendum 1.
Please cite this article as: Prieto M, Ielpo B, Jiménez Fuertes M, González Sánchez MdC, Martín Antona E, Balibrea JM, et al. Encuesta nacional sobre el tratamiento de la apendicitis aguda en España durante la fase inicial de la pandemia por COVID-19. Cir Esp. 2021;99:450–456.